Post-extubation Stridor in COVID-19
The FLARE Four
- There are anecdotal reports of a high incidence of post-extubation stridor and extubation failure in COVID-19
- COVID-19 patients possess many of the traditional risk factors for post-extubation complications, the most important of which is prolonged mechanical ventilation
- A number of tests (cuff leak, ultrasound, video laryngoscopy) have been investigated as means of predicting which patients will develop post-extubation stridor. None have both high sensitivity and high specificity
- Short courses of steroids prior to a planned extubation have been shown to reduce the incidence of post-extubation stridor and reintubation
Many people are saying...COVID-19 patients experience post-extubation stridor.
Subscribe to the latest updates from FLARE Advances in Motion
How Common is Post-extubation Laryngeal Edema? What are the Risk Factors?
Many intensivists are saying that their COVID-19 patients have a high rate of post-extubation stridor. Post-extubation stridor may result from laryngeal edema which is a well-described complication in the peri-extubation period in ICU patients. Decreased airway lumen circumference due to edema results in increased airflow velocity and a damaged laryngeal surface leads to turbulent flow, both contributing to stridulous breath sounds. In some cases, laryngeal edema can lead to acute airway compromise and respiratory distress.
The largest review of post-extubation laryngeal edema and stridor in pre-COVID-19 critically ill patients was by Wittekamp et al., updated by Pluijms et al. in 2015 (Pluijms et al., 2015; Wittekamp et al., 2009). They found that the incidence of laryngeal edema and stridor after extubation, as well as the need for re-intubation due to these complications varied dramatically: 5-55% for post-extubation laryngeal edema (6 studies) and 1.5-26.3% for stridor (18 studies). Among those patients, anywhere from 10 to 100% required reintubation, depending on the study (with 100% re-intubation rate reported only in one small study of 8 patients). Authors suggest that this variability may be explained by the lack of a standardized method to assess for laryngeal edema and stridor, and thus inconsistent definitions used across studies.
In the same review, reported risk factors for laryngeal injury, edema, and stridor included longer duration of intubation, high cuff pressure or large tube size relative to laryngeal size, female gender, higher BMI, history of difficult intubation, and history of self-extubation.
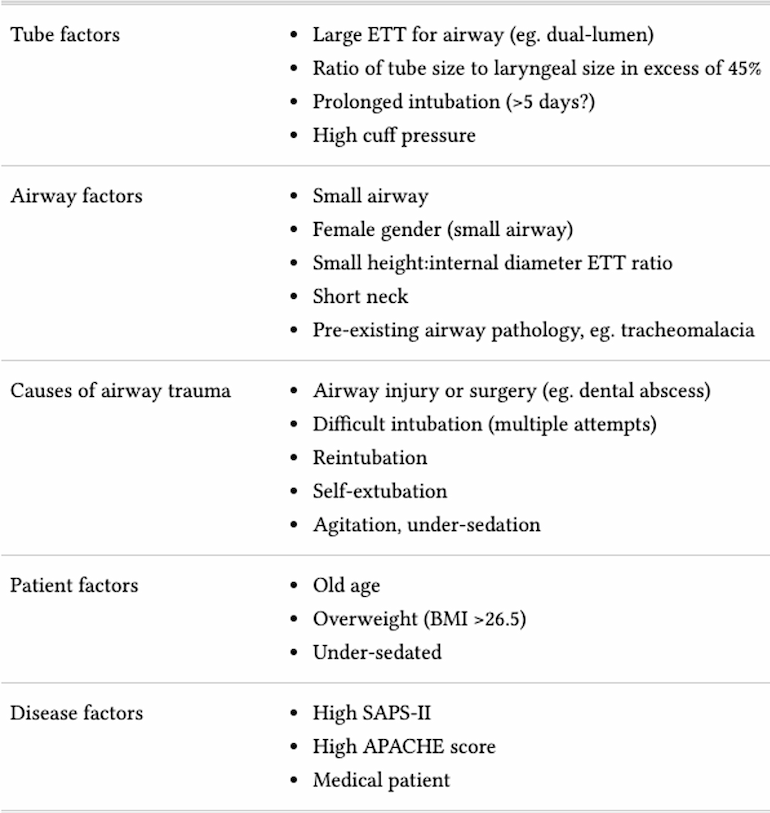
Table 1
Reported risk factors for post-extubation laryngeal edema and stridor. From Alex Yartsev, https://derangedphysiology.com/.
Is There Something Different about COVID-19 That May Put These Patients at Higher Risk for Laryngeal Edema?
Some have hypothesized that the prolonged duration of intubation for COVID-19 patients may increase the risk of laryngeal edema after extubation.
In clinical case series, it has been suggested that COVID-19 patients are intubated for prolonged periods of time (Bhatraju et al., 2020; Grasselli et al., 2020; Yang et al., 2020). Of the major published studies reporting outcomes for ICU patients, only the small study by Bhatraju et al. reports median duration of mechanical ventilation of 11 days (IQR 7-12) for 6 patients who were extubated (Bhatraju et al., 2020). In the largest series of ICU patients with COVID-19 published thus far, Grasselli et al. report the median duration of ICU stay (a proxy for duration of intubation) of 9 days (95% CI 6-13, n = 1300). However, at the time of their report, greater than 50% of patients remained in the ICU (Grasselli et al., 2020), presumably intubated.
It has been well-established that patients with severe COVID-19 are generally older (Grasselli et al., 2020; Guan et al., 2020; Wang et al., 2020; Yang et al., 2020) and are all medical patients by virtue of their predominant illness. Obesity has been common in some ICU cohorts (Barrasa et al., 2020; Bhatraju et al., 2020).
Does Prone Positioning Predispose Patients to Laryngeal Edema?
In addