Benefits of Cytoreductive Nephrectomy with Targeted Cancer Therapy for Metastatic Renal Cell Cancer
In This Article
- Dramatic reduction in cytoreductive nephrectomies since the advent of targeted cancer therapies in mid-2000s.
- Studies continue to suggest that a combination of surgery and targeted therapy produces the best outcome for patients.
The development of targeted, non-surgical cancer therapies has led some physicians to question cytoreductive nephrectomy—surgery to remove the primary tumor—as the standard of care for metastatic renal cell carcinoma patients. Since the advent of targeted cancer therapies in the mid-2000s, there has been a 50% reduction in the number of cytoreductive nephrectomies (Figure 1).
Subscribe to the latest updates from Urology Advances in Motion
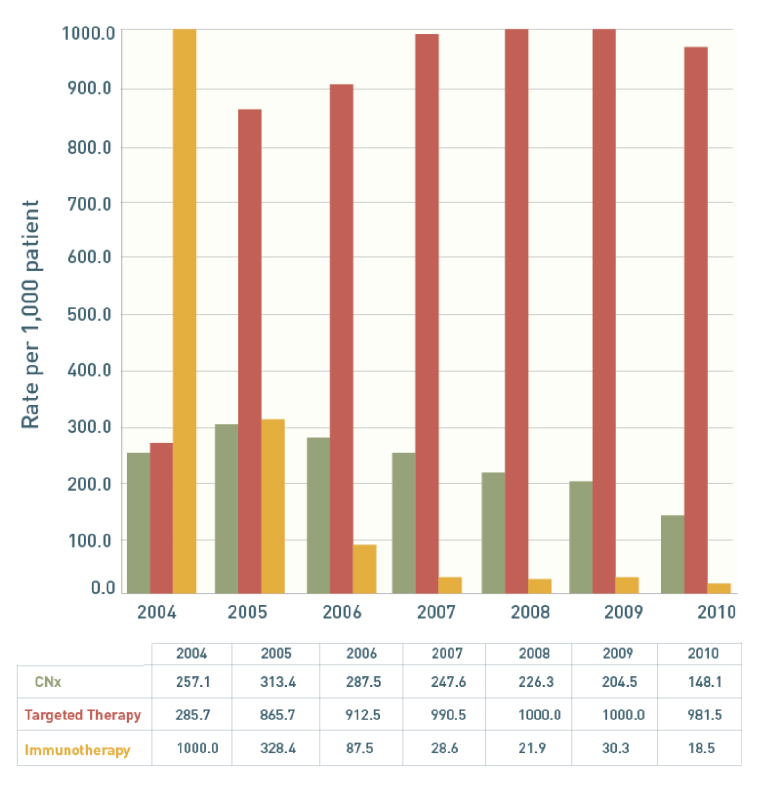
Figure 1: Trend Use of Cytoreductive Nephrectomies
The annual number of cytoreductive nephrectomies (CNx) decreased between 2005 and 2010 by about 50%. This decline began when the use of targeted cancer therapies nearly tripled from 2004 to 2005. (Source: Psutka SP, Kim PK, Gross CP, et al. The Impact of Targeted Therapy on Management of Metastatic Renal Cell Carcinoma: Trends in Systemic Therapy and Cytoreductive Nephrectomy Utilization. Urology. 2015.)
A review of the National Cancer Database published in the Journal of Clinical Oncology showed that currently only three out of ten patients with metastatic kidney cancer undergo cytoreductive nephrectomy. Improved systemic effectiveness and markedly increased tolerability compared to cytokine therapy has resulted in targeted treatment as before front-line therapy to cloud the role of cytoreductive nephrectomy in patients with metastasis. “The standard of care has shifted away from cytoreductive nephrectomy in the absence of level 1 evidence for its cancer survival benefit in the targeted therapy era,” says Michael Blute, MD, chief of the Department of Urology at Massachusetts General Hospital.
Dr. Blute states that abandoning cytoreductive nephrectomy as a standard of care should be viewed with concern. Cytoreductive nephrectomy has maintained its importance at the Mass General Cancer Center, where all patients with metastatic renal cancer are seen by urologic surgeons, and medical and radiation oncologists.
Targeted Therapy Combined with Surgery May Improve Outcomes for Patients
The majority of kidney cancers are caused by mutations in the von Hippel-Lindau tumor suppressor (VHL) gene, which activates proteins that promote angiogenesis and tumor cell growth. Targeted agents including sunitinib, sorafenib, pazopanib, bevacizumab and axitinib are designed to inhibit the angiogenic pathways that are affected by mutations in the VHL genes. These agents, which were FDA approved between 2004 and 2009, revolutionized the treatment of metastatic renal cell cancer.
Advances in the field have led to more recent approvals of additional drugs, including new generation angiogenesis inhibitors such as cabozantinib and lenvatinib, as well as immune-activating treatments such as nivolumab. Research is ongoing with widespread expectation for additional significant advances in the near future.
