LTVV in non-ARDS
The FLARE Four
- Low tidal volume ventilation is a cornerstone of therapy for ARDS and has a well-demonstrated mortality benefit
- Low tidal volume ventilation has also been associated with improved outcomes in non-ARDS patients
- Implementation of low tidal volume ventilation has costs in the form of increased sedation and even paralysis. These costs must be balanced against the benefits of achieving low tidal volume ventilation in a particular patient
- Given demonstrated benefits of low tidal volume ventilation in both ARDS and non-ARDS respiratory failure, it should not be assumed that protocolized use of higher tidal volumes, as has been advocated, is ever without harm
Many people are saying...we don’t need to use low tidal volume ventilation in COVID-19 patients.
Subscribe to the latest updates from FLARE Advances in Motion
Introduction
COVID-19 infection commonly leads to hypoxemic respiratory failure that falls within the spectrum of ARDS and is thus optimally managed with lung protective ventilation strategies, including low tidal volume ventilation (LTVV). However, some patients with hypoxemic respiratory failure do not meet criteria for ARDS or are suspected to have a different underlying process. In this FLARE, we discuss the possible benefits and costs of low tidal volume ventilation in ARDS and the evidence for use of LTVV in patients with non-ARDS respiratory failure.
COVID-19 Respiratory Failure is ARDS
There has been much debate throughout this pandemic about whether the hypoxemic respiratory failure resulting from COVID-19 is acute respiratory distress syndrome (ARDS) or whether it represents a novel process. Notably, ARDS is not a specific disease and is instead a clinical syndrome with significant heterogeneity in clinical severity, physiologic parameters, and histopathology (Bellani et al. 2016; Thille et al. 2013). As we have discussed previously (FLARE April 10th) and as seen in recently published physiologic data from a cohort of COVID-19 ICU patients (Ziehr et al. 2020) and pathologic studies (FLARE May 1st), COVID-19 hypoxemic respiratory failure fits well within the previously-described spectrum of ARDS. However, the claim that COVID-19 is not ARDS has also led to some strong suggestions (Gattinoni et al. 2020; “German Physician Explains Alternative Ventilation for COVID-19” 2020) about use of ventilatory strategies other than lung protective mechanical ventilation, including larger tidal volumes. Even if the weight of evidence suggests COVID-19 associated respiratory failure fits within the accepted spectrum of ARDS, it is certainly true that not all respiratory failure fits the Berlin definition of ARDS.
Should Non-ARDS Respiratory Failure Be Managed With Large Tidal Volumes?
To fully evaluate the recommendation for larger tidal volumes in COVID-19 associated respiratory failure, we must first examine the rationale and evidence for LTVV in both ARDS and non-ARDS patients.
Why Use Low Tidal Volumes in ARDS?
Low tidal volume ventilation (usually defined as ~6 ml/kg predicted body weight) is a cornerstone of ARDS therapy. The rationale for this therapy is well described but will be briefly outlined here. ARDS is characterized by a cascade of injury that includes increased endothelial permeability, an influx of protein rich fluid into alveoli, hyaline membrane formation, and alveolar instability and collapse (Thompson, Chambers, and Liu 2017). These events lead to significant heterogeneity of aeration, including areas of well-inflated lung and areas of non-aerated lung, and a smaller functional lung size. Tidal volumes delivered to the lung afflicted with ARDS are therefore often maldistributed, resulting in overdistention of already open lung even with relatively modest tidal volumes (so called volutrauma/barotrauma), or in cyclic opening and closing of those lung units that are poorly aerated (so called atelectrauma). The stress and strain experienced by the inflamed lung can also propagate further inflammation – a phenomenon known as biotrauma (Figure 1). Judicious choice of tidal volume, adjusted by predicted body weight and thereby supposed lung size, can minimize these risks. LTVV has been shown repeatedly to improve outcomes in patients with ARDS, starting with the landmark ARDSnet ARMA trial (Acute Respiratory Distress Syndrome Network et al. 2000).
