FAQs, GI Disease, Washington and Italy
The FLARE Four
- FAQs about the Mass General Critical Care Guidelines
- COVID-19 presenting as GI disease
- Analysis and comparison of newly published clinical data from Washington State and Italy
- The predictors of COVID-19 mortality
FAQ About the Mass GeneralCritical Care Guidelines
After publicizing our guidelines, we have received many questions. We will address the rationale behind some of our recommendations, particularly those which contrast with SCCM guidelines.
Subscribe to the latest updates from FLARE Advances in Motion
- Why consider statins in severe COVID-19 disease?
- Mass General guidelines advise against the use of NIPPV and HFNC, but other centers are using these modalities. Why the difference?
- Mass General guidelines also call for iNO as the sole inhaled pulmonary vasodilator. Why advise against epoprostenol which has the same mechanism of action
- Why so hesitant about steroids in ARDS-associated with COVID-19?
Why Consider Statins in Severe COVID-19 Disease?
Answered by Dr. Tiara Calhoun
While it is true there is no clinical evidence to date that statins are beneficial for patients with COVID-19, there are several reasons they may be worthwhile to consider:
- Several reports so far have identified cardiovascular disease and diabetes as major risk factors for severe COVID-19 disease and COVID-19 mortality. It follows that cardiac risk reduction may also reduce the risk of severe COVID-19 disease
- Myocardial injury is frequently seen in patients with severe COVID-19, and patients with pre-existing CVD are more likely to have cardiac complications of COVID-19
- There is theoretical evidence that statins may protect the inmate immune response in COVID-19, namely through inhibition of the MYD88/NF-κB pathways
- Statins may promote improved outcomes in viral pneumonia, but the evidence is mixed and largely observational. Frost et al. (2007, large matched cohort study) found a decreased risk of death due to COPD and influenza for patients on statins compared to not; Vandermeer et al. (2012) and Kwong et al. (2009) found similarly for statin-users with influenza. On the other hand, Brett et al (2011) did not find a statistically significant association between pre-admission statin use and severity of outcome in H1N1 patients during the 2009 pandemic
- As discussed Sunday’s FLARE newsletter, statins may play an even more promising role in the hyperinflammatory phenotype of ARDS, which could represent a large portion COVID-19 ARDS patients (Calfee and Famous papers, cited below)
Statins are generally accepted as safe, are widely available, and there is no reason to suspect they will harm COVID-19 patients. Therefore, while they do not recommend statins purely for respiratory failure, the Mass GeneralCOVID Treatment Task Force feels that statin therapy is reasonable among patients with an existing primary indication for statin therapy.
Mass General Guidelines Advise Against the Use of NIPPV and HFNC, But Other Centers are Using These Modalities. Why the Difference?
Answered by Dr. Corey Hardin
Our reasoning is two-fold:
- To the extent that these patients have ARDS, NIPPV and HFNC present a serious risk of propagating lung injury. Our usual understanding of the pathophysiology of VILI which really does not distinguish between spontaneous large tidal volumes and mechanically ventilated large tidal volumes. High trans-pulmonary pressure is to be avoided in ARDS. Full stop. Thus, early intubation with lung protective ventilation is to be preferred over HFNC/NIPPV
- The recent letter in the NEJM pointing to moderately long persistence of aerosolized virus does highlight the potential risk to staff with aerosol generating procedures including HFNC and NIPPV. Granted they used a lot of HFNC in China, but with somewhat different PPE practices. Use in Italy and at other centers here has been only with limitation of flow and patients wearing masks over the cannula in the case of HFNC and helmet ventilation in the case of NIPPV. The helmet set up is not widely available here
The Mass General Guidelines Call for iNO as the Sole Inhaled Pulmonary Vasodilator. Why Advise Against Epoprostenol?
Answered by Dr. Corey Hardin
Inhaled epoprostenol is a nebulized agent, while NO is a gas mixture. As a nebulized agent epoprostenol requires a filter in the circuit that must be changed every 4 hours. This involves a risk of aerosol generation. NO is also thought to have some antiviral activity that epoprostenol does not have. It is not that the evidence for in vivo anti-viral activity is strong, it is just that it does not have to be iNO is a safer agent to deploy and is an effective pulmonary vasodilator.
Why Avoid Steroids for ARDS in COVID-19?
