Cardiac Arrest and COVID-19
The FLARE Four
- Early reports from China indicated very poor outcomes with cardiac arrest in COVID-19
- These reports likely reflected a high prevalence of factors such as primary respiratory (as opposed to cardiac) arrest and out-of-ICU arrest, which were known to worsen prognosis in the pre-COVID-19 era
- Cardiac arrest in COVID-19 does present unique infection control challenges which are addressed by national guidelines
- Post-arrest care does not meaningfully differ from post-arrest care in the pre-COVID-19 era
Many people are asking...how should we approach cardiopulmonary resuscitation in COVID-19?
Subscribe to the latest updates from FLARE Advances in Motion
Introduction
In-hospital cardiac arrest (IHCA) during the COVID-19 pandemic presents a unique set of resuscitation challenges such as exposure risk to clinical providers and obstacles to family communication. In this FLARE, we provide a brief review of IHCA in the pre-COVID-19 era and then discuss emerging evidence regarding IHCA during the COVID-19 pandemic.
IHCA in the Pre-COVID-19 Era
IHCA is a common and highly morbid event affecting over 290,000 adults in the United States each year (Holmberg et al. 2019). IHCA survival rates have been increasing over the past two decades across all age groups from approximately 17% in 2000 to 25% in 2016 (Wiberg et al. 2020). Even among elderly patients, those IHCA survivors who are discharged from the hospital have a >50% likelihood of being alive at 1-year (Chan et al. 2013). While no specific pharmacologic therapy has been shown to improve IHCA survival, declining mortality rates likely relate to a focus on resuscitation quality and post-arrest critical care.
A number of studies have found that certain aspects of intra-arrest resuscitation quality are tightly associated with outcome. In particular, a focus on early and effective chest compressions (Bircher et al. 2019), reducing time to first defibrillation in patients with an initial shockable rhythms (Chan et al. 2008), and reducing time to epinephrine in patients with initial non-shockable rhythms (Chan et al. 2008) improve outcomes. For patients who remain comatose after return of spontaneous circulation (ROSC), there is evidence that utilizing targeted temperature management (Lascarrou et al. 2019), and potentially avoiding hyperoxia (Kilgannon et al. 2010) (although this finding should be considered hypothesis-generating) can improve post-IHCA outcomes.
IHCA Epidemiology in the Time of COVID-19
Data regarding IHCA during the COVID-19 pandemic remain sparse. In one case series of 136 SARS-CoV-2 positive patients who experienced IHCA in Wuhan, China, the outcomes were quite poor with just 18 (13.2%) patients achieving ROSC, four (2.9%) patients surviving to 30 days, and one (<1%) achieving a favorable neurological outcome by 30 days (Shao et al. 2020). Compared to large IHCA cohorts prior to COVID-19, these outcomes are substantially worse and have resulted in some suggestion that outcomes of COVID-19 IHCA are uniquely poor. Diving into this data, these outcomes may have been driven by a number of factors. First, as compared to patients prior to COVID-19 where the most common etiology of IHCA is cardiac (Wallmuller et al. 2012; Perman et al. 2016), in this cohort the most common etiology of IHCA was respiratory. In addition, a large percent of COVID-19 related IHCA occurred on the medical wards (>80%), compared to >50% occurring in ICUs in prior American cohorts (Perman et al. 2016). Thirdly, the presenting rhythm was asystole (a rhythm associated with overall worse prognosis) in 90% of patients in the Wuhan cohort, compared to 40% in pre-COVID-19 cohorts (Perman et al. 2016).
Non-cardiac etiology of arrest, asystole as initial rhythm, and arrest occurrence on an unmonitored ward are all associated with lower survival after IHCA and were all much more common in the COVID-19 cohort described (Shao et al. 2020). Some of these factors, such as the frequency of a respiratory etiology, may not be modifiable given the nature of COVID-19. Others, however, such as the percentage of arrests that occur in an ICU or that present with asystole (as asystole often occurs when arrests are unwitnessed and pre-CPR downtime is longer), may be modifiable with improved surge planning and ICU capacity. While IHCA outcomes in this cohort were quite poor, it is a single experience that does not match with general pre-COVID-19 IHCA characteristics or outcomes and more data is needed.
