SARS-CoV-2 Affects Children Differently Than Adults
The FLARE Four
- The kids are alright: When infected with SARS-CoV-2, children may have lower rates of symptomatic infection and decreased illness severity compared to adults
- Infants (<1 year old) seem to have a slightly higher risk for severe or critical illness compared to other pediatric age groups
- Overall mortality in children is extremely low
- The mechanisms leading to lower rates of severe illness in children are unknown
Special thanks to Dr. Sara C. Handley from the Children’s Hospital of Philadelphia for her contributions.
Subscribe to the latest updates from FLARE Advances in Motion
Many people are saying...SARS-CoV-2 affects children differently than adults.
Though FLARE primarily focuses on the care of adult patients with COVID-19, many adult providers caring for COVID-19 patients return home to their families, which may include children. Today’s FLARE discusses the current footprint of SARS-CoV-2 in pediatric populations.
Do Children Get COVID-19? How Sick Do They Get?
It appears that children (<18 years old) represent a small proportion of COVID-19 infections and that, overall, pediatric infections are less severe than adult infections.
Initial reports from China indicated that only 2.2% of the 44,672 confirmed COVID-19 cases in China were in patients aged 19 and under (Wu and McGoogan, 2020). A small Chinese case series of 9 hospitalized COVID-19 positive infants (<1 year) indicated generally mild symptoms: fever, cough, and runny nose in 6 infants and no symptoms in one patient. The study was missing data regarding symptoms in two (Wei et al., 2020). Of note, none required intensive care, mechanical ventilation, or experienced any severe complications.
While reassuring, these reports lack a robust sample size and contain no detailed clinical data.
The largest published pediatric COVID-19 cohort to date is a case series of 2,143 pediatric patients with COVID-19 (731 PCR confirmed) reported to the China CDC through February 8th, 2020 (Dong et al., 2020). This cohort reveals several key findings, including:
- No statistically significant difference in prevalence between sexes, in contrast to the gender disparity reported in adult cohorts thus far (Chen et al., 2020; Grasselli et al., 2020; Shi et al., 2020).
- The age range of patients included those from 1 day to 18 years old, demonstrating vulnerability to infection across all ages.
- 94% of children had asymptomatic, mild, or moderate disease.*
