Improving the Safety of Vena Caval Thrombectomy in Kidney Cancer with Tumor Thrombus Team Approach
In This Article
- A new multidisciplinary tumor thrombus team enlists cardiothoracic, urologic and vascular surgical expertise at Massachusetts General Hospital
- Extensive involvement by genitourinary, radiology, cardiovascular and anesthesiology teams improves outcomes for the high-risk and complex tumor thrombus excision surgery
- Combination surgeries are performed if necessary, with the tumor excision surgery performed with cardiac repair surgery in a number of recent cases to prevent a post-surgical cardiac event
Subscribe to the latest updates from Urology Advances in Motion
Up to 30% of patients with advanced renal cell carcinoma (RCC) have venous tumor invasion resulting in a tumor thrombus. Complete removal of these thrombi is essential for eliminating the cancer, but the surgical process can be dangerous, with a significant risk of hemorrhage, unstable hemodynamics and death.
A multispecialty tumor thrombus team within an integrated practice can improve the safety of this intricate and extensive procedure. Since 2016, a new tumor thrombus team at Massachusetts General Hospital has jointly managed dozens of patients with advanced RCC tumor thrombi, and all patients treated by the team have experienced improved safety.
A Specialized Team Approach
When advanced RCC invades the renal vein, it extends to the inferior vena cava (IVC), above the level of the liver and/or the heart (Figure 1).
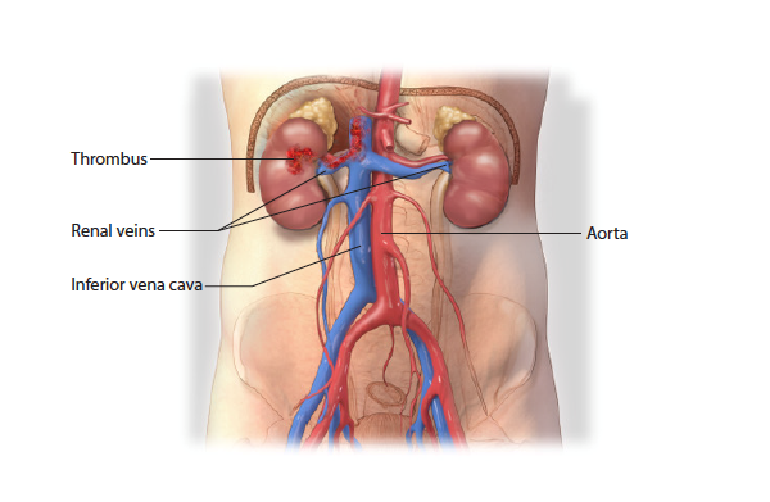
Figure 1: Normal Kidney and Inferior Vena Cava Anatomy
In advanced RCC, cancer can spread from the kidney, through the renal vein, into the inferior vena cava, upward above the diaphragm into the heart.
The complications of treating advanced RCC tumor thrombus can be considerable. The surgical team needs to be prepared for extensive blood loss or cardiovascular events resulting from changes in hemodynamics.
“A specialized team absolutely gives the patient the best chance of recovery,” says Michael Blute, MD, chief of the Department of Urology at Massachusetts General Hospital. Thoralf Sundt, MD, director of the Corrigan Minehan Heart Center at Mass General and chief of the Division of Cardiac Surgery, adds that training urologic surgeons, cardiothoracic surgeons, vascular surgeons, anesthesiologists and radiologists to work together on the intricacies of these procedures “adds a margin of safety to what is a complex and high-risk procedure.”
Francis McGovern, MD, another member of the tumor thrombus team in the Department of Urology, adds that “many patients with vena cava tumor thrombus have significant comorbidities, including cardiovascular, pulmonary and advanced age. All must be optimized in an expedited manner by the tumor thrombus team to achieve optimal outcomes in a high-risk surgery.”
Multidisciplinary Pre-Operative Planning
Even before the operation, the team conducts pre-operative cardiac assessment and imaging studies to gain as much insight into each case as possible, with the goal of avoiding surgical surprises and ensuring the best possible outcomes. This is especially important for resection of high-grade RCC in the IVC. Once admitted for surgery, patients undergo cardiopulmonary assessment, anticoagulation and imaging of the lesion. The IVC is the largest vein in the body and can become occluded within 48 hours from a tumor thrombus.
“Once we have diagnosed it, we want to use the best imaging tool that can provide an accurate surgical road map,” says Mukesh Harisinghani, MD, director of Abdominal MRI within the Mass General Department of Imaging. When patients are admitted to the hospital, they receive additional imaging using protocols with MRI to accurately stage the tumor thrombus and determine the level within the IVC or heart for operative planning (Figure 2).