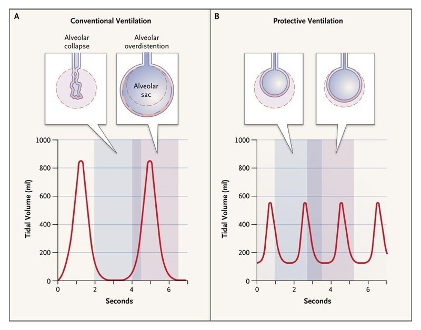
Figure 1
Conventional Ventilation as Compared with Protective Ventilation (Malhotra 2007).
Low Tidal Volume Ventilation Does Not Guarantee Lung Protective Ventilation
It is important to note that low tidal volume ventilation alone does not guarantee lung protection, and that even with low tidal volumes there can be cyclic opening and closing of inflamed lung and overdistention of a very small functional lung. Judiciously titrating positive end-expiratory pressure (PEEP) can prevent derecruitment, thus increasing functional lung size and reducing the risk of both volutrauma and atelectrauma. In addition to tidal volume, physiologic metrics such as plateau pressure, driving pressure, and static compliance yield additional information about how well matched the tidal volume and PEEP are to a patient’s individual respiratory system mechanics. As personalization of mechanical ventilation based on recruitability and functional lung size is a topic of its own, here we will focus specifically on the use of low tidal volumes as the cornerstone of lung protective ventilation.
Evidence for LTVV in non-ARDS Patients
The rationale for low tidal volume ventilation is not limited to patients who fit the definition of ARDS. Specifically, localized inflammation and aeration inhomogeneity, as well as the potential for biotrauma, are present in many other conditions including pneumonia, trauma, and some cases of cardiogenic pulmonary edema. It is therefore natural to ask whether non-ARDS patients should also receive low tidal volume ventilation.
Epidemiologic data suggest that widespread adoption of low tidal volume ventilation, among other developments in critical care, has benefitted patients. In the years since the landmark ARDSnet trial, hospital-acquired ARDS has been on the decline while community-acquired ARDS remains stable, suggesting we are converting fewer patients with other problems into ARDS patients with harmful ventilation (Figure 2, adapted from Li et al. 2011).
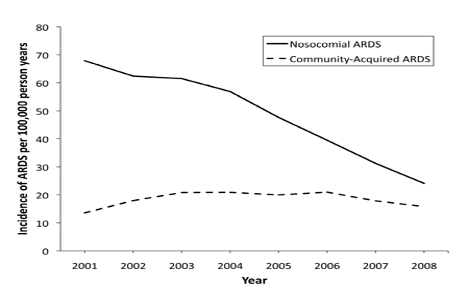
Figure 2
Comparison of incidence of nosocomial ARDS versus community-acquired ARDS. Adapted from Li et al. 2011, courtesy of Dr. B. Taylor Thompson.
There are also many observational studies that have found an association between higher tidal volumes and development of lung injury in patients who are mechanically ventilated for a variety of reasons other than ARDS. One study examined patients who did not fit ARDS criteria at the time of intubation who subsequently fulfilled Berlin criteria and found that high tidal volume was an independent predictor of developing ARDS, with a dose-related OR of 1.3 for each ml/kg above 6 ml/kg predicted body weight (Gajic et al. 2004). An important insight from a follow-up study of a larger cohort was that in the small percentage of patients who received high tidal volumes and went on to develop ARDS, initial compliance was high – suggesting that compliance is not a good predictor of risk for lung injury (Gajic et al. 2005). Additional retrospective studies have shown an association between higher tidal volumes and development of acute lung injury in critically ill patients with brain injury (Mascia et al. 2007) and in surgical patients (Ladha et al. 2015). Several additional meta-analyses have confirmed the association between high tidal volumes and development of lung injury, higher mortality, longer length of stay, and pulmonary complications as a composite endpoint (Serpa Neto et al. 2012, 2014, 2015).
Although there have been no large randomized controlled trials to look at the impact of low tidal volume ventilation in the non-ARDS population, several smaller interventional trials are notable. These include a high profile study in surgical patients undergoing major abdominal surgery, which demonstrated a significantly greater incidence of complications (27% vs. 10%) in those who received high tidal volume intra-operatively than those who received low tidal volumes (Futier et al. 2013). Complications included a higher incidence of postoperative mechanical ventilation and longer length of stay. Another study in ICU patients without lung injury was stopped early after the higher tidal volume group was observed to be at greater risk of developing lung injury compared to the low tidal volume group (13.5 v 2.6%) (Determann et al. 2010).