- Infants (< 1 year old) had the highest proportion of severe and critical cases of any age group. However, this group included both “confirmed” and “suspected” cases which makes interpretation difficult. No infants died.
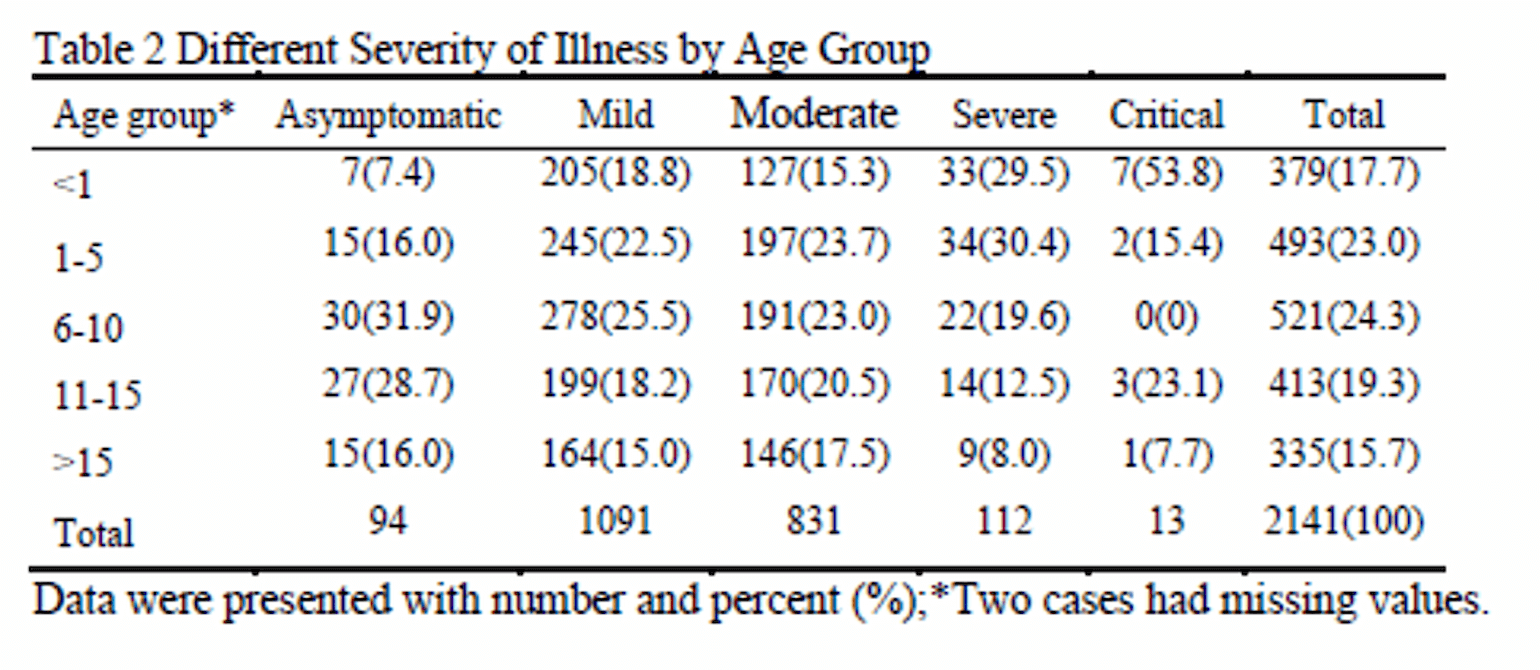
Table 1
*Asymptomatic = no symptoms. Mild = mild URI symptoms, +/- fever, +/- GI symptoms. Moderate = pneumonia, fever and cough, no hypoxemia; Severe = pneumonia, fever, cough, SpO2 < 92%. Critical = ARDS / respiratory failure, other end organ failure.
A second, smaller case series of 171 confirmed pediatric cases from Wuhan Children’s Hospital through March 8, 2020 yielded similar epidemiologic and outcome data (Lu et al., 2020).
Available data from the Italian experience suggest more of the same: 1.2% (270 cases) of their 22,512 cases as of March 15, 2020 were in children (≤ 18 years old) and no deaths were reported in this age group (Livingston and Bucher, 2020). In a recent case series of 1591 patients admitted to the ICU with COVID-19 in the Lombardy Region in Italy, only 4 patients (0.2%) were < 20 years old (Grasselli et al., 2020).
Hot off the presses yesterday (April 6, 2020), the US Morbidity and Mortality Weekly published preliminary data from the US experience (CDC MMWR, 2020). Of the 151,294 laboratory-confirmed COVID-19 cases between February 12 to April 2, 1.7% were among children <18 years. 15% of pediatric COVID-19 patients were infants (< 1 year) and 57% were males. Limited information is available on symptoms, underlying conditions, and hospitalization status. However, available information suggests that hospitalization is most common among patients aged < 1 year and in those with underlying conditions, most commonly asthma.
France, Germany, and Spain, which have more than 75,000 confirmed cases each, have not yet published data on the specific characteristics and outcomes of pediatric patients.
Do Children Die from COVID-19?
So far, thankfully, the answer to this question seems to be “very rarely”.
From the Chinese CDC data, one child in the 2,143 patient case series died. He was 14 years old, and no additional clinical data regarding the case is reported. In the subsequent case series of 171 confirmed positive children in Wuhan, one 10 month-old child with intussusception died after a four week hospitalization.
At this time, the Italians have reported no deaths in individuals under the age of 30 years (Livingston and Bucher, 2020).