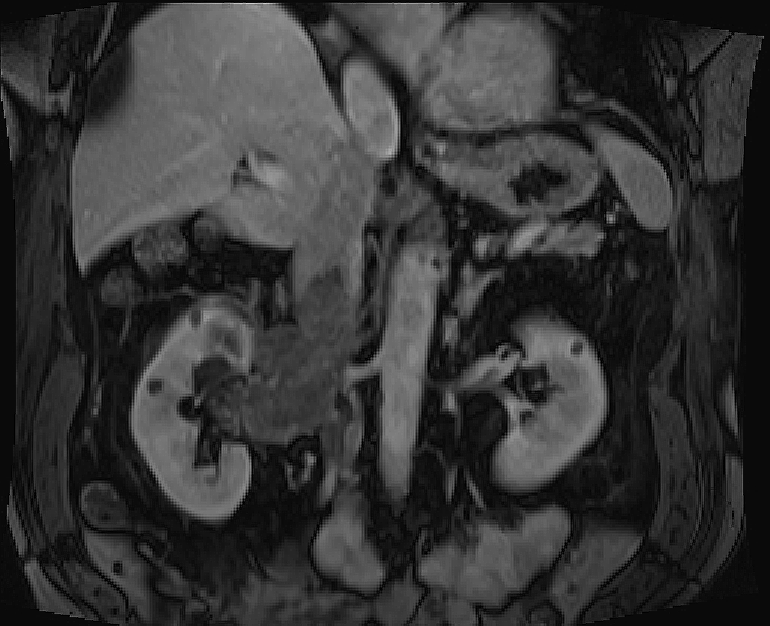
Figure 2: MRI
Coronal post contrast MRI showing extension of thrombus into renal vein and IVC.
The procedure can also present anesthetic management challenges, including intraoperative complications involving massive blood loss, or tumor or thrombus pulmonary embolization. Planning for these events also happens well before the surgery.
The team uses intraoperative transesophageal echocardiography (TEE), in which a transducer placed in the esophagus and stomach allows surgeons to monitor the surgical progress of the thrombus during the case.
“The complex nature of these tumors often requires the use of TEE to determine the location of the tumor in relation to the heart as well as assessment of the safety of surgical manipulation and tumor removal,” says Michael G. Fitzsimons, MD, director of Cardiac Anesthesia in the Department of Anesthesia, Critical Care and Pain Medicine at Mass General. "TEE serves as a valuable adjunct to the other cardiovascular monitors placed by the cardiac anesthesiologist and significantly contributes to the safety of our patients." TEE is used after the resection as well, to be sure the thrombus is completely removed (Figure 3).
Figure 3: Excision of Tumor Thrombus
Excision of tumor thrombus visualized by TEE using cardiopulmonary bypass, hypothermia and circulatory arrest.
If the tumor is growing above the diaphragm and near the heart, the team may plan for a vascular bypass to stabilize the patient’s blood pressure and blood volume during the operation. Sometimes an extracorporeal membrane oxygenator (ECMO) is used to maintain cardiac and respiratory support.
If the tumor thrombus is in the heart itself, the team uses cardiopulmonary bypass techniques, allowing the cardiac surgeon time to perform an atriotomy to gain and extract the thrombus (Figure 4). This also provides the time needed after its removal to inspect the IVC and make sure that all the fragments of the tumor thrombus are gone, and to reconstruct it if necessary.

Figure 4: TUMOR THROMBUS AFTER EXCISION
Renal cancer specimen with associated tumor thrombus that reached the right atrium (level IV).
Combination Surgeries if Needed
Patients are also simultaneously screened with coronary computed tomography (CT) for heart disease. The team has combined the tumor excision surgery with a cardiac repair surgery in a number of recent cases. This can improve the likelihood that the patient will survive and not suffer a cardiac event after this major operation.
“We want the opportunity to correct valves or do coronary bypass grafting in patients who need them,” says Dr. Blute. These steps, at the intersection of several surgical specialties, have led to better outcomes. “Before this approach, the case may have fallen to a surgeon without the benefit of the most up-to-date imaging studies or access to a cardiovascular pump room,” he says. “In that environment, it becomes dangerous with a hurried approach with potential for hemorrhage, particularly in patients who have cardiac compromise. It can be a much safer operation now with efforts like this one.”
Because of the risks of hemorrhage, thrombus and cardiac events, it takes a whole team of specialists to successfully manage a patient with a tumor thrombus. With its focus on coordinated surgical and perioperative care strategies, the Mass General tumor thrombus team has established a new safety standard for this challenging surgery.
About the Department of Urology