Using 3D-Printed Anatomical Models for Surgical Planning
In This Article
- Even with advanced cardiac imaging, surgeons face a steep learning curve with septal myectomy to treat hypertrophic cardiomyopathy
- Massachusetts General Hospital's chief of Cardiac Surgery has collaborated with radiologists and the Simulation Center to create 3D-printed anatomic models of individual hypertrophic hearts
- A model reveals an individual patient's complex abnormal anatomy to help the surgical team plan surgery and anticipate important details
- The technology has enormous potential in other conditions
Subscribe to the latest updates from Cardiovascular Advances in Motion
Cardiac surgeons at Massachusetts General Hospital are applying 3D-printing technology to create anatomical replicas of individual hypertrophic cardiomyopathy patients' hearts for use in preparation for septal myectomy. Thor Sundt, MD, chief of Mass General's Division of Cardiac Surgery and director of the Corrigan Minehan Heart Center, says the tool provides important details that improve surgical planning and facilitate the teaching of residents and fellows.
"We have remarkably sophisticated imaging approaches to look at hypertrophic cardiomyopathy, such as CT scan, MRI and echocardiogram. Yet it's very hard to bridge the gap between what the images show and what the surgeons do," Dr. Sundt says. "We're using 3D printing to bridge that gap—to make treatment of this condition more reliable, more predictable and easier to learn."
So far, the approach has been used to help surgeons at Mass General prepare for surgery in about 50 cases.
Shortening the Learning Curve and Improving Surgical Planning for Septal Myectomy
Hypertrophic cardiomyopathy is a common condition—affecting about 1 in 500 people, according to American Heart Association—in which the heart muscle becomes abnormally thick, making it harder for the heart to pump blood. However, this complex condition manifests differently in different patients.
Hypertrophic cardiomyopathy patients with obstructions in the heart require treatment. The primary options are alcohol ablation and septal myectomy, a type of open-heart surgery that removes part of the thickened septum between the ventricles, sometimes called the muscle bar.
"The surgical treatment is quite effective, but there aren't very many surgeons who perform it. One of the real challenges in this surgery is the learning curve. Without a certain volume of cases, it's very hard to teach. Complicating that is a very narrow field of view of the procedure through the aortic valve," Dr. Sundt says. "We want to develop techniques and modalities to help surgeons get over that learning curve faster so that more patients can be taken care of."
A 3D-printed, life-sized, realistic anatomical model of a patient's heart can help a surgeon plan the surgery and anticipate important details.
"I can get the model about a day before the surgery, and I can actually put my hands on it, feel it, look at it, measure it. That helps me integrate into my brain what exactly we need to do and what I can anticipate seeing in the operating room," Dr. Sundt says. "I can anticipate the instruments I will use in the operating room, such as graduated hooks of various depths and get a sense of how deep I need to reach down in the ventricle."
A 3D model of a hypertrophic heart can:
- Demonstrate the contour and thickness of the muscle so the surgeon knows in advance exactly where to excise
- Help the surgeon determine whether he or she needs to reposition anomalous papillary muscles, an anomaly that can be difficult to detect on imaging
- Reveal the morphology of the hypertrophy, such as a narrow, shallow muscle bar or one that extends further into the ventricle, which determines how deep the surgeon should go
In addition, Dr. Sundt says, the models have helped him facilitate patient education and train residents and fellows on what to expect during septal myectomy. He also brings the model to the operating room to enhance communication with the anesthesiologist performing transesophageal echocardiography.
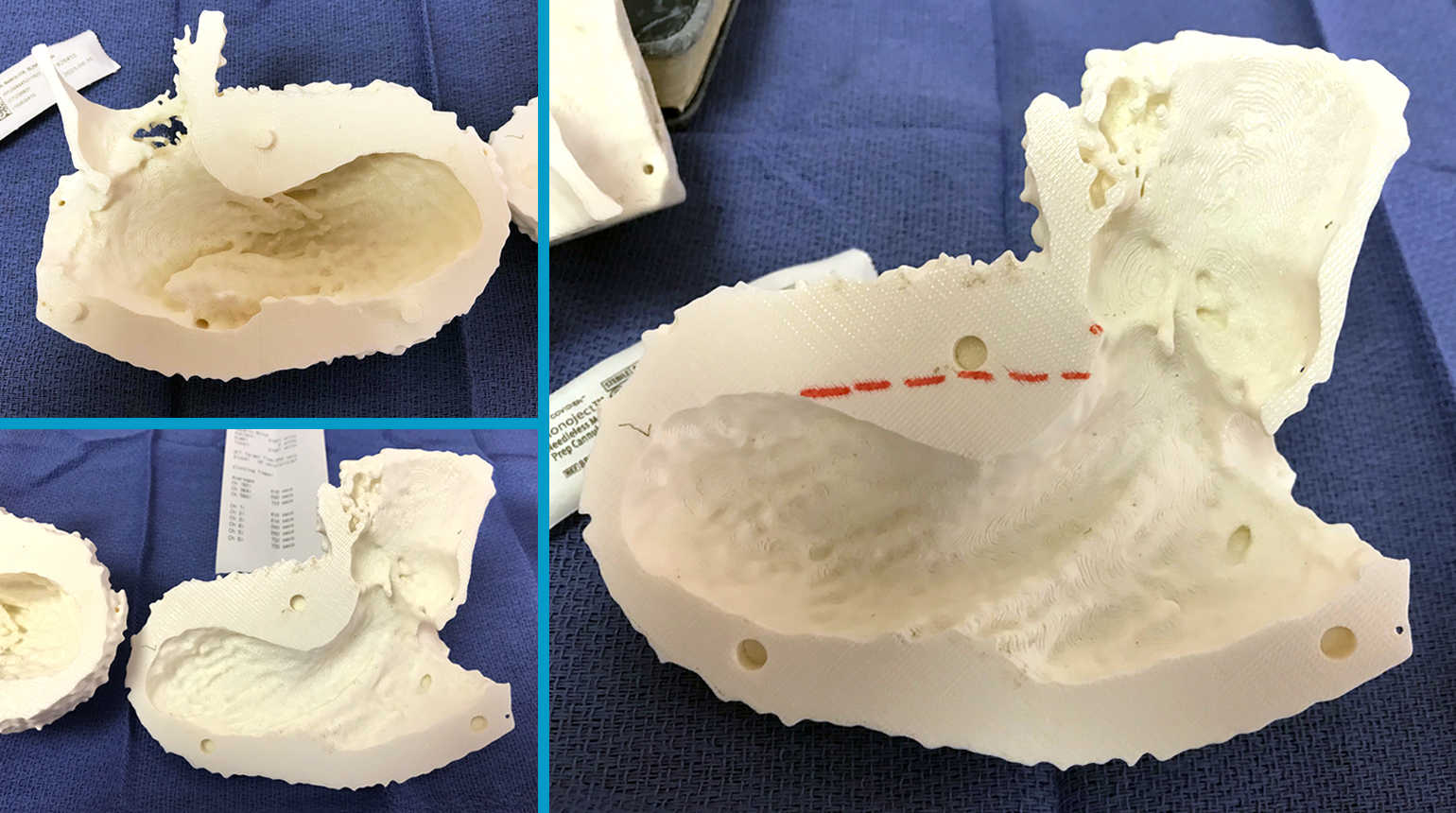
Figure 1
Examples of 3D printed heart models.
Using 3D Printing to Model Complex Abnormal Anatomy
Dr. Sundt envisions the technology being used in many more patients and other complex anatomies over time. To apply 3D technology to this type of cardiac surgery, Dr. Sundt collaborated with Mass General radiologists and Mark Ottensmeyer, MD, of Mass General's Simulation Group, which develops medical simulation systems to improve medical education, assist clinicians and surgeons and boost patient safety.
When developing a model for a clinician or surgeon, the Simulation Group determines whether existing images of the anatomy have sufficient resolution and contrast. They then apply software to the images to segment triangulated models of the anatomy in question, creating a model for printing.
Although the use of 3D-printed models in septal myectomy has not yet been published, the Simulation Group has presented the technology's contributions in other areas, such as:
- Anatomical models of the larynx for educational purposes, with separable hyoid, thyroid lamina, thyroid gland, and upper and lower laryngeal soft tissues
- Models of pediatric ears and ear canals for educational purposes
- Skeletal and vascular model of the torsos of conjoined twins to plan surgical separation
Dr. Sundt believes this is just the beginning and that 3D-printed anatomical models will have many more uses in treatment planning for other complex abnormal anatomy in the future.
"This is the kind of thing that will benefit everybody—surgeons, surgical teams, patients and trainees. So it's very closely aligned with our mission, which is not just to build our own personal clinical practice here. It's about trying to develop ways to disseminate knowledge to improve the care of everyone, everywhere," he says. "These 3D printing techniques are increasingly available, and they offer a real opportunity for us as surgeons."
Learn more about the Division of Cardiac Surgery at Mass General
Refer a patient to the Corrigan Minehan Heart Center