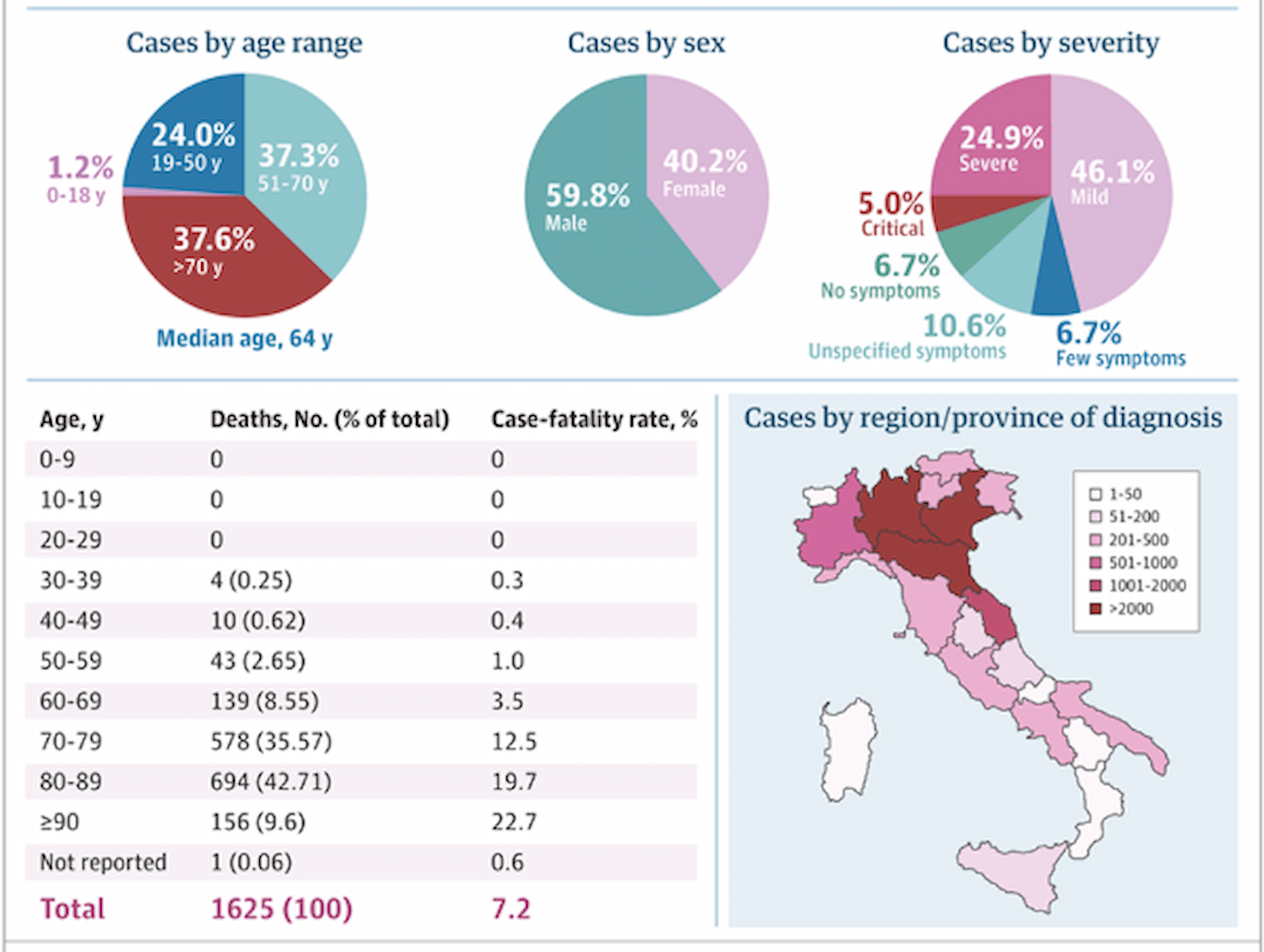
Figure 1
(Livingston and Bucher, 2020).
From the United States, three pediatric deaths were reported in the April 6, 2020 MMWR cohort. However, it is unclear at this time whether COVID-19 was the cause of death.
Why Do Children Have Milder Illness than Adults?
Whether the rate of SARS-CoV-2 infection in children is truly lower than that of adults, or the lower infection rates reflect a lack of testing in this age group (due to non-existent or mild symptoms), is unclear. Of note, similar trends were observed with SARS in 2003 and MERS in 2012: very few pediatric cases and no pediatric deaths were reported with either of those coronavirus outbreaks, despite an overall higher case fatality rate (Cao et al., 2020).
