Minimally Invasive Surgery Linked to Shorter Survival in Early-Stage Cervical Cancer
Key findings
- In a large retrospective study, minimally invasive radical hysterectomy for early-stage cervical cancer was associated with a significantly higher risk of death compared with open surgery
- This association was apparent regardless of laparoscopic approach (robot-assisted or traditional), histologic type or tumor size
- Adoption of minimally invasive radical hysterectomy in 2006 coincided with a decline in cancer-related survival
In patients with early-stage uterine, colorectal or gastric cancer, randomized clinical trials have shown that survival is similar whether surgery is open or minimally invasive. That might partly explain why minimally invasive radical hysterectomy has become the standard treatment for early-stage cervical cancer despite a lack of high-quality supporting data.
Subscribe to the latest updates from OB/GYN Advances in Motion
Now, gynecologic oncology fellow Alexander Melamed, MD, MPH, and Marcela G. del Carmen, MD, MPH, a gynecologic oncologist in the Center for Gynecologic Oncology, and colleagues have reported that minimally invasive surgery for early-stage cervical cancer is actually associated with significantly shorter survival. They report their findings in the New England Journal of Medicine.
The research team reviewed the National Cancer Database, a cancer registry that includes about 70% of newly diagnosed cancer cases in more than 1,500 U.S. hospitals. They identified 2,461 women with stage IA2 or IB1 cervical cancer who were diagnosed between 2010 and 2013, underwent radical hysterectomy as their primary treatment and did not receive neoadjuvant chemotherapy or radiotherapy. Half of the women (49.8%) underwent minimally invasive surgery.
The researchers first determined that a patient's propensity to undergo minimally invasive radical hysterectomy rather than open surgery was predicted by a number of factors, including:
- Race/ethnicity
- Type of insurance
- Year of diagnosis
- Income and education
- Type of hospital
- Tumor size and grade
By accounting for these differences, they created a "propensity-weighted" cohort of patients who differed with respect to surgical approach but were similar in terms of other characteristics.
The median follow-up in that cohort was 45 months. The four-year mortality rate was 9.1% in the minimally invasive surgery group and 5.3% in the open-surgery group. That represented a 65% higher risk of death from any cause for women who had minimally invasive surgery (HR, 1.65; 95% CI, 1.22–2.22; P=.002) (Figure 1).
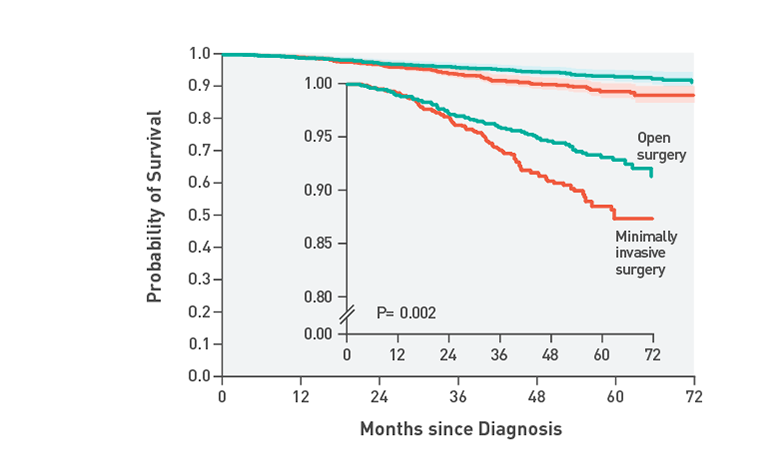
Fig. 1: Inverse Probability of Treatment–Weighted Survival Curves Among Women with Stage IA2 or IB1 Cervical Cancer, According to Type of Surgery
Shaded bands represent the 95% confidence interval. Women who underwent minimally invasive surgery had shorter overall survival than those who underwent open surgery (P=0.002 by the log-rank test). The at-risk table shows the actual number of patients at risk. The inset shows the same data on an enlarged y axis.
Subgroup Analysis Reveals Differences
Exploratory subgroup analyses showed that the risk of death with minimally invasive surgery was higher whether patients underwent robot-assisted laparoscopy (61% higher risk of death) or traditional laparoscopy (50% higher risk of death). The higher risk was also apparent regardless of histologic types and tumor sizes.
