Perinatal Substance Use Clinic: Multidisciplinary Care from Pregnancy to Early Childhood
In This Article
- An increasing number of women with opioid use disorder are becoming pregnant and facing the challenges of motherhood while living with this disease
- Pregnancy and early motherhood are a unique time to engage in treatment for substance use disorders and provide care for both mother and child
- A multidisciplinary, 1000-day clinical model offers a new approach to prenatal and postnatal care for mothers with opioid use disorder and their children
Over the past decade, the use of opioids has increased drastically and with that has come an increase in opioid use during pregnancy. However, pregnant women struggling with opioid use disorder (OUD) are often motivated to seek treatment after their first trimester of pregnancy and early in the lives of their newborns.
Subscribe to the latest updates from OB/GYN Advances in Motion
In 2015 Massachusetts General Hospital established a hospital-wide Substance Use Disorders Initiative, which seeks to effectively transform care by improving outcomes of patients grappling with substance use and addiction. Clinicians across the hospital have been actively involved in tackling the challenges of the opioid epidemic.
Now, Mass General is launching the HOPE Clinic, a multidisciplinary clinic that supports women during pregnancy and early parenting years (roughly 1,000 days) to close care gaps in OUD patients before, during and after birth. This need is especially acute in Massachusetts, where the rate of opioid use is approximately three times that of the national average.
The HOPE Clinic
The coordinated care program at the HOPE Clinic—which stands for “Harnessing support for Opioid and substance use disorders in Pregnancy and Early childhood”— began enrolling patients in April 2018. The clinic is a collaboration of Mass General and MassGeneral Hospital for Children, led by a team of physicians including pediatrician Davida M. Schiff, MD, who serves as medical director, family medicine addiction specialist Jessica Gray, MD, who servers as clinical director, and maternal-fetal medicine specialist Sarah Bernstein, MD.
The program provides intensive, integrated care throughout pregnancy and the first two years of the child’s life. It focuses on both the child’s medical needs, such as treatment for neonatal abstinence syndrome, and those of the mother and other family members.
“What I’ve learned as a pediatrician,” says Dr. Schiff, “is that it’s clear we need to do a better job linking prenatal and postnatal services for women and families affected by substance use disorder so that we can make recovery resources and wrap-around services available across the care continuum.”
“Being a new mother is not easy,” says Dr. Gray. “And the challenges are even greater when the transition to motherhood is complicated by OUD, which is a high-stakes, chronic disease. By streamlining medical, psychological and recovery support services with the rest of the woman’s medical care, the HOPE Clinic addresses the needs of the mother and family in a patient-centered way.”
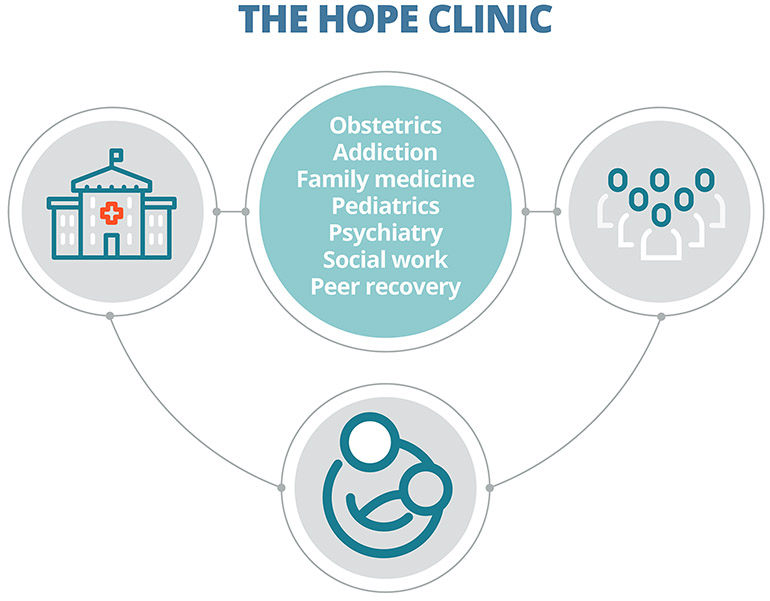
Fig. 1: A Multidisciplinary Team
The HOPE Clinic is staffed by a team of specialists from across Mass General and MassGeneral Hospital for Children with experience treating patients with substance use disorder.