However, even with the advent of these new agents, studies continue to suggest that a combination of surgery and targeted therapy produces the best outcome for patients. Two preliminary 2011 reports suggested a benefit from cytoreductive nephrectomy before the initiation of targeted therapy. The first report in the Journal of Urology showed that median survival was 21.6 months for patients undergoing cytoreductive nephrectomy and targeted therapy (sunitinib or sorafenib), vs. 13.9 months for patients undergoing targeted therapy alone. However, the differences were not statistically significant due to small sample size.
The second Journal of Urology report, with larger sample size, showed that median survival was 19.8 months for the group undergoing cytoreductive nephrectomy combined with targeted therapy vs. 9.4 months for patients treated with targeted therapy (sunitinib, sorafenib, or bevacizumab) alone (Figure 2).
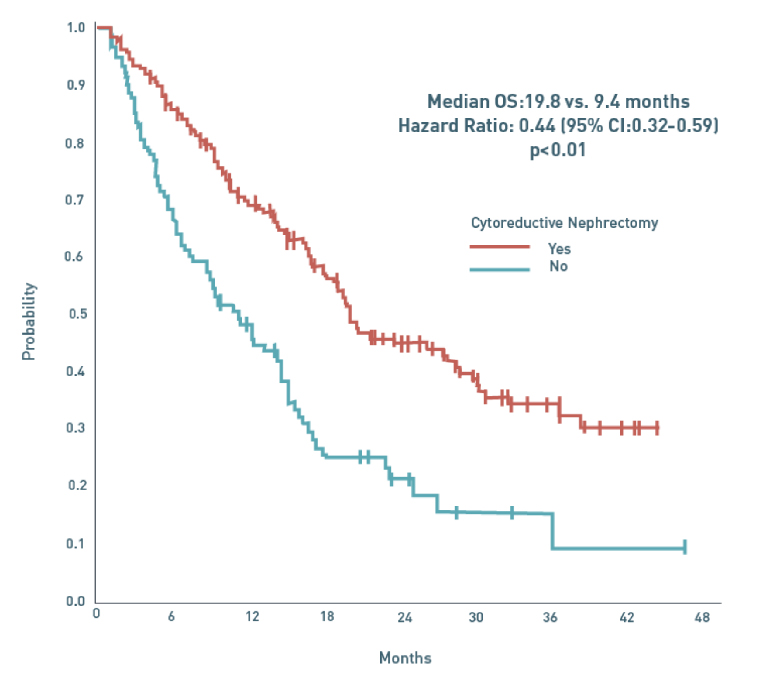
Figure 2: Overall Survival of Patients Who Did or Did Not Receive Cytoreductive Nephrectomy in Patients Receiving TK1 Therapy Era
This graph depicts overall survival from initiation of VEGF (Vascular endothelial growth factor) targeted therapy for 314 patients who did or did not receive cytoreductive nephrectomy. The median survival for those who received CNx was 19.8 months compared to 9.4 months for those who did not receive CNx. (Source: Choueiri, et al.)
Although targeted therapies are effective and usually well-tolerated by patients, they are not a cure.
Another concern is that many tumors eventually develop resistance to targeted therapies. Theoretically, surgically removing the primary tumor reduces the tumor burden, diminishes the primary tumor’s suppression of the immune system and can delay disease progression by removing growth promoters and angiogenic factors.
“If you treat with targeted therapy alone and the disease progresses, you may put patients out of the window of opportunity where the surgery has a great impact,” says Dr. Blute. “The major concern is to identify patients who will not benefit from cytoreductive nephrectomy, as up to 17-20% of patients with metastatic disease will rapidly progress. Improved understanding of risk factors, surgical indication and overall health of patients will improve patient selection. Ultimately, molecular signals may help personalize options for these patients.”
Mass General Urology works with a multidisciplinary team of oncologists to determine the best course for the management of each patient’s metastatic renal cell carcinoma.
Evidence Needed to Test Timing of Targeted Therapies Combined with Surgery
The role of presurgical targeted therapy is the subject of ongoing trials: SURITIME (NCT01099423) and CARMENA (NCT00930033). These two widely-cited European trials are testing whether targeted cancer therapy is most effective before or after cytoreductive nephrectomy. A few studies, including those published in European Urology and Annals of Oncology, have assessed the safety of presurgical targeted therapy (bevacizumab or sunitinib) and found no difference in complications between patients receiving and not receiving presurgical targeted therapy.
Regardless of the outcome of those trials, the takeaway for physicians should be that cytoreductive nephrectomy can improve the chances of patients with metastatic disease. “Targeted therapies are not cures,” says Dr. Blute, “and surgery can provide an independent strong survival advantage to these patients.”
Learn more about the Department of Urology
Refer a patient to the Department of Urology