Videoconference-resiliency Intervention Successfully Targets Health-related Anxiety in Adults With Congenital Heart Disease
In This Article
- Researchers in the Department of Cardiology at Massachusetts General Hospital developed a mind-body intervention to improve resiliency in patients with chronic medical conditions that can be delivered via synchronous group videoconferencing
- The Stress Management and Resiliency Training Program-Relaxation Response Resiliency Program (SMART-3RP) is an 8-week group intervention with sessions lasting 1.5 hours each
- The intervention combines mind-body medicine, cognitive behavioral therapy, and positive psychology skills to improve stress coping and enhance resiliency
- In a randomized pilot feasibility trial, the researchers explored acceptability of videoconference-delivered SMART-3RP for adults with congenital heart disease (ACHD), who often experience increased health anxiety when compared with the general population
- The results revealed quantitative and qualitative improvements in patient experience and positive psychological change
Adults with congenital heart disease (ACHD) often experience increased health anxiety when compared with the general population. Health anxiety involves a high level of worrying about an individual's health, physical symptoms, and maladaptive behaviors including excessively scanning the body for signs of illness or avoiding activities that may trigger anxiety, such as physical activity and medical tests (Behavior Therapy). These anxiety symptoms are also associated with poor cardiac health outcomes, including physical inactivity (International Journal of Behavioral Medicine), medication non-adherence (Journal of Psychosomatic Research), elevated blood pressure (Psychology, Health & Medicine), lower quality of life (Cardiology in the Young & Current Opinion in Cardiology) and suboptimal healthcare utilization (Current Psychiatry Reports, Behavior Modification & International Journal of Cardiology). Although research on behavioral treatments for healthy anxiety associated with adult congenital heart disease is undoubtedly required, there have been very few trials conducted to date, with only one trial for anxiety in ACHD and no trials for health-related anxiety specifically.
Subscribe to the latest updates from Cardiovascular Advances in Motion
SMART-3RP
Our research team in the Department of Cardiology at Massachusetts General Hospital developed a mind-body intervention to improve resiliency in patients with chronic medical conditions that can be delivered via synchronous group videoconferencing. This intervention, called the Stress Management and Resiliency Training Program-Relaxation Response Resiliency Program (SMART-3RP), is an 8-week group intervention with sessions lasting 1.5 hours each that combines mind-body medicine, cognitive behavioral therapy, and positive psychology skills to improve stress coping and enhance resiliency (Psychosomatics). The program maintains the in-person benefits of real-time interactions with peers and a clinician, with the added benefits of convenience and accessibility (Maternal and Child Health Journal, Journal of Autism and Developmental Disorders & Global Advances in Health and Medicine).
Mind-body skills promote stress awareness and offset the negative physiological effects of stress through elicitation of the relaxation response. Skills from cognitive behavioral therapy and positive psychology help patients develop adaptive perspectives and positive coping strategies (General Hospital Psychiatry).
In multiple clinical trials of other patient populations, the SMART-3RP has been associated with improvements in stress coping, resiliency, and anxiety symptoms (Psychosomatics & Maternal and Child Health Journal).
CV Clinical Trial
In our waitlist-controlled, randomized pilot feasibility trial, we explored the feasibility and acceptability of videoconference-delivered SMART-3RP as well as the feasibility and acceptability of remote blood pressure monitoring and monitoring the changes in health anxiety, mindfulness, and resiliency.
In each session of eight total, participants learned about stress and resiliency, practiced relaxation response exercises, and learned skills for coping with stress and anxiety using cognitive-behavioral therapy as well as positive psychology techniques. A licensed clinical psychologist trained in the SMART-3RP protocol and experienced in working with patients with cardiovascular disease delivered the intervention. Participants received weekly guided audio recordings of relaxation response practices and were encouraged to practice at home daily. All sessions were delivered over a HIPAA-secure secure group video conferencing platform where participants could see, hear, and interact with each other and the group leader in real time.