Answered by Dr. Laura Brenner
Multiple studies have been done over the past few decades to determine the effect of steroids to treat ARDS. The results of these trials have been both positive and negative making its use controversial for ARDS (see table below). Thus, the utility of steroids for non-COVID-19 ARDS patients is unclear.
Additionally, the data from influenza and other viral illnesses suggest an increased mortality in viral PNA and viral-mediated ARDS when steroids are used (Ni 2019, Tsai 2020). Therefore, there is concern that corticosteroids could be harmful in the viral syndrome that is COVID-19 ARDS. It is also important to note that the LaSRS trial showed worse mortality in patients who received steroids 14 days after the onset of ARDS (Steinberg 2006). As patients in the available case series on COVID-19 present to the hospital around day 10, it may be prudent to avoid steroids due to this association. Additionally, both CDC and WHO guidelines currently do not recommend steroids.
Why are Some People Using Them?
The SCCM guidelines suggest as a weak recommendation amidst admittedly low-quality evidence to use corticosteroids. Data for steroids include a non-peer-reviewed case series of COVID-19 patients with severe disease had a shorter duration of O2 use and improved radiographic studies (Wang 2020). However, there is potential for confounding in this non-randomized study so we, as well as the SCCM, are hesitant to use this data to guide clinical care. Additionally, there is data in community-acquired pneumonia that showed that corticosteroids may reduce the need for mechanical ventilation, reduce mortality, and may improve radiographic findings (Siemieniuk 2015). These trials were mostly in non-ICU patients and were not with viral pneumonia and thus we do not believe can be easily applied to this COVID-19 population.
Take Home Points
Therefore, with the evidence for potential harm and the lack of evidence for benefit in this population, we do not recommend giving steroids routinely for COVID-19 ARDS. We caveat this recommendation with the understanding that there may be secondary indications for steroid use (for example adrenal insufficiency, transplant, etc.) in which we support the use of steroids with careful weighing of the risks and benefits.
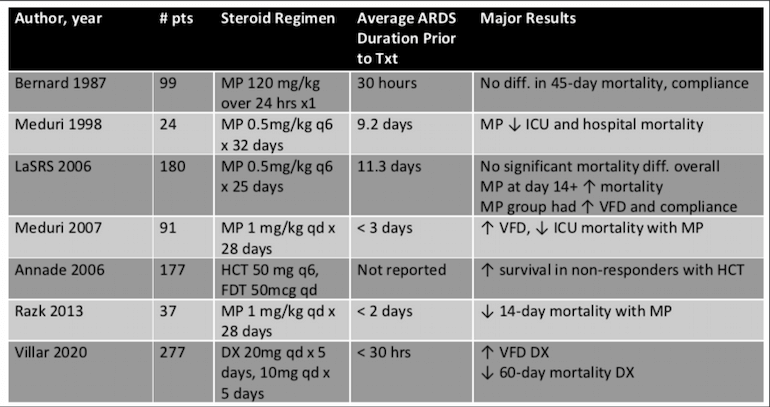
Table 1
Selection and summary of major trials including steroids for ARDS.
N.b. Several ARDS practice-changing studies were published in the midst of all of these trials. Significant limitations include: small sample sizes, some studies with cross-over between groups, and trials without standardized ventilator management.
COVID-19 Presenting with GI Illness
Courtesy of Dr. Walter O'Donnell
First, Why Might This Be Important to We Lung Doctors?
In house, one of the three patients that we admitted on MICU Blue in the past 10 days had mild transient diarrhea prior to admission but none since, and is out of the MICU.
Two Real Time Cases from Today’s Phone Calls:
- Brigham/Harvard Pulmonary alum, now a senior clinician-teacher at a major academic medical center in NYC, called me to report presenting to his ED 3 days ago with nausea, vomiting, and diarrhea, COVID19 tested negative, received 3 liters of IVF, no respiratory symptoms though CXR had a streak of atelectasis in LLL, stool+ for enterovirus, sent home, recovering. Three of his patients have been diagnosed and hospitalized with COVID19 in the past 5 days. His division’s schedules have already completely reorganized to handle the current overload, and he is scheduled for duty this week. Living alone, will he progress suddenly? Re-test before he goes back to work?