IHCA Prevention
As compared to out-of-hospital arrests, in-hospital arrests offer an opportunity for prevention. This can either come from earlier detection and interception of clinical deterioration, or recognition that cardiopulmonary resuscitation is not concordant with a patient’s goals of care. Indeed, in their interim guidance described in detail below, the AHA has emphasized the importance of addressing advanced directives and goals of care at hospital admission for all COVID-19 patients (Edelson et al. 2020).
A particularly relevant opportunity for prevention in the COVID-19 era is avoiding delays in intubation for respiratory failure. This form of preventability is often related to a patient with adequate oxygenation, but who has other signs of clinical deterioration such as increased work of breathing, worsening hemodynamic instability, or progressive acidemia (Moskowitz et al. 2019).
Interim Guidance on Resuscitation Practices
Due to the potential for transmission of infection to healthcare workers during resuscitation of a COVID-19 patient, the American Heart Association (AHA) and the International Liaison Committee on Resuscitation (ILCOR) have published interim adjustments and commentary on their guidelines and treatment recommendations (Edelson et al. 2020). ILCOR also performed a systematic review to evaluate the risk of infection transmission during resuscitation, as well as the impact of wearing PPE on resuscitation performance measures. This review identified conflicting results but limited observational evidence of increased risk of infection in healthcare workers performing CPR on SARS patients (compared to healthcare workers who had not performed CPR in this setting) (Couper et al. 2020). A mannequin study found time-to-perform various resuscitation measures was slightly longer when PPE was utilized. The AHA, similar to ILCOR, concluded that, “the administration of CPR involves performing numerous aerosol-generating procedures, including chest compressions, positive pressure ventilation, and establishment of an advanced airway” (Edelson et al. 2020). The AHA additionally provides an updated advanced cardiac life support (ACLS) algorithm for use during the COVID-19 era (Figure 1).
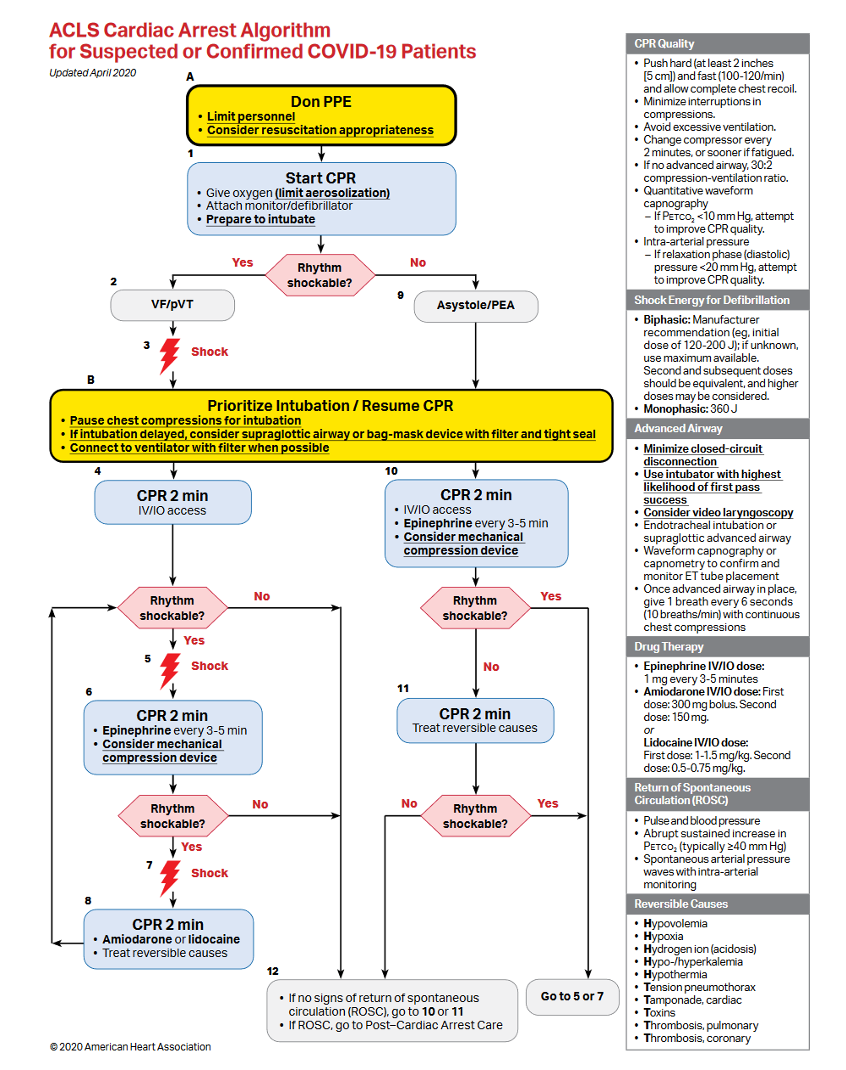
Figure 1
ACLS cardiac arrest algorithm for suspected or confirmed patients with SARS-CoV-2 infection (Edelson et al. 2020).