Furthermore, the etiology of the relationship between age and severity of illness remains to be determined. It may be related to differences in the immune and inflammatory responses to the virus that vary with age, as well as host factors. In adults with COVID-19, progressive decreases in peripheral lymphocyte count are an indicator of disease severity and viral activity. Early individual pediatric case reports described patients with normal lymphocyte counts and no progressive reduction in lymphocyte count during the course of illness, suggesting decreased immune dysregulation as a result of SARS-CoV-2 infection as compared to adults (Yonker et al., 2020). It is also possible that a blunted neutrophil response, diminished pro-inflammatory cytokine release, and decreased pulmonary inflammatory mediators result in lower rates of ARDS in children overall (Schouten et al., 2019). This may hold true for respiratory infections with SARS-CoV-2.
Why is it that despite becoming infected with SARS-CoV-2, children experience milder illness? And why is it that even if children become critically ill, very few die, whereas initial reports of the case fatality rate of critically ill patients, mainly adults, in Wuhan, Lombardy and Seattle ranged between 26-50% (Bhatraju et al., 2020; Grasselli et al., 2020; Wu and McGoogan, 2020)? At this point, the answers to these questions are only speculative.
References
- Bhatraju, P.K., Ghassemieh, B.J., Nichols, M., Kim, R., Jerome, K.R., Nalla, A.K., Greninger, A.L., Pipavath, S., Wurfel, M.M., Evans, L., et al. (2020). Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N. Engl. J. Med.
- Cao, Q., Chen, Y.-C., Chen, C.-L., and Chiu, C.-H. (2020). SARS-CoV-2 infection in children: Transmission dynamics and clinical characteristics. J. Formos. Med. Assoc. 119, 670–673.
- CDC MMWR (2020). Coronavirus Disease 2019 in Children — United States, February 12–April 2, 2020. MMWR Morb. Mortal. Wkly. Rep. 69.
- Chen, T., Wu, D., Chen, H., Yan, W., Yang, D., Chen, G., Ma, K., Xu, D., Yu, H., Wang, H., et al. (2020). Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 368, m1091.
- Dong, Y., Mo, X., Hu, Y., Qi, X., Jiang, F., Jiang, Z., and Tong, S. (2020). Epidemiological Characteristics of 2143 Pediatric Patients With 2019 Coronavirus Disease in China. Pediatrics.
- Grasselli, G., Pesenti, A., and Cecconi, M. (2020). Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA.
- Livingston, E., and Bucher, K. (2020). Coronavirus Disease 2019 (COVID-19) in Italy. JAMA.
- Lu, X., Zhang, L., Du, H., Zhang, J., Li, Y.Y., Qu, J., Zhang, W., Wang, Y., Bao, S., Li, Y., et al. (2020). SARS-CoV-2 Infection in Children. N. Engl. J. Med.
- Schouten, L.R., van Kaam, A.H., Kohse, F., Veltkamp, F., Bos, L.D., de Beer, F.M., van Hooijdonk, R.T., Horn, J., Straat, M., Witteveen, E., et al. (2019). Age-dependent differences in pulmonary host responses in ARDS: a prospective observational cohort study. Ann. Intensive Care 9, 55.
- Shi, Y., Yu, X., Zhao, H., Wang, H., Zhao, R., and Sheng, J. (2020). Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit. Care 24, 108.
- Wei, M., Yuan, J., Liu, Y., Fu, T., Yu, X., and Zhang, Z.-J. (2020). Novel Coronavirus Infection in Hospitalized Infants Under 1 Year of Age in China. JAMA.
- Wu, Z., and McGoogan, J.M. (2020). Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA.
- Yonker, L.M., Shen, K., and Kinane, T.B. (2020). Lessons unfolding from pediatric cases of COVID-19 disease caused by SARS-CoV-2 infection. Pediatr. Pulmonol.
View all COVID-19 updates
Learn about research in the Division of Pulmonary and Critical Care Medicine