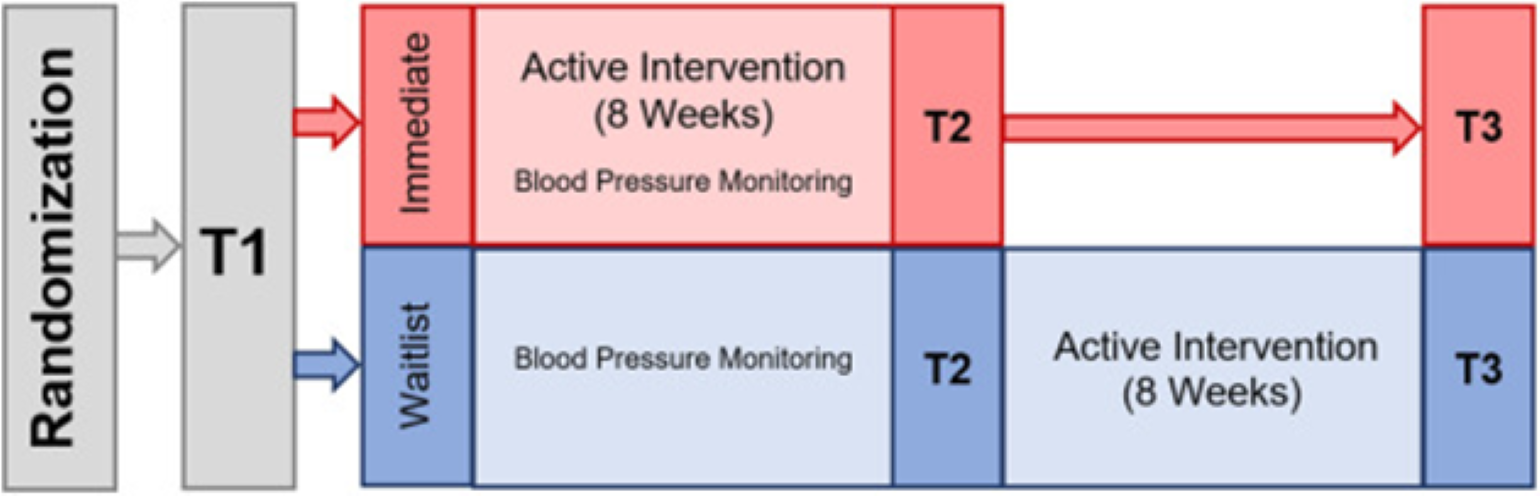
Figure 1
CV Clinical Trial chart, a waitlist-controlled, randomized pilot feasibility trial that explored the feasibility and acceptability of videoconference-delivered SMART-3RP. Image courtesy of Ami B. Bhatt, MD.
Results
Validated self-report measures of health anxiety (primary psychological variable), mindfulness (secondary psychological variable), and resiliency (secondary psychological variable) were used to assess outcomes. Health anxiety was assessed using a 14-item version of the Short Health Anxiety Inventory (SHAI), which assesses anxiety related to one's physical health and bodily sensations (Cognitive Therapy and Research). Mindfulness was measured using the 12-item Cognitive Affective Mindfulness Scale-Revised (CAMS-R), which measures the tendency to be mindful in everyday life (Journal of Psychopathology and Behavioral Assessment). Scores can range from 12 to 48 and higher scores are better. Resiliency was measured using the 21-item Current Experiences Scale (General Hospital Psychiatry), a revised version of the Post-traumatic Growth Inventory that assesses the ability to cope with the chronic stressors of daily living.
We found that health anxiety, mindfulness, and resiliency tended to improve in the intervention group compared to the waitlist group with a medium-large effect size for the between-group difference (Cohen's r = −0.36 to −0.62). The results of Wilcoxon signed rank tests of the full sample across their intervention period indicated medium-large effect sizes in the direction of improvement (Cohen's r = −0.44 to −0.59).
All participants reported that they learned helpful skills, most commonly the brief breathing exercises, and conveyed that they enjoyed the group connection with other ACHD patients. Most participants also liked the virtual delivery method since it eliminated transportation challenges. The most-reported improvements were emotional improvements, with almost all participants reporting reduced levels of anxiety or stress, and improved stress coping by using the skills taught in the intervention. Many participants reported psychological changes in terms of increased mindfulness (i.e., the ability to pay attention and choose adaptive behaviors during everyday life). Some participants also reported reduced physical symptoms (e.g., heart palpitations, neck tension) and improved health behaviors (e.g., improved sleep due to using relaxation skills before bed or upon waking in the middle of the night). Several participants reported improvements in utilizing their social support systems outside of the group, and a couple reported having increased empathy for others.
Additionally, participants were given the opportunity to provide suggestions for improvement. One important suggestion was targeting the intervention skills directly to ACHD-related stressors, such as applying skills in moments of physical symptoms, medical appointments, and test results.
The Mass General Adult Congenital Heart Disease Program and the Benson Henry Mind Body Institute collaborative pilot in using resilience training for the treatment of health-related anxiety revealed quantitative and qualitative improvements in patient experience and positive psychological change. Patients acted as partners in the post-study period, suggesting mechanisms to improve upon the curriculum and its implementation to maximize its effect. Holistic care of individuals with chronic disease is known to improve experience and outcomes, and in this research study, we observed that virtual resiliency training was effective and accepted by patients who are all too familiar with the healthcare system. The team is currently applying for NIH grants to perform larger studies and continuing to raise funds to support additional cohorts of patients who are awaiting the opportunity to learn coping skills as part of their cardiovascular well-being.
Learn more about the Corrigan Minehan Heart Center
Refer a patient to the Corrigan Minehan Heart Center