Barriers to Care
The lack of stable health care benefits often jeopardizes the health of mother and child in the early postnatal period. “After six weeks, partly because of financial policies, care can become disjointed,” says Dr. Schiff. “That’s the time families need our help most.”
“Unfortunately for women with OUD, there is a lot of shame and stigma around their addiction and drug use and their baby’s health related to it,” says Dr. Bernstein. “That prevents them from seeking the prenatal care they need.”
Pregnant women with substance use disorder are often identified late in their pregnancies due to several factors:
- Patient shame
- Lack of screening tools
- Limited physician training during medical school and residency on identification and management of substance use disorders
- Insufficient evidence for best practices in treating neonatal opioid withdrawal syndrome
“Our goal is to create a warm, welcoming environment where we take the shame and stigma off the table so patients will feel comfortable coming to their visits,” says Dr. Bernstein.
The HOPE Clinic Care Continuum
For prenatal patients, the care team offers services from pediatricians, family medicine physicians, nurse-midwives and high-risk obstetricians. The team also includes psychiatrists, mental health counselors and addiction medicine professionals, as well as peer recovery coaches who share their experiences getting and staying in recovery.
This team works collaboratively to:
- Help women with OUD receive medication and behavioral treatment
- Devise and practice relapse prevention strategies
- Connect both parents with recovery-support groups and peer counselors
- Teach positive parenting skills
- Improve retention rates for prenatal care
- Keep women engaged in their own care during the chaotic postpartum period
- Monitor the medical status of the whole family
After the baby is born, services for the mother continue and expand to include services for infants. This includes care from neonatologists, addiction medicine specialists and lactation consultants.
Providing care for the family together as a unit is a key feature of the clinic. “As a family medicine physician, I was trained to identify and treat the family unit as the patient,” says Dr. Gray. “The illness or health of one member directly affects the well-being of the entire family. In the case of pregnant and parenting women with substance use disorder, this could not be more true.”
Advantages of the Integrated Clinical Model
The HOPE Clinic model provides a number of distinct clinical advantages:
- Long span of care. It reaches over a vulnerable period—from prenatal care to high-risk birth to postnatal care for the child’s first two years of life, including managing the challenges of a newborn exposed to opioids in utero
- Co-location of services. By co-locating multidisciplinary caregivers and social workers in the same space during the same hours, mothers, newborns, siblings and partners can be seen in one appointment. By streamlining the logistics of scheduling and location, HOPE aims to eliminate a common impediment to regular health care
- Multidisciplinary expertise. Mass General is well-suited to staff the HOPE Clinic with the full range of specialties needed by a diverse patient population struggling with SUDs-related medical, mental health, psychosocial and after-care issues
- Commitment to transforming care by effectively managing SUDs. Mass General prioritizes innovating clinical solutions to substance use disorders and has formed the Substance Use Disorders Initiative to do so
Roots of the HOPE Model
For Dr. Schiff, both her training and experience exposed her to the power of creative collaboration. “Addressing the opioid epidemic and its implications for mothers, children, families—and society—will require more than one or two practitioners operating in isolation. We need multidisciplinary teams of providers to support families in this vulnerable moment,” she says. “That’s why we believe the HOPE Clinic holds so much potential. Our integrated team will capitalize on the motivation women experience during pregnancy and provide intensive support to maintain their recovery following delivery. We believe this model can really help make a difference.”
Dr. Bernstein was also inspired by early experiences in her medical education. She trained in another area of the country affected by unusually high OUD rates. The experience convinced her that a creative care solution was needed.
“Mass General’s history is all about meeting patients’ needs by discovering original solutions to problems,” says Dr. Bernstein. “We are so excited to offer the HOPE Clinic as yet another contribution to this care ethic.”
Learn more about the HOPE Clinic
Learn more about the Substance Use Disorders Initiative