- 50 yo patient of mine with bronchiectasis, called last week with a typical flare, given doxy for MSSA. She called yesterday because her 18 yo daughter home for a week from college developed fever, nausea, vomiting, diarrhea, aches, malaise but no cough or dyspnea. I sent her daughter to NWH for COVID/ Flu testing – now pending. This morning, my patient now has chest tightness and a sense of a “new cold”, while her daughter continues with vomiting, diarrhea, and low grade fevers, COVID19 result “will return in 3 days”
Could either or both have COVID-19? If so, what next?
Let's Turn to a Preprint Article in the AJG
Below is a synopsis from preprint of “Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study.” Pan L Mu M et al, Am J Gastroenterol 2020 (not yet in Pubmed, but on AJG website)
Background
SARS-CoV2 is known to be to be capable of invading the GI tract, and in one small study, virus was detected in stool specimens of 50% of infected patients, but not much has been reported about GI symptoms as part of the COVID-19 syndrome.
Methods
Multicenter cohort study of COVID-19 PCR-positive patients (by throat swab) with chest CT scans and complete lab data admitted to three hospitals in Hubei province including Wuhan from 1/18-2/28/2020, with followup through 3/5/20.
Results
- Original cohort according to the text was n = 300 (vs 310 according to figure 1), and 96 were excluded due to lack of CT or absence of PCR confirmation or lack of complete lab data, leaving the reported cohort of 204 patients
- Severity of illness in the overall cohort – hard to be certain because of overlapping terminology especially the use of the term critical. 36% or 74 of the 204 were described as “critically ill”, with 16 or 8% transferred to ICU
- GI symptoms in 99, 48% overall in the cohort of 204
- No difference in demographics (mean age 55 yr, 55% male, 5% smoking) contact history, or underlying diseases compared to non-GI
- Anorexia was considered as a GI symptom and found in 83% of the GI subgroup
- Diarrhea 29% of GI subgroup, Vomiting in 8%, Abdominal pain in 4%
- Most of us would consider anorexia not a GI symptom per se, but a common, systemic symptom of illness especially an infection. Per authors, if anorexia were not considered to be a GI symptom, 20% of entire cohort of 204 had GI symptoms of diarrhea, vomiting or abdominal pain, but no separate analysis was performed on this subgroup. Diarrhea was most commonly non-dehydrating loose stools and usually not high volume
- Fever in 94%; Concomitant Respiratory symptoms in 93% (81% in non-GI)
- Pure GI without respiratory symptoms in 7%
- Presented later: 9.0 days vs 7.3 days of illness in non-GI
- No difference in CBC/diff, LFTs, coags, d-dimer, CK or other labs except PT 14.1 +/- 5.0 vs 12.5 +/- 2.3
- Prognosis per authors was worse in GI subgroup, but the numbers from Table 1 don’t bear this out. Mortality was 18% overall, 19.2% in GI subgroup vs 16.2% in non-GI, p = 0.57. There was also a trend for less ICU transfer need, 5.1% in GI subgroup compared to 10.5% in non-GI. Table 1 indicates 22 of 99 were “critical” but that was not defined
- The authors’ basis for increased severity in the GI subgroup seemed to be that they were less likely to be discharged by end of study period – 46% of GI subgroup were still in house, vs 24% of non-GI patients
Conclusions
In this early, small series of patients in Hubei province who were ill enough to be hospitalized and limited to those with PCR-confirmed infection and complete lab/chest CT data, 48% had GI symptoms, mainly anorexia.
In terms of prominent GI symptoms, 20% of the overall cohort had diarrhea, vomiting, or abdominal pain. The presence of GI symptoms (when anorexia was included) was correlated with a delayed presentation, possibly more frequent respiratory symptoms, and with a prolonged hospitalization. GI symptoms did not correlate with LFTs or any lab indices of inflammation or severity including creatinine, except a mildly elevated PT, nor with ICU transfer or increased risk of death.
How to Apply this Preliminary Data to These Outpatients?
The pulmonary/critical care faculty member could certainly have GI-predominant COVID-19 in addition to enterovirus, with implications for his own health if he develops respiratory disease consistent with his chest Xray, and for his division’s staffing.
The mother with bronchiectasis has a reasonable chance of exposure to COVID-19 and incipient respiratory illness, or her daughter may have norovirus or another enterovirus.
