Managing PEEP and Recruitment
The FLARE Four
- ARDS is a disease of surfactant dysfunction and alveolar collapse that results in regions of V/Q mismatch and shunt. The application of PEEP can open, or "recruit," poorly ventilated alveoli. Opening alveoli decreases shunt, improves oxygenation and can simultaneously improve pulmonary mechanics since the higher regional volume may be associated with higher compliance
- Overdistension of lung units, however, results in decreased compliance and barotrauma. PEEP must be titrated to balance the benefit from recruitment of affected lung units against the risk of over distending unaffected units
- Many people are saying that patients with COVID-19 oxygenate well on low to moderate levels of PEEP but do not improve with more aggressive maneuvers. Patients are thus simultaneously easy to recruit (i.e. fully open at low PEEP), but do not respond to (aggressive) recruitment
- Care must therefore be taken to choose the PEEP that captures the benefit of recruiting the easily recruitable lung units without the pitfall of over distending the large amount of normal lung. No method of PEEP optimization is known to be superior to any other. Tabulated PEEP-FiO2 tables are likely a reasonable first approach while a select group of patients may benefit from more individualized PEEP titration
Many people are asking...how should I manage PEEP and alveolar recruitment in COVID-19 ARDS patients?
Subscribe to the latest updates from FLARE Advances in Motion
In this FLARE, we will review recruitment maneuvers, PEEP titration and best PEEP trials based on tidal compliance.
What's the Deal with Recruitment, Anyway?
A recruitment maneuver is a sustained increase in mean airway pressure with the goal to open collapsed alveoli, after which PEEP is applied at a sufficient level to keep alveoli inflated (Hess, 2015). As a reminder, the early trials using high PEEP and recruitment strategies - called the “open lung” approach - showed no mortality benefit (reviewed in detail in the March 23rd FLARE). This was revisited in the large Alveolar Recruitment for ARDS Trial (ART) in 2017. ART enrolled 1010 patients with moderate or severe (PaO2:FiO2 ≤ 200) ARDS across 120 ICUs and 9 countries. Patients were randomized to receive either: (1) an open lung approach - meaning a formal recruitment maneuver followed by decremental PEEP titration to assess the best tidal compliance, or (2) the conventional ARDSnet low PEEP strategy (Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators et al., 2017). 28-day all-cause mortality was increased with the “open lung” approach (55.3% vs 49.3%, HR 1.20, 95% CI 1.01-1.42, p=0.04) as shown in the figure below.
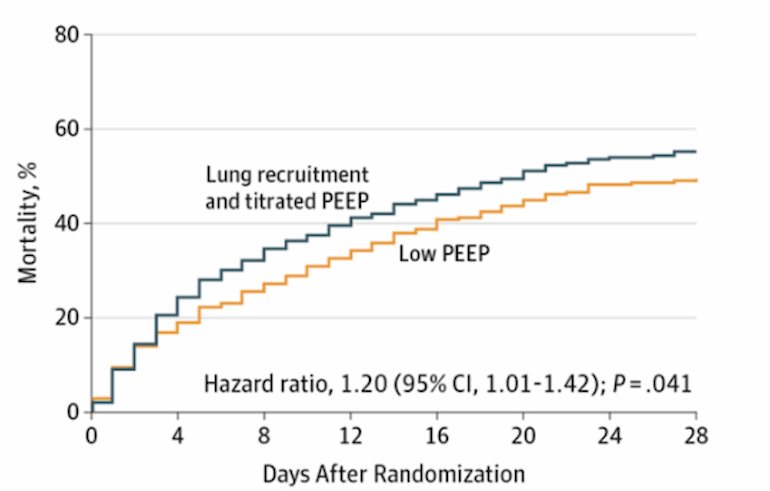
Figure 1
Critics of the ART trial note the high pressures used during recruitment (PEEP up to 45 cmH2O in 40% of patients; for reference, peak inspiratory pressures > 30 cmH2O are generally avoided due to risk of barotrauma). There was evidence of harm from the high pressures - the protocol was modified after cardiac arrests were reported during recruitment and recruitment attempts also resulted in episodes of hemodynamic instability requiring pressors and intravenous fluids.