The research team analyzed how the adoption of minimally invasive surgery has affected survival trends for U.S. patients with early-stage cervical cancer. To do this, the researchers used the April 2017 release of the Surveillance, Epidemiology, and End Results database maintained by the National Cancer Institute.
During the period from 2000 to 2006 before minimally invasive radical hysterectomy was being used, there was a nonsignificant trend toward longer cancer-related survival over time (Figure 2). After 2006, there was a significant change of trend (P=.01), such that the four-year relative survival rate declined 0.8% per year between 2006 and 2010.
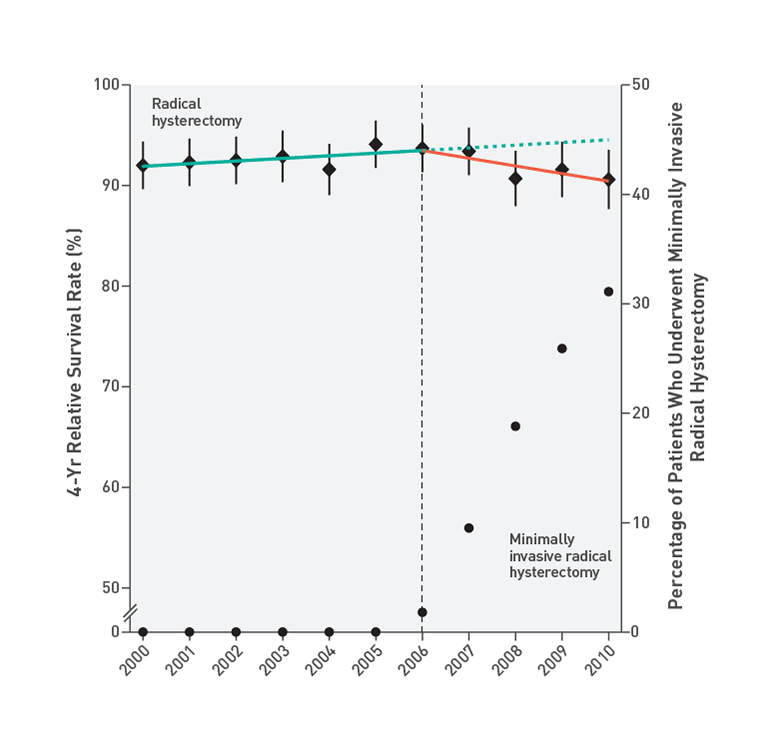
Fig. 2: Interrupted Time-Series Evaluation of the Effect of Adoption of Minimally Invasive Radical Hysterectomy on 4-Year Relative Survival Rate
Shown are the 4-year relative survival rates among women who underwent radical hysterectomy for cervical cancer by any surgical approach (diamonds) with 95% confidence intervals (error bars) and the percentages of radical hysterectomies that were undertaken with the use of a minimally invasive approach (circles). The adoption of minimally invasive radical hysterectomy in 2006 was associated with a significant change of temporal trend (as indicated by the dotted blue line) (P=0.01) and a declining 4-year relative survival rate after 2006 (yellow line) (annual percentage change, 0.8%; 95% CI, 0.3 to 1.4).
Potential Explanations for Shorter Survival Rates
The researchers note that a retrospective study cannot explain why minimally invasive surgery was associated with shorter survival, but they propose several potential explanations:
- There may be inherent differences between open and minimally invasive radical hysterectomy in terms of the amount of resection achievable
- In this cohort, close surgical margins may have been more common in the minimally invasive surgery group than in the open surgery group
- Uterine manipulators are frequently used during minimally invasive hysterectomy, and it may be that they disseminate tumor cells
- Cancer control after minimally invasive radical hysterectomy may be sensitive to the surgeon's length of experience. If so, the survival difference after open surgery and minimally invasive surgery should diminish as surgeons gain experience with minimally invasive surgery
The researchers call attention to a prospective, randomized study of minimally invasive radical hysterectomy for cervical cancer that is reported in the same issue of the New England Journal of Medicine. The findings of that study were similar to theirs.
view original journal article Subscription may be required
Learn more about the Center for Gynecologic Oncology
Learn more about OB/GYN research