I would also recommend an excellent podcast featuring one of Miranda’s favorite PennMed professors, Paul Offit, an ID physician and co-developer of the rotavirus vaccine, who gives a fascinating, if contrarian, perspective on SARS-CoV2 as potentially being fecal-oral spread: https://zdoggmd.com/podcasting/paul-offit-covid/.
Update on Recently Published Clinical Data from Washington and Italy
Courtesy of Dr. Rebecca Israel
In the last week, JAMA published two case series describing COVID-19 cohorts in Italy and Washington State. Here we intend to understand this new data in the context of larger and more mature studies of Chinese patients.
What Accounts for Differences in Case Fatality Rates (CFR) in China, Italy, and Washington?
The case fatality rate is defined as the number of deaths divided by the number of confirmed cases. The current CFR for Italy is 7.2% compared to 1.4% in China. There are several factors that may be influencing the difference in CFR.
- Selection Bias: In the US and Italy, due to limited resources, hospitalized patients and those with severe symptoms are preferentially tested. As a result, the confirmed population (denominator) reflects the sickest subset of the population rather than the true prevalence of the disease. As recognition and testing of COVID-19 becomes widespread, the crude fatality rate is expected decrease. In fact, in China the initial CFR decreased from 17.3% in January to 0.7% in February as tests became more accessible
- Population Specific Factors: There are unique features of the populations affected in both Italy and Washington. Italy has the second oldest population in the world with 23% of people older than 65 years (compared to 15% in the US). In fact, people ≥70 years old account for 37.6% of cases in Italy but only 11.9% of cases in China. This may account for higher CFR given the association between older age and COVID-19 mortality. Similarly, in Washington, COVID-19 differentially impacted an elderly population given an early outbreak in a local nursing home, the Life Care Center, resulting in at least 37 deaths. While this highlights the risk to older patients with co-morbidities, it is difficult to extrapolate these results to the general population
- Definitions: For the data reported from Italy, case fatalities included anyone diagnosed with COVID-19 by RT-PCR who died. However, dying with COVID-19 (association) is not equivalent to dying from COVID-19 (causation). Although yet to be published in a peer-reviewed journal, Prof Walter Riccardi, the Scientific Advisor to the Italian Minister of Health, reported on March 20, 2020 that on reevaluation, “only 12% of death certificates have shown direct causality.” Furthermore, in a retrospective review of 355 deceased Italian patients with RT-PCR proven COVID-19 infection, only 3 (0.2%) had no comorbidities or identifiable alternative causes of death (Onder 2020)
What are the Predictors of COVID-19 Mortality?
Across all three cohorts, older age increases the risk for severe disease and mortality. In a population of 191 hospitalized patients in Wuhan, China, multivariable regression demonstrated a significant association between age and in-hospital mortality (OR 1.10, CI 1.03-1.17 per year increase, p=0.0043). A similar trend has also been noted in Italy.
The current data also suggest an association between comorbidities and severe disease. In a Chinese cohort of 1099 inpatients and outpatients with RT-PCR diagnosed COVID-19, 67 patients (38.7%) with severe disease had ≥1 comorbidity while only 194 (21.0%) with non-severe disease had at ≥1 comorbidity. Similarly, in a retrospective review of 355 deceased Italian patients with COVID-19, 352 (99.8%) had ≥1 comorbidity. In a 21 person cohort of critically ill COVID-19 patients in Washington, 18 (86%) had ≥1 comorbidity. Initial data from China suggest that hypertension, diabetes, and coronary artery disease are the most common comorbidities among COVID-19 patients, however there is insufficient data to draw meaningful conclusions. Finally, early results suggest that lymphocytopenia may be an important marker of disease severity, with multiple studies demonstrating an association between initial lymphocyte counts <1000 cells/µL and development of severe disease.