Driving pressures (Pplat - PEEP) were also similar between treatment and control groups (13.0 and 11.5 cmH2O). Since tidal volumes were similar between the groups as well, the small difference in driving pressure suggests compliance (tidal volume ÷ driving pressure) was similar between the two groups. In ARDS, compliance is generally a function of lung volume. If compliance was similar in the recruitment maneuver group and the control group, then the maneuver did not likely augment lung volume - i.e. no recruitment actually occurred. The trial has therefore been criticized for not attempting to identify the patients who were likely to benefit from recruitment. Physiologically, there is potential for significant local overdistension and potential for significant barotrauma with recruitment. ART therefore suggests that, while it may still be possible that a PEEP-responsive subgroup of ARDS exists, there is certainly great potential for harm in aggressive recruitment of unselected ARDS patients, harm that is likely additive with each subsequent maneuver. There appears to be little rationale for daily recruitment maneuvers and frequent, aggressive PEEP titration.
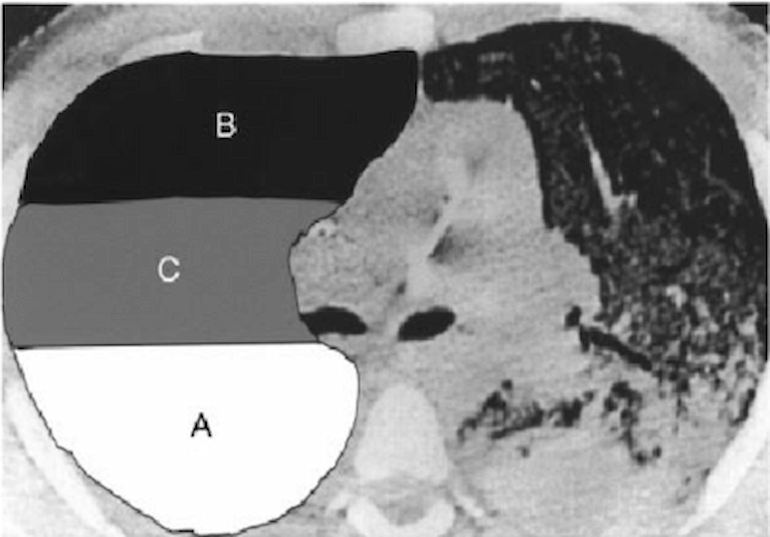
Figure 2
ARDS is heterogenous. A, B and C may represent areas with different mechanics and hence different ideal PEEP (Moloney and Griffiths 2004).
My Patient Keeps Desaturating with Turns. Should I Be Recruiting Them to Help with Oxygenation?
Probably not. The most likely reason patients desaturate with repositioning is indeed alveolar collapse and de-recruitment; however, frequent recruitment maneuvers are not the answer because each repeated recruitment maneuver will lead to cumulative barotrauma to injured alveoli, even if it does succeed in opening others. Derecruitment is best prevented with optimization of standing PEEP. In addition, keep in mind that not all positional hypoxemia is de-recruitment. The differential diagnosis for positional desaturation also includes increased shunt fraction with a gravitational gradient increasing flow to consolidated lung and maldistribution of pulmonary perfusion leading to hypoxemic vasoconstriction and RV strain. Practitioners may consider increasing PEEP moderately (by 2-5 cmH2O) preemptively prior to positional changes. One should also ensure that patients are adequately diuresed as excess extravascular lung water can exacerbate derecruitment.
How Should I Optimize PEEP?
Please refer to our previous FLARE on PEEP titration in ARDS for the evidence regarding different PEEP strategies. A variety of ways of setting PEEP have been reported, none clearly superior to any other. Here we will discuss two methods that are in common use: the ARDSnet FiO2 - PEEP tables and best PEEP by tidal compliance.
1. ARDSnet Tables
A defensible approach, particularly when time or available expertise does not allow for formal PEEP titration, is to simply set PEEP by the low PEEP / high FiO2 ARDSnet table (Acute Respiratory Distress Syndrome Network et al., 2000).
The ARDSnet tables, created by a consensus review by experts, do not take into account individual lung physiology. However, they provide a good framework for ventilator management (Brower et al. 2004). There are two ARDSnet tables: one for higher and one for lower PEEP, but data are lacking for the superiority of the high PEEP table. There may be benefit in a subset of patients or in obese patients. Therefore, a reasonable strategy to optimize PEEP is simply to adopt the low PEEP high FiO2 table.
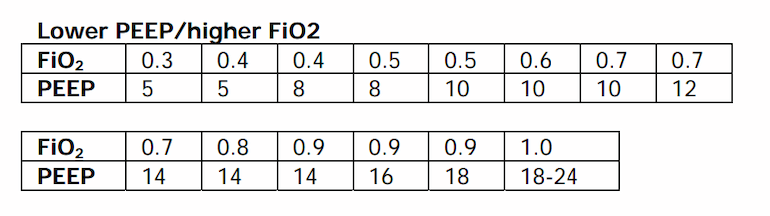
Table 1
ARDSnet low PEEP / higher FiO2 table (Brower et al. 2004).
2. Best PEEP Trial By Tidal Compliance
The rationale for individualized PEEP titration has always been based on the fact that the pressure volume curve of the lung is a) non-linear and b) exhibits hysteresis (see figure). In other words, the slope of the curve, which is compliance, may be greater at higher lung volumes (though becomes lower again at the highest volumes) and the pressure required to open a lung unit is higher than the pressure required to keep it open. This is illustrated in the figure below.
Steady application of high airway pressure can therefore increase lung volume and result in a higher compliance, and this higher volume can then be maintained at a lower airway pressure. In this circumstance, transient high pressure results in sustained improved gas exchange and mechanics.
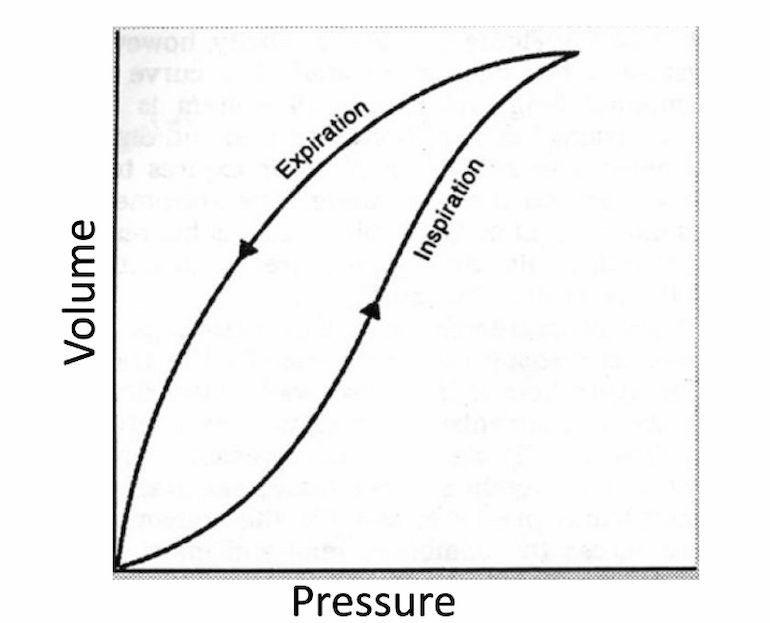
Figure 3
In the circumstance described above, the PEEP associated with best compliance will also optimize gas exchange -- identifying this PEEP in patients is the goal of individualized PEEP titration. In principle, the “best PEEP” may be found by calculating the compliance at a variety of PEEPs, moving either up or down from the patient’s current PEEP until the correct level is identified. In ART, a recruitment maneuver was performed first and the trial performed in a decremental fashion to find the lowest PEEP that would maintain recruitment. However, as noted above, this approach was associated with harm in unselected patients.
How do we identify best PEEP based on tidal compliance without a recruitment maneuver? Below is an example of the data generated for a patient at a constant tidal volume of 400ml. The patient is kept at a single level of PEEP for five minutes before taking measurements.
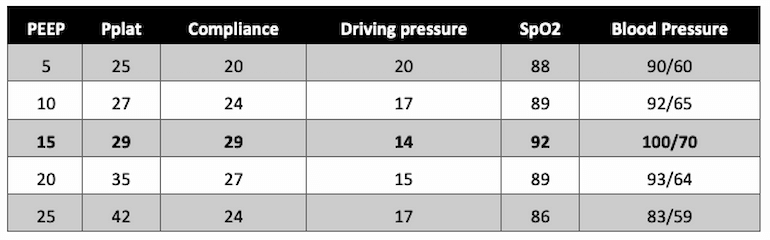
Table 2
Example of the results of a PEEP titration, with the "best" PEEP indicated in bold font.
In this example, a PEEP of 15 results in the lowest driving pressure (Pplat - PEEP), a Pplat <30, and the highest SpO2 without evidence of hypotension (which can be an adverse effect of higher PEEP due to increased right ventricular afterload and impaired venous return).
