Paradigm Change: Patient and Provider Expectations Around Same-day Discharge
In This Article
- Newly modified enhanced recovery after surgery (ERAS) protocol guides same-day discharge of vaginal hysterectomy patients while maintaining quality of patient care
- Pre-operative patient education counseling and discharge criteria change patients’ and practitioners’ expectations about hospitalization
Same-day discharge for elective vaginal hysterectomy was once considered an unacceptable risk to patients, but a new protocol in the Female Pelvic Medicine & Reconstructive Surgery Program (FPMRS) at Massachusetts General Hospital is helping make same-day discharge the norm. A team of researchers led by May Wakamatsu, MD, FPMRS director, and former FPMRS member Samantha Pulliam, MD, is leading this paradigm change with the development of new medical guidelines for a safe same-day discharge protocol and identification of key social factors to support that change. The protocol has been so successful that the team is now looking for opportunities to generalize this protocol to decrease patient stays.
Subscribe to the latest updates from OB/GYN Advances in Motion
Getting patients home more quickly has a significant impact on patient care. “I hear from patients in my practice that they want to be home, in their own bed, with their own food,” said Milena Weinstein, MD, a urogynecologist in the FPMRS Program who was involved in the development of the protocol. “It’s really a better-quality recovery in so many ways.”
Same-Day Discharge Rate Greatly Increased in Two Years
Dr. Wakamatsu’s team began by reviewing all elective vaginal hysterectomy cases from the previous year to determine how long most patients stayed in the hospital after surgery. When the research began in 2013, 99% of vaginal hysterectomy patients stayed overnight after surgery.
This research also included creative collaboration among the medical team focused on patient care during and after vaginal hysterectomy. The research team spoke with care team members and conducted a survey among nurses in the unit to identify the most common causes for delayed discharge.
Armed with this information, the research team set out to change discharge protocols to decrease the amount of time patients spend in the hospital, while also decreasing patient costs and increasing hospital efficiency and throughput—all while ensuring the quality of patient care stayed the same.
By 2014 after the application of the new enhanced recovery after surgery (ERAS) protocol, 25% of patients returned home the same day as their surgery after meeting key discharge criteria. In addition, the average length of stay decreased by one hour, from 29.6 hours to 28.6 hours between July 2012 to March 2014 (Figure 1).
While decreasing average length of stay by one hour may not sound significant, this seemingly small decrease can help significantly improve hospital through-put of patients and help alleviate bed shortages.

Fig. 1: Length of Stay After Vaginal Hysterectomy
Data includes all cases between July 2012 and March 2014. Note: Average duration exceeds a 24-hour day because the measure is an average and includes cases with comorbidities and complications.
“We looked at the potential negative outcomes of same-day discharge and didn’t find any,” Dr. Wakamatsu said. By tracking such measures as post-operative calls from home to the hospital, post-operative emergency room visits, extra office visits and interviewing patients, researchers concluded the approach is safe, successful and well-liked by patients.
Use of the ERAS protocol has continued in the FPMRS Program, and at present approximately 80% of patients returned home on the same day as their surgery.
Setting Patient Expectations for Surgery
“Our patients tend to be older, and they want to recover at home—and that was a driver in our research,” said Dr. Weinstein. “In the past, a woman who was 70-years-old wasn’t likely to be running or kayaking or sailing. But in my practice, they do. They want a rapid return home and a rapid recovery.”
Social factors proved to be an important component for facilitating same-day discharge and supporting faster recovery for these patients. Two social factors in particular stood out:
- Managing patient expectations about discharge and recovering from major surgery
- Coaching patients to ensure they know who will give a ride home
“We noticed that medically, some patients could have gone home the same day. But they stayed in the hospital largely because they expected to do so after major surgery,” explained Dr. Wakamatsu. “The transportation finding was particularly surprising. It seems simple, but lack of a ride home can be a common obstacle to discharge.”
Research Methodology
Dr. Wakamatsu’s team used a methodology called the PDSA Cycle: Plan, Do, Study, Act (Figure 2). The PDSA is a four-stage method for process analysis of data typically used in commercial quality-control settings. Its goal is to produce rapid, iterative improvements. The application of this model with Mass General’s gynecological surgery patients enabled researchers to identify key variables to change in patient preparation and care after surgery, while the routine vaginal hysterectomy operative procedure itself did not change.