Key Updates to the ACLS Algorithm
- Ensure all providers are wearing appropriate personal protective equipment (PPE) for aerosol-generating procedures upon entering the room
- Limit personnel in the room
- If available, and there are protocols in place for use, consider a mechanical CPR device as opposed to hands-on CPR. This will allow for a decreased number of resuscitators in the room
- Prioritize endotracheal intubation after assessing for and defibrillating and shockable rhythm
- If using a bag-valve mask or supraglottic airway prior to intubation, consider attaching a HEPA filter in the path of exhaled gas
- Maximize the chances of first pass endotracheal intubation
- Pause compressions during intubation
- Have the most experienced airway provider perform the intubation
- Consider video-laryngoscopy which allows a greater distance from the patient’s airway
- After intubation, ensure the cuff is inflated and a HEPA filter is in the path of exhaled gas
Chest Compressions in the COVID-19 Era
In a recent simulation study using both mannequin and cadaver models, authors found that chest compressions can result in aerosol generation, with the direction of aerosol production towards the clinician performing chest compressions. In addition, a simple surgical facemask on the mannequin or cadaver did not reliably prevent aerosol formation (Ott et al. 2020). This simulation study has substantial face validity given that chest compressions are likely to generate substantial exhaled air flows (although there is little published data on this topic). Notably, a supraglottic device with a viral filter was effective in limiting aerosol generation. While this is concerning and appropriate precautions should be taken, it is unclear if aerosols generated during procedures produce infectious virus (as discussed in a prior FLARE).

Figure 2
Aerosol spread (as indicated by white plume arising from mannequin’s mouth) during chest compressions (Ott et al. 2020).
While mechanical CPR devices have previously been shown to improve compression quality as compared to hands-on CPR, they have not been shown to improve outcomes and are therefore not recommended for standard use in the in-hospital setting (Poole et al. 2018). Both the AHA and ILCOR however have previously suggested mechanical CPR in scenarios where manual CPR may be difficult to maintain or pose a risk to providers, and these organizations have suggested that COVID-19 meets these criteria. They therefore suggest the use of mechanical CPR devices for resuscitation of COVID-19 patients if available and there are protocols in place for their use.
Airway Management in the COVID-19 era
Even before COVID-19, airway management during cardiac arrest was a hotly debated and researched topic. Three randomized trials, all conducted in the out-of-hospital arrest setting, found that bag-valve mask and supraglottic airways were similar or superior to intra-arrest endotracheal intubation (Granfeldt et al. 2019). With respect to in-hospital arrest, an observational study found that intra-arrest endotracheal intubation is associated with worse outcomes as compared to no endotracheal intubation (Andersen et al. 2017); however this study may be confounded by indication. The 2019 AHA ACLS update recommended that either bag-valve mask or an advanced airway can be used during resuscitation. Further, if an advanced airway is used, either endotracheal or supraglottic airways can be chosen--largely on the basis of provider experience with endotracheal intubation (Panchal et al. 2019).
Given the concerns detailed above regarding aerosol generation during chest compressions and known risks regarding the generation of aerosols with non-invasive positive pressure ventilation (reviewed in a prior FLARE), the interim guidance from the AHA and ILCOR recommend early endotracheal intubation to be done by the most experienced provider. Chest compressions should be paused to increase the odds of first pass success and minimize aerosol generation while the intubator is closest to the airway. Finally, a HEPA filter should be placed in the path of any exhaled gas.
Resuscitation in the Prone Position
Prone positioning is a well described therapy for moderate/severe acute respiratory distress syndrome. The AHA document specifically addresses resuscitation of patients who arrest while in the prone position. The statement suggests that in an intubated patient, rescuers should consider leaving the patient prone and conducting CPR and defibrillation in that position. However, it must be noted that this is based on virtually no evidence. Data for prone CPR consist of case reports only, with a systematic review of these identifying only one case of a patient proned in an ICU for respiratory failure, while the other 22 cases were patients in the operating room who could not be supinated for operative reasons (Brown, Rogers, and Soar 2001).