As these representative studies demonstrate, there is a strong signal that higher tidal volumes may result in lung injury in many different types of patients. This begs the question – why do we not use LTVV across the board?
Hazards of Low Tidal Volume Ventilation
Despite the firm physiologic rationale and demonstrated benefit of LTVV, it does not come without potential costs to the patient. Setting aside the question of whether to intubate a patient with ARDS to ensure LTVV (a topic that deserves its own nuanced discussion), once patients are intubated, the imposition of stringent low tidal volumes often requires significant sedation and, at times, paralysis. Analgesia, sedation, and paralysis can prevent patient-ventilator asynchrony by suppressing respiratory drive and/or effort. Patient-ventilator asynchrony can result in ventilator-induced lung injury and is associated with worsened outcomes (Blanch et al. 2015). However, sedation and paralysis are also associated with many immediate and long-term sequelae. For example, use of deep sedation can be complicated by hemodynamic instability, decreased gut motility, hypertriglyceridemia and pancreatitis, and drug interactions, to name a few (as discussed in FLARE from May 2nd; Hanidziar and Bittner 2020). Sedation in general, and specific classes of medications including benzodiazepines, are also associated with delirium and longer term cognitive deficits (Salluh et al. 2015; Sasannejad, Ely, and Lahiri 2019). In a paradox not uncommon in ICU care, use of sedation intended to achieve LTVV and avoid higher tidal volumes has been associated with worse outcomes can lead to delirium, an independent predictor of mortality in ICU patients (Ely et al. 2004). In the absence of large randomized trials that examine this dilemma (benefits of LTVV weighed against risks of pharmacologic measures to support LTVV), it is left to the clinician to reconcile these data.
Use of low tidal volumes can also limit the ability to achieve adequate gas exchange. At a tidal volume of 6 cc/kg predicted body weight or below, higher respiratory rates are typically required to deliver a minute ventilation that matches the patient’s metabolic demands. One approach is to accept some degree of hypercapnia and associated mild respiratory acidosis. These metabolic derangements are typically well tolerated but can become more problematic in patients with concomitant metabolic acidosis and in those with specific concerns about hypercapnia such as an increased intracranial pressure. Additionally, in patients with severe obstructive lung disease, the increased respiratory rate required to normalize minute ventilation can result in dynamic hyperinflation and auto-PEEP. Therefore, the uniform application of LTVV to all patients may result in harm (Davies, Senussi, and Mireles-Cabodevila 2016).
What Should We Do at the Bedside?
Clinicians are faced with a wealth of data about the risk of high tidal volumes, not only in patients with ARDS but also in those who are intubated for other indications. Critical care providers must also simultaneously contend with the risks associated with implementation of LTVV, including increased intensity of critical care and associated potential complications, as well as individual circumstances that may lead to poor tolerance of LTVV. Thus, an individualized decision for each patient about tidal volume and other parameters of mechanical ventilation is necessary – this decision should take into account patient-specific factors such as frailty and risk of complications, duration of illness and patient trajectory, and concomitant risk factors for ARDS such as infection and inflammatory state. As in many aspects of critical care, the art of medicine is thoughtful application of the available data to the patient in front of us.
Conclusion
The use of low tidal volumes is potentially preferred in any situation characterized by heterogeneous inflation and pulmonary inflammation. This assertion is based on reasonably strong evidence for its benefit in non-ARDS respiratory failure. LTVV, however, is not without cost. The increased sedation that frequently accompanies LTVV has itself been associated with poorer outcomes. There is clearly a need for careful clinical assessment in order to balance these risks. What is clear, however, is that there is a role of LTVV in non-ARDS respiratory failure at least in some patients. To declare that any large group of patients with respiratory failure (whether due to SARS CoV-2 or another insult), should universally receive high tidal volumes is to ignore the potential to do harm.
References:
- Acute Respiratory Distress Syndrome Network, Roy G. Brower, Michael A. Matthay, Alan Morris, David Schoenfeld, B. Taylor Thompson, and Arthur Wheeler. 2000. “Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome.” The New England Journal of Medicine 342 (18): 1301–8.
- Bellani, Giacomo, John G. Laffey, Tài Pham, Eddy Fan, Laurent Brochard, Andres Esteban, Luciano Gattinoni, et al. 2016. “Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries.” JAMA: The Journal of the American Medical Association 315 (8): 788–800.
- Blanch, Lluís, Ana Villagra, Bernat Sales, Jaume Montanya, Umberto Lucangelo, Manel Luján, Oscar García-Esquirol, et al. 2015. “Asynchronies during Mechanical Ventilation Are Associated with Mortality.” Intensive Care Medicine 41 (4): 633–41.
- Davies, John D., Mourad H. Senussi, and Eduardo Mireles-Cabodevila. 2016. “Should A Tidal Volume of 6 mL/kg Be Used in All Patients?” Respiratory Care 61 (6): 774–90.
- Determann, Rogier M., Annick Royakkers, Esther K. Wolthuis, Alexander P. Vlaar, Goda Choi, Frederique Paulus, Jorrit-Jan Hofstra, Mart J. de Graaff, Johanna C. Korevaar, and Marcus J. Schultz. 2010. “Ventilation with Lower Tidal Volumes as Compared with Conventional Tidal Volumes for Patients without Acute Lung Injury: A Preventive Randomized Controlled Trial.” Critical Care / the Society of Critical Care Medicine 14 (1): R1.
- Ely, E. Wesley, Ayumi Shintani, Brenda Truman, Theodore Speroff, Sharon M. Gordon, Frank E. Harrell Jr, Sharon K. Inouye, Gordon R. Bernard, and Robert S. Dittus. 2004. “Delirium as a Predictor of Mortality in Mechanically Ventilated Patients in the Intensive Care Unit.” JAMA: The Journal of the American Medical Association 291 (14): 1753–62.
- Futier, Emmanuel, Jean-Michel Constantin, Catherine Paugam-Burtz, Julien Pascal, Mathilde Eurin, Arthur Neuschwander, Emmanuel Marret, et al. 2013. “A Trial of Intraoperative Low-Tidal-Volume Ventilation in Abdominal Surgery.” The New England Journal of Medicine 369 (5): 428–37.
- Gajic, Ognjen, Saqib I. Dara, Jose L. Mendez, Adebola O. Adesanya, Emir Festic, Sean M. Caples, Rimki Rana, et al. 2004. “Ventilator-Associated Lung Injury in Patients without Acute Lung Injury at the Onset of Mechanical Ventilation.” Critical Care Medicine 32 (9): 1817–24.
- Gajic, Ognjen, Fernando Frutos-Vivar, André Esteban, Rolf D. Hubmayr, and Antonio Anzueto. 2005. “Ventilator Settings as a Risk Factor for Acute Respiratory Distress Syndrome in Mechanically Ventilated Patients.” Intensive Care Medicine 31 (7): 922–26.
- Gattinoni, Luciano, Davide Chiumello, Pietro Caironi, Mattia Busana, Federica Romitti, Luca Brazzi, and Luigi Camporota. 2020. “COVID-19 Pneumonia: Different Respiratory Treatments for Different Phenotypes?” Intensive Care Medicine, April. https://doi.org/10.1007/s00134-020-06033-2.
- Gattinoni, Luciano, and Alessandro Protti. 2008. “Ventilation in the Prone Position: For Some but Not for All?” CMAJ: Canadian Medical Association Journal = Journal de l’Association Medicale Canadienne.
- “German Physician Explains Alternative Ventilation for COVID-19.” 2020. Medscape. April 28, 2020. https://www.medscape.com/viewarticle/929609.
- Hanidziar, Dusan, and Edward Bittner. 2020. “Sedation of Mechanically Ventilated COVID-19 Patients: Challenges and Special Considerations.” Anesthesia & Analgesia Publish Ahead of Print (April). https://doi.org/10.1213/ANE.0000000000004887.
- Ladha, Karim, Marcos F. Vidal Melo, Duncan J. McLean, Jonathan P. Wanderer, Stephanie D. Grabitz, Tobias Kurth, and Matthias Eikermann. 2015. “Intraoperative Protective Mechanical Ventilation and Risk of Postoperative Respiratory Complications: Hospital Based Registry Study.” BMJ 351 (July): h3646.