3. Why Wait 5 Minutes Between PEEP Titration?
Prior evaluation by Chiumello et al. demonstrated that when PEEP was decreased, oxygen-related variables such as PaO2 seemed to have the most dramatic change within 5 minutes of alteration (Chiumello et al., 2013). Although complete equilibrium of compliance was not always achieved within the 5 minute time window, this time frame has been viewed as a compromise to help determine clinical change while avoiding damage through overdistention or hemodynamic compromise.
The Bottom Line
Recruitment maneuvers are an appealing intervention in COVID-19-induced ARDS because they are associated with improved oxygenation in the short-term. However, recruitment maneuvers can also lead to hemodynamic instability, and there is a strong physiologically-grounded concern for worsening lung injury. In the current outbreak of COVID-19-associated ARDS, it appears that full recruitment is often easily achieved with low to moderate PEEP. This is fortunate, but should not be confused with such patients being ‘not recruitable’ or not having a ‘different kind of ARDS’. It is perverse, after all, to say that achieving a thing means the thing did not exist! At the same time, having achieved full recruitment, it is equally important to avoid the temptation to place additional strain on the lung with additional maneuvers. Large multicenter trials show no benefit from alveolar recruitment maneuvers in ARDS, and, in fact, show some evidence for harm. We favor careful application of stepwise changes in PEEP to a level that optimizes respiratory system compliance by balancing alveolar overdistension and recruitment. It is very frequently the case that the same optimal PEEP may be achieved with use of the ARDSnet table.
References
- Acute Respiratory Distress Syndrome Network, Brower, R.G., Matthay, M.A., Morris, A., Schoenfeld, D., Thompson, B.T., and Wheeler, A. (2000). Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 342, 1301–1308.
- Amato, M.B.P., Meade, M.O., Slutsky, A.S., Brochard, L., Costa, E.L.V., Schoenfeld, D.A., Stewart, T.E., Briel, M., Talmor, D., Mercat, A., et al. (2015). Driving pressure and survival in the acute respiratory distress syndrome. N. Engl. J. Med. 372, 747–755.
- Brower, R.G., Lanken, P.N., MacIntyre, N., Matthay, M.A., Morris, A., Ancukiewicz, M., Schoenfeld, D., Thompson, B.T., and National Heart, Lung, and Blood Institute ARDS Clinical Trials Network (2004). Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N. Engl. J. Med. 351, 327–336.
- Chiumello, D., Coppola, S., Froio, S., Mietto, C., Brazzi, L., Carlesso, E., and Gattinoni, L. (2013). Time to reach a new steady state after changes of positive end expiratory pressure. Intensive Care Med. 39, 1377–1385.
- Hess, D.R. (2015). Recruitment Maneuvers and PEEP Titration. Respir. Care 60, 1688–1704.
- Hickling, K.G. (2001). Best compliance during a decremental, but not incremental, positive end-expiratory pressure trial is related to open-lung positive end-expiratory pressure: a mathematical model of acute respiratory distress syndrome lungs. Am. J. Respir. Crit. Care Med. 163, 69–78.
- Hubmayr, R.D. (2002). Perspective on lung injury and recruitment: a skeptical look at the opening and collapse story. Am. J. Respir. Crit. Care Med. 165, 1647–1653.
- Moloney ED, Griffiths MJ. Protective ventilation of patients with acute respiratory distress syndrome. Br J Anaesth. 2004;92(2):261–270. doi:10.1093/bja/aeh031.
- Pintado, M.-C., de Pablo, R., Trascasa, M., Milicua, J.-M., Rogero, S., Daguerre, M., Cambronero, J.-A., Arribas, I., and Sánchez-García, M. (2013). Individualized PEEP setting in subjects with ARDS: a randomized controlled pilot study. Respir. Care 58, 1416–1423.
- Suter, P.M., Fairley, B., and Isenberg, M.D. (1975). Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N. Engl. J. Med. 292, 284–289.
- Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti, A.B., Suzumura, É.A., Laranjeira, L.N., Paisani, D. de M., Damiani, L.P., Guimarães, H.P., Romano, E.R., Regenga, M. de M., Taniguchi, L.N.T., et al. (2017). Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA 318, 1335–1345.
View all COVID-19 updates
Learn about research in the Division of Pulmonary and Critical Care Medicine