As CPR and defibrillation, which have been extensively studied in the supine and not the prone position, are by far the most life-saving interventions for cardiac arrest, and as hospitals where proning is used frequently are capable of rapidly turning a patient, practitioners should consider immediate supination as soon as feasible if the appropriate expertise and resources are available.
Post-arrest Care
Care of the COVID-19 patient following ROSC should not differ from that of resuscitated IHCA victims in the pre-COVID-19 era. This should include exploration regarding the cause of arrest, careful attention to established critical care practices, targeted temperature management to a goal temperature between 32-36°C if the patient remains comatose, and delayed neurologic prognosis until at least 72 hours after rewarming.
Conclusions
IHCA is a highly morbid event, however outcomes have improved over time. Cardiac arrest in the setting of COVID-19 poses unique challenges which include the need to protect health care workers responding to cardiac arrest. COVID-19 specific treatment recommendations stress the need to don PPE (acknowledging the possible delay in provision of CPR), consider early endotracheal intubation, and minimize the number of responded personnel in the room facilitated by the use of automated chest compression devices. IHCA in COVID-19 is more likely to be due primarily to respiratory failure than cardiac etiology--this may impact prognosis and highlights the need for early, aggressive respiratory support to reverse the underlying etiology.
References
- Andersen, Lars W., Asger Granfeldt, Clifton W. Callaway, Steven M. Bradley, Jasmeet Soar, Jerry P. Nolan, Tobias Kurth, Michael W. Donnino, and American Heart Association’s Get With The Guidelines–Resuscitation Investigators. 2017. “Association Between Tracheal Intubation During Adult In-Hospital Cardiac Arrest and Survival.” JAMA: The Journal of the American Medical Association 317 (5): 494–506.
- Bircher, Nicholas G., Paul S. Chan, Yan Xu, and American Heart Association’s Get With The Guidelines–Resuscitation Investigators. 2019. “Delays in Cardiopulmonary Resuscitation, Defibrillation, and Epinephrine Administration All Decrease Survival in In-Hospital Cardiac Arrest.” Anesthesiology 130 (3): 414–22.
- Brown, J., J. Rogers, and J. Soar. 2001. “Cardiac Arrest during Surgery and Ventilation in the Prone Position: A Case Report and Systematic Review.” Resuscitation 50 (2): 233–38.
- Chan, Paul S., Harlan M. Krumholz, Graham Nichol, Brahmajee K. Nallamothu, and American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. 2008. “Delayed Time to Defibrillation after in-Hospital Cardiac Arrest.” The New England Journal of Medicine 358 (1): 9–17.
- Chan, Paul S., Brahmajee K. Nallamothu, Harlan M. Krumholz, John A. Spertus, Yan Li, Bradley G. Hammill, Lesley H. Curtis, and American Heart Association Get with the Guidelines–Resuscitation Investigators. 2013. “Long-Term Outcomes in Elderly Survivors of in-Hospital Cardiac Arrest.” The New England Journal of Medicine 368 (11): 1019–26.
- Couper, Keith, Sian Taylor-Phillips, Amy Grove, Karoline Freeman, Osemeke Osokogu, Rachel Court, Amin Mehrabian, et al. 2020. “COVID-19 in Cardiac Arrest and Infection Risk to Rescuers: A Systematic Review.” Resuscitation. https://doi.org/10.1016/j.resuscitation.2020.04.022.
- Edelson, Dana P., Comilla Sasson, Paul S. Chan, Dianne L. Atkins, Khalid Aziz, Lance B. Becker, Robert A. Berg, et al. 2020. “Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get With the Guidelines®-Resuscitation Adult and Pediatric Task Forces of the American Heart Association in Collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, The Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists: Supporting Organizations: American Association of Critical Care Nurses and National EMS Physicians.” Circulation, April. https://doi.org/10.1161/CIRCULATIONAHA.120.047463.
- Granfeldt, Asger, Suzanne R. Avis, Tonia C. Nicholson, Mathias J. Holmberg, Ari Moskowitz, Amin Coker, Katherine M. Berg, et al. 2019. “Advanced Airway Management during Adult Cardiac Arrest: A Systematic Review.” Resuscitation 139 (June): 133–43.
