COVID-19 Risk Factor Round-Up
The FLARE Four
- You may find yourself in an ICU. You may ask yourself..."Well, how did I get here?"
- A minority of patients with COVID-19 require ICU-level care. Early reports from China indicated that risk factors for severe disease included advanced age, cardiac disease and diabetes
- Since we have been letting the days go by, tonight’s FLARE will summarize and appraise the best evidence to date on risk factors for severe disease
- More recent reports are largely consistent with early reports and emphasize that risk factors for severe COVID-19 (a once in a lifetime pandemic) are qualitatively similar to risk factors for mortality in general critical illness
Many people are saying...with regards to risk factors for severe COVID-19, it’s the same as it ever was.
Subscribe to the latest updates from FLARE Advances in Motion
Risk Factor Round-Up
To date, over a dozen studies have attempted to identify risk factors associated with severe COVID-19 or related death. Methodologies vary widely and studies are of overall poor quality, with most papers presenting unadjusted analyses or raw proportions instead of comparative measures. In general, risk factors for morbidity and mortality in COVID-19 are similar to known risk factors for morbidity and mortality in the ICU: advanced age and presence of comorbidities including cardiovascular disease, hypertension, diabetes, chronic lung disease, and cancer. Severe obesity (BMI ≥40), immunocompromising conditions, chronic kidney and liver disease are also implicated (and included in the United States CDC list of risk factors), although the data about COVID-19 in these conditions is limited.
As an example, early US outcomes data from the CDC indicated mortality is indeed highest among the oldest age groups (see table below comparing case fatality rates among US, Chinese, and Italian cohorts). Among American patients, comorbidities more common in ICU patients than non-ICU hospitalized patients included diabetes (32% vs 24%), cardiovascular disease (29% vs 23%) and chronic lung disease (21% vs 15%). Although age and risk factor associations to date have been similar in US, Chinese, and Italian cohorts, Americans may be especially at risk for poor outcomes, given high rates of obesity and related metabolic disease; 10.1% of American have diabetes, 10.6% have cardiovascular disease, 5.9% have COPD, and 7.9% have active asthma (CDC COVID-19 Response Team, 2020a).

Table 1
Case Fatality Rate (CFR) by Age Group in the USA, Italy, and China.
Case fatality rate (CFR) is the proportion of fatal cases compared to the total number of reported cases since the first identification of SARS-CoV-2 infection.
The largest compiled datasets come from two meta-analyses and the Chinese CDC cohort. Yang et al. analyzed 8 studies published prior to February 25, 2020, encompassing 46,246 patients. The most prevalent comorbidities were hypertension (17%), diabetes (8%), cardiovascular diseases (5%), and respiratory disease (2%) (Yang et al., 2020a). For comparison, the overall prevalence of hypertension and diabetes in China are 23.2% and 10.9%, respectively (Liu et al., 2019; Ma et al., 2020). Risk factors for severe disease where hypertension (OR 2.36, 95% CI: 1.46-3.83), respiratory disease (OR 2.46, 95% CI: 1.76-3.44), and cardiovascular diseases (OR 3.42, 95% CI: 1.88-6.22). Of note, the authors did not define severe and non-severe disease, and different definitions may have been used among the studies analyzed.
Emami et al., analyzed 10 studies published prior to February 15, 2020 encompassing 76,993 patients. The pooled prevalence of hypertension, cardiovascular disease, smoking history, and diabetes in COVID-19 patients regardless of disease severity were estimated at 16.37%, 12.11%, 7.63% and 7.87%, respectively (Emami et al., 2020).
Finally, the Chinese CDC cohort published by Woo and McGoogan encompassed 44,672 confirmed cases in Mainland China through Feb 11, 2020. Overall case-fatality rate (CFR) was 2.3%. CFR was higher among older patients (see above table) and among patients with pre-existing medical comorbidities: 10.5% for cardiovascular disease, 7.3% for diabetes, 6.3% for chronic respiratory disease, 6.0% for hypertension, and 5.6% for cancer (Wu and McGoogan, 2020). These results are similar to the many other case series published to date (primarily from China, although one is from Italy).
Select reports are detailed in the table below; others have been omitted for brevity (Du et al., 2020; Guan et al., 2020b; Huang et al., 2020; Liu et al., 2019; Wang et al., 2020; Yang et al., 2020b; Zhang et al., 2020; Zhou et al., 2020).