- Li, Guangxi, Michael Malinchoc, Rodrigo Cartin-Ceba, Chakradhar V. Venkata, Daryl J. Kor, Steve G. Peters, Rolf D. Hubmayr, and Ognjen Gajic. 2011. “Eight-Year Trend of Acute Respiratory Distress Syndrome: A Population-Based Study in Olmsted County, Minnesota.” American Journal of Respiratory and Critical Care Medicine 183 (1): 59–66.
- Malhotra, Atul. 2007. “Low-Tidal-Volume Ventilation in the Acute Respiratory Distress Syndrome.” The New England Journal of Medicine 357 (11): 1113–20.
- Mascia, Luciana, Elisabeth Zavala, Karen Bosma, Daniela Pasero, Daniela Decaroli, Peter Andrews, Donatella Isnardi, et al. 2007. “High Tidal Volume Is Associated with the Development of Acute Lung Injury after Severe Brain Injury: An International Observational Study.” Critical Care Medicine 35 (8): 1815–20.
- Salluh, Jorge I. F., Han Wang, Eric B. Schneider, Neeraja Nagaraja, Gayane Yenokyan, Abdulla Damluji, Rodrigo B. Serafim, and Robert D. Stevens. 2015. “Outcome of Delirium in Critically Ill Patients: Systematic Review and Meta-Analysis.” BMJ 350 (June): h2538.
- Sasannejad, Cina, E. Wesley Ely, and Shouri Lahiri. 2019. “Long-Term Cognitive Impairment after Acute Respiratory Distress Syndrome: A Review of Clinical Impact and Pathophysiological Mechanisms.” Critical Care / the Society of Critical Care Medicine 23 (1): 352.
- Serpa Neto, Ary, Sérgio Oliveira Cardoso, José Antônio Manetta, Victor Galvão Moura Pereira, Daniel Crepaldi Espósito, Manoela de Oliveira Prado Pasqualucci, Maria Cecília Toledo Damasceno, and Marcus J. Schultz. 2012. “Association between Use of Lung-Protective Ventilation with Lower Tidal Volumes and Clinical Outcomes among Patients without Acute Respiratory Distress Syndrome: A Meta-Analysis.” JAMA: The Journal of the American Medical Association 308 (16): 1651–59.
- Serpa Neto, Ary, Sabrine N. T. Hemmes, Carmen S. V. Barbas, Martin Beiderlinden, Michelle Biehl, Jan M. Binnekade, Jaume Canet, et al. 2015. “Protective versus Conventional Ventilation for Surgery: A Systematic Review and Individual Patient Data Meta-Analysis.” Anesthesiology 123 (1): 66–78.
- Serpa Neto, Ary, Fabienne D. Simonis, Carmen S. V. Barbas, Michelle Biehl, Rogier M. Determann, Jonathan Elmer, Gilberto Friedman, et al. 2014. “Association between Tidal Volume Size, Duration of Ventilation, and Sedation Needs in Patients without Acute Respiratory Distress Syndrome: An Individual Patient Data Meta-Analysis.” Intensive Care Medicine 40 (7): 950–57.
- Thille, Arnaud W., Andrés Esteban, Pilar Fernández-Segoviano, José-Maria Rodriguez, José-Antonio Aramburu, Oscar Peñuelas, Irene Cortés-Puch, Pablo Cardinal-Fernández, José A. Lorente, and Fernando Frutos-Vivar. 2013. “Comparison of the Berlin Definition for Acute Respiratory Distress Syndrome with Autopsy.” American Journal of Respiratory and Critical Care Medicine 187 (7): 761–67.
- Thompson, B. Taylor, Rachel C. Chambers, and Kathleen D. Liu. 2017. “Acute Respiratory Distress Syndrome.” The New England Journal of Medicine.
- Ziehr, David R., Jehan Alladina, Camille R. Petri, Jason H. Maley, Ari Moskowitz, Benjamin D. Medoff, Kathryn A. Hibbert, B. Taylor Thompson, and C. Corey Hardin. 2020. “Respiratory Pathophysiology of Mechanically Ventilated Patients with COVID-19: A Cohort Study.” American Journal of Respiratory and Critical Care Medicine, April. https://doi.org/10.1164/rccm.202004-1163LE.
Learn more about research in the Division of Pulmonary and Critical Care Medicine
View all COVID-19 updates