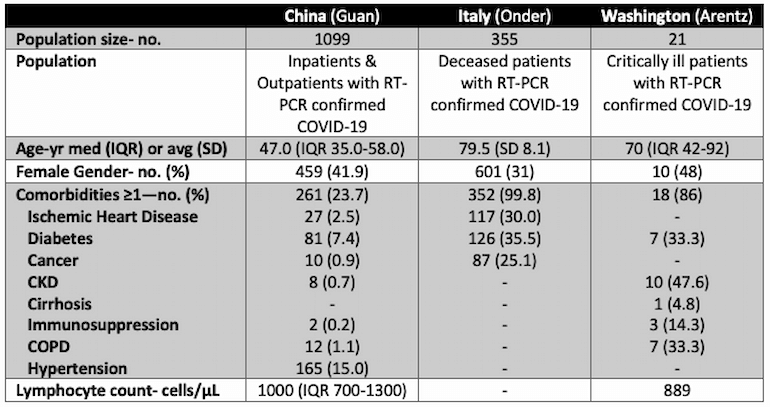
Table 2
Comparison of patient characteristics in the major Chinese, Italy and American published studies.
References
- Brett SJ, Myles P, Lim WS, Enstone JE, Bannister B, Semple MG, et al. Pre-admission statin use and in-hospital severity of 2009 pandemic influenza A(H1N1) disease. PLoS One. 2011;6(4):e18120.
- Douglas I, Evans S, Smeeth L. Effect of statin treatment on short term mortality after pneumonia episode: cohort study. BMJ. 2011 Apr 6;342:d1642
- Famous KR, Delucchi K, Ware LB, et al. Acute Respiratory Distress Syndrome Subphenotypes Respond Differently to Randomized Fluid Management Strategy. AJCCRM 2017;195:331-8.
- Frost FJ, Petersen H, Tollestrup K, and Skipper B. Influenza and COPD mortality protection as pleiotropic, dose-dependent effects of statins. Chest, vol. 131, no. 4, pp. 1006–1012.
- Kwong JC, Li P, and Redelmeier DA. Influenza morbidity and mortality in elderly patients receiving statins: a cohort study. PLoS ONE, vol. 4, no. 11, Article ID e0008087.
- Vandermeer ML1, Thomas AR, Kamimoto L, et al. Association between use of statins and mortality among patients hospitalized with laboratory-confirmed influenza virus infections: a multistate study. J Infect Dis. 2012 Jan 1;205(1):13-9.
- Yuan S. Statins May Decrease the Fatality Rate of Middle East Respiratory Syndrome Infection. mBio. 2015;6(4):e01120-15
- Zheng Y-Y, Ma Y-T, Zhang J-Y, Xie X. COVID-19 and the cardiovascular system. Nature Reviews Cardiology. 2020
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020.
- Steinberg KP, Hudson LD, Goodman RB, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. NEJM 2006;354:1671-84.
- Villar J, Ferrando C, Martinez D, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med 2020;8:267-76.
- Ni YN, Chen G, Sun J, Liang BM, Liang ZA. The effect of corticosteroids on mortality of patients with influenza pneumonia: a systematic review and meta-analysis. Crit Care 2019;23:99.
- Tsai MJ, Yang KY, Chan MC, et al. Impact of corticosteroid treatment on clinical outcomes of influenza-associated ARDS: a nationwide multicenter study. Ann Intensive Care 2020;10:26.
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
- Wang Y, Jiang W, He Q, Wang C, Wang B, Zhou P, Dong N, Tong Q, (2020) Early, low-dose and short-term application of corticosteroid treatment in patients with severe COVID-19 pneumonia: single-center experience from Wuhan, China. medRxiv: 2020.2003.2006.20032342
- Siemieniuk RA, Meade MO, Alonso-Coello P, Briel M, Evaniew N, Prasad M, Alexander PE, Fei Y, Vandvik PO, Loeb M, Guyatt GH, (2015) Corticosteroid Therapy for Patients Hospitalized With Community-Acquired Pneumonia: A Systematic Review and Meta-analysis. Ann Intern Med 163: 519-528
- Onder G, Rezza G, Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020.
- Arentz M, Yim E, Klaff L, et al. Characteristics and Outcomes of 21 Critically Ill Patients with COVID-19 in Washington State. JAMA. 2020.
- Zhou F, Yu T, Fan G, et al. Clinical Course and Risk Factors for Mortality of Adult Inpatient with COVID-19 in Wuhan, China: A Retrospective Cohort Study. Lancet. 2020.
- Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. NEJM. 2020.
- Livingstone E, Bucher M. Coronavirus Disease 2019 (COVID-19) in Italy. JAMA. 2020.
- Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID 2019). 2020.
View all COVID-19 updates
Learn about research in the Division of Pulmonary and Critical Care Medicine