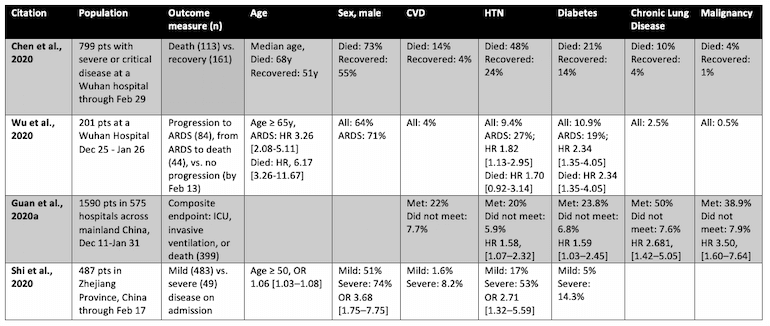
Table 2
Select case series addressing risk factors for severe COVID-19 or related death.
Other risk factors have been implicated. In a systematic review, Vardavas and Nikitara found that current smokers were 1.4 times more likely (RR = 1.4, 95% CI: 0.98–2.00) to have severe symptoms of COVID-19 and approximately 2.4 times more likely to be admitted to an ICU, need mechanical ventilation, or die compared to non-smokers (RR =2.4, 95% CI: 1.43–4.04)
Are These Risk Factors Unique to SARS-CoV-2?
To answer, let us review some prior data.
Two major studies during the SARS epidemic reported that advanced age was an independent predictor of mortality or severe disease. Interestingly, the presence of other coexisting conditions was not associated with worse clinical outcomes in either cohort (totaling 4141 patients) (Choi et al., 2003; Lee et al., 2003).
Among critically ill patients with pneumonia, a secondary analysis of clinical trial data found that male sex, higher APACHE II score on admission, chronic heart failure, and dialysis were independently associated with risk of hospital mortality (Li et al., 2016).
Finally, when looking specifically at ARDS, Luo et al. found that non-survivors of direct ARDS (meaning ARDS caused by an identifiable pulmonary injury, such as pneumonia or aspiration), were older (55 vs. 58, p= 0.04), had elevated BMI (25 vs. 26, p =0.03), and chronic liver disease (4% vs. 16%, p = 0.001) (Luo et al., 2017).
Studies thus consistently demonstrate that in respiratory failure from a variety of causes, older age, and underlying chronic organ dysfunction are associated with worse mortality.
Major Limitations
Reports to date have not adequately adjusted for confounders such as age, sex, and smoking status, limiting their interpretation. Further, pre-existing conditions are likely under-reported. For example, Chen et al. reported a 7% rate of current or prior smoking in their cohort, whereas the prevalence of smoking among Chinese males is estimated at 48% (World Bank, 2016). Finally, follow up periods have been short---several reports have been published with less than half of the cohort having reached one of the primary outcomes (i.e. death or discharge). Due to these significant limitations, the relative contributions of underlying health conditions remain unclear and additional studies are needed.
In the end, the current data suggest that the risk factors associated with critical illness due to COVID-19 do not appear qualitatively different from risk factors for poor outcome in critical illness due to other causes.
References
- CDC COVID-19 Response Team (2020a). Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019—United States, February 12–March 28, 2020.
- CDC COVID-19 Response Team (2020b). Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 343–346.
- Chen, T., Wu, D., Chen, H., Yan, W., Yang, D., Chen, G., Ma, K., Xu, D., Yu, H., Wang, H., et al. (2020). Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 368, m1091.
- Chinese CDC (2020). The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China, 2020. CCDCW 2, 113–122.
- Choi, K.W., Chau, T.N., Tsang, O., Tso, E., Chiu, M.C., Tong, W.L., Lee, P.O., Ng, T.K., Ng, W.F., Lee, K.C., et al. (2003). Outcomes and prognostic factors in 267 patients with severe acute respiratory syndrome in Hong Kong. Ann. Intern. Med. 139, 715–723.
- Du, Y., Tu, L., Zhu, P., Mu, M., Wang, R., Yang, P., Wang, X., Hu, C., Ping, R., Hu, P., et al. (2020). Clinical Features of 85 Fatal Cases of COVID-19 from Wuhan: A Retrospective Observational Study. Am. J. Respir. Crit. Care Med.