- Holmberg, Mathias J., Catherine E. Ross, Garrett M. Fitzmaurice, Paul S. Chan, Jordan Duval-Arnould, Anne V. Grossestreuer, Tuyen Yankama, Michael W. Donnino, Lars W. Andersen, and American Heart Association’s Get With The Guidelines–Resuscitation Investigators. 2019. “Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States.” Circulation. Cardiovascular Quality and Outcomes 12 (7): e005580.
- Kilgannon, J. Hope, Alan E. Jones, Nathan I. Shapiro, Mark G. Angelos, Barry Milcarek, Krystal Hunter, Joseph E. Parrillo, Stephen Trzeciak, and Emergency Medicine Shock Research Network (EMShockNet) Investigators. 2010. “Association between Arterial Hyperoxia Following Resuscitation from Cardiac Arrest and in-Hospital Mortality.” JAMA: The Journal of the American Medical Association 303 (21): 2165–71.
- Lascarrou, Jean-Baptiste, Hamid Merdji, Amélie Le Gouge, Gwenhael Colin, Guillaume Grillet, Patrick Girardie, Elisabeth Coupez, et al. 2019. “Targeted Temperature Management for Cardiac Arrest with Nonshockable Rhythm.” The New England Journal of Medicine 381 (24): 2327–37.
- Moskowitz, Ari, Katherine M. Berg, Michael N. Cocchi, Maureen Chase, Jesse X. Yang, Jennifer Sarge, Anne V. Grossestreuer, Todd Sarge, Sharon O’ Donoghue, and Michael W. Donnino. 2019. “Cardiac Arrest in the Intensive Care Unit: An Assessment of Preventability.” Resuscitation 145 (December): 15–20.
- Ott, Matthias, Alfio Milazzo, Stefan Liebau, Christina Jaki, Tobias Schilling, Alexander Krohn, and Johannes Heymer. 2020. “Exploration of Strategies to Reduce Aerosol-Spread during Chest Compressions: A Simulation and Cadaver Model.” Resuscitation, May. https://doi.org/10.1016/j.resuscitation.2020.05.012.
- Panchal, Ashish R., Katherine M. Berg, Karen G. Hirsch, Peter J. Kudenchuk, Marina Del Rios, José G. Cabañas, Mark S. Link, et al. 2019. “2019 American Heart Association Focused Update on Advanced Cardiovascular Life Support: Use of Advanced Airways, Vasopressors, and Extracorporeal Cardiopulmonary Resuscitation During Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.” Circulation 140 (24): e881–94.
- Perman, Sarah M., Emily Stanton, Jasmeet Soar, Robert A. Berg, Michael W. Donnino, Mark E. Mikkelsen, Dana P. Edelson, et al. 2016. “Location of In-Hospital Cardiac Arrest in the United States-Variability in Event Rate and Outcomes.” Journal of the American Heart Association 5 (10). https://doi.org/10.1161/JAHA.116.003638.
- Poole, Kurtis, Keith Couper, Michael A. Smyth, Joyce Yeung, and Gavin D. Perkins. 2018. “Mechanical CPR: Who? When? How?” Critical Care / the Society of Critical Care Medicine 22 (1): 140.
- Shao, Fei, Shuang Xu, Xuedi Ma, Zhouming Xu, Jiayou Lyu, Michael Ng, Hao Cui, et al. 2020. “In-Hospital Cardiac Arrest Outcomes among Patients with COVID-19 Pneumonia in Wuhan, China.” Resuscitation 151 (June): 18–23.
- Wallmuller, Christian, Giora Meron, Istepan Kurkciyan, Andreas Schober, Peter Stratil, and Fritz Sterz. 2012. “Causes of in-Hospital Cardiac Arrest and Influence on Outcome.” Resuscitation 83 (10): 1206–11.
- Wiberg, Sebastian, Mathias J. Holmberg, Michael W. Donnino, Jesper Kjaergaard, Christian Hassager, Lise Witten, Katherine M. Berg, Ari Moskowitz, Lars W. Andersen, and American Heart Association’s Get With The Guidelines®-Resuscitation Investigators. 2020. “Age-Dependent Trends in Survival after Adult in-Hospital Cardiac Arrest.” Resuscitation 151 (June): 189–96.
View all COVID-19 Updates
Learn more about research in the Division of Pulmonary and Critical Care Medicine