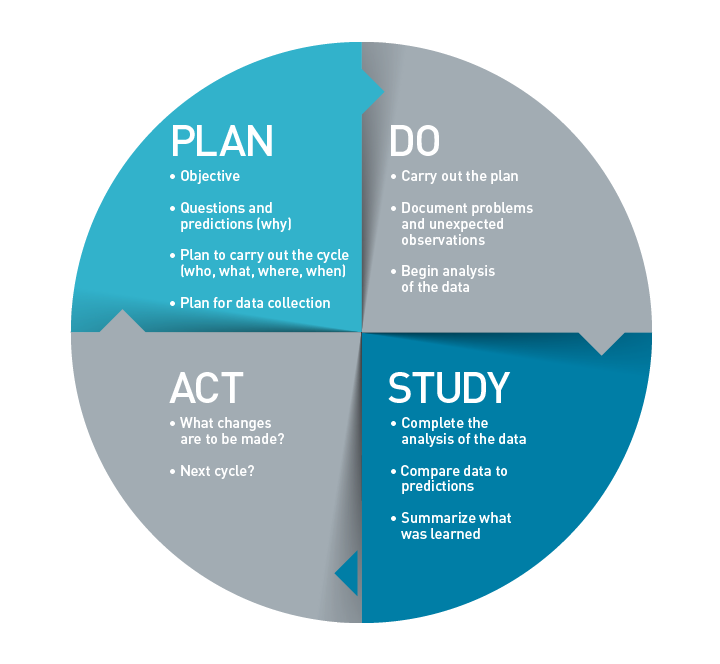
Fig. 2: The PDSA Cycle (Plan, Do, Study, Act)
A four-stage method developed by W. Edwards Deming and Walter A. Shewhart for process analysis and change based on rapid, iterative improvements.
“From my point of view as a surgeon, I did what I always do,” Dr. Wakamatsu said.
Investigators reviewed the entire continuum of care to develop the safe same-day “discharge on criteria” orders and coached staff to follow these rather than simply assuming patients will stay overnight. To be discharged, a patient must meet the following criteria after surgery:
- No signs of fever
- No excessive nausea and sleepiness from anesthesia
- Ability to eat and drink
- Ability to walk
According to Dr. Wakamatsu, the most impactful change was simply writing post-op orders differently so that the nurse can discharge the patient when she is ready to go home.
The research team worked with major medical stakeholders—including anesthesiologists, post-anesthesia care unit (PACU) nurses and floor nurses—to enact processes that helped facilitate faster patient discharge, including:
- Improving post-operative nausea management
- Providing discharge information and prescriptions ahead of time
- Standardizing anesthesia practices
A Paradigm Change
Based on these early results and the progress they’ve seen within the FPMRS program since then, Dr. Wakamatsu and Dr. Weinstein believe this approach can be safely applied to other gynecologic surgical specialties and encourage its consideration to decrease length of stays.
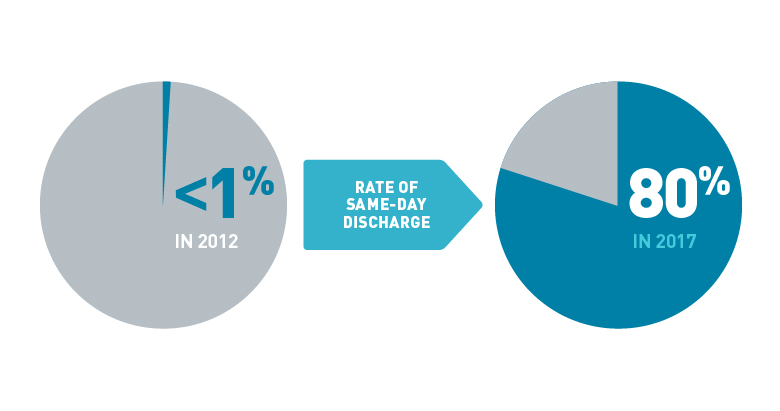
Fig. 3: A Dramatic Change for FPMRS Patients
Since 2012 and the development of the new ERAS protocols, the rate of same-day discharge among vaginal hysterectomy patients in the FPMRS program has changed dramatically. Following this initial success, the ERAS protocol has been extended to other surgeries.
Because the initial results with elective vaginal hysterectomy were so strong, the same-day discharge protocol has already been extended to include longer, more complicated laparoscopic procedures and robotic reconstructions across FPMRS.
“The modified ERAS protocol has really served us well—both caregivers and patients,” said Dr. Wakamatsu. “So far, we see no down sides to this approach. When I was trained, everyone stayed two nights in the hospital, but now I rarely have patients stay overnight. It really is paradigm changing.”
Learn more about the Female Pelvic Medicine & Reconstructive Surgery Program
Learn more about the Gynecology at Mass General