- Emami, A., Javanmardi, F., Pirbonyeh, N., and Akbari, A. (2020). Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis. Arch Acad Emerg Med 8, e35.
- Guan, W.-J., Liang, W.-H., Zhao, Y., Liang, H.-R., Chen, Z.-S., Li, Y.-M., Liu, X.-Q., Chen, R.-C., Tang, C.-L., Wang, T., et al. (2020a). Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. Eur. Respir. J.
- Guan, W.-J., Ni, Z.-Y., Hu, Y., Liang, W.-H., Ou, C.-Q., He, J.-X., Liu, L., Shan, H., Lei, C.-L., Hui, D.S.C., et al. (2020b). Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med.
- Huang, R., Zhu, L., Xue, L., Liu, L., Yan, X., Wang, J., Zhang, B., Xu, T., Ji, F., Zhao, Y., et al. (2020). Clinical Findings of Patients with Coronavirus Disease 2019 in Jiangsu Province, China: A Retrospective, Multi-Center Study.
- Lee, N., Hui, D., Wu, A., Chan, P., Cameron, P., Joynt, G.M., Ahuja, A., Yung, M.Y., Leung, C.B., To, K.F., et al. (2003). A major outbreak of severe acute respiratory syndrome in Hong Kong. N. Engl. J. Med. 348, 1986–1994.
- Li, G., Cook, D.J., Thabane, L., Friedrich, J.O., Crozier, T.M., Muscedere, J., Granton, J., Mehta, S., Reynolds, S.C., Lopes, R.D., et al. (2016). Risk factors for mortality in patients admitted to intensive care units with pneumonia. Respir. Res. 17, 80.
- Liu, M., Liu, S.-W., Wang, L.-J., Bai, Y.-M., Zeng, X.-Y., Guo, H.-B., Liu, Y.-N., Jiang, Y.-Y., Dong, W.-L., He, G.-X., et al. (2019). Burden of diabetes, hyperglycaemia in China from to 2016: Findings from the 1990 to 2016, global burden of disease study. Diabetes Metab. 45, 286–293.
- Luo, L., Shaver, C.M., Zhao, Z., Koyama, T., Calfee, C.S., Bastarache, J.A., and Ware, L.B. (2017). Clinical Predictors of Hospital Mortality Differ Between Direct and Indirect ARDS. Chest 151, 755–763.
- Ma, L.-Y., Chen, W.-W., Gao, R.-L., Liu, L.-S., Zhu, M.-L., Wang, Y.-J., Wu, Z.-S., Li, H.-J., Gu, D.-F., Yang, Y.-J., et al. (2020). China cardiovascular diseases report 2018: an updated summary. J. Geriatr. Cardiol. 17, 1–8.
- Onder, G., Rezza, G., and Brusaferro, S. (2020). Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA.
- Shi, Y., Yu, X., Zhao, H., Wang, H., Zhao, R., and Sheng, J. (2020). Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit. Care 24, 108.
- Wang, L., He, W., Yu, X., Hu, D., Bao, M., Liu, H., Zhou, J., and Jiang, H. (2020). Coronavirus Disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J. Infect.
- World Bank (2016). Smoking prevalence, males (% of adults) | Data.
- Wu, Z., and McGoogan, J.M. (2020). Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA.
- Wu, C., Chen, X., Cai, Y., Xia, J. ’an, Zhou, X., Xu, S., Huang, H., Zhang, L., Zhou, X., Du, C., et al. (2020). Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med.
- Yang, J., Zheng, Y., Gou, X., Pu, K., Chen, Z., Guo, Q., Ji, R., Wang, H., Wang, Y., and Zhou, Y. (2020a). Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int. J. Infect. Dis.
- Yang, X., Yu, Y., Xu, J., Shu, H., Xia, J. ’an, Liu, H., Wu, Y., Zhang, L., Yu, Z., Fang, M., et al. (2020b). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med.
- Zhang, J.-J., Dong, X., Cao, Y.-Y., Yuan, Y.-D., Yang, Y.-B., Yan, Y.-Q., Akdis, C.A., and Gao, Y.-D. (2020). Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy.
- Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., Xiang, J., Wang, Y., Song, B., Gu, X., et al. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395, 1054–1062.
View all COVID-19 updates
Learn about research in the Division of Pulmonary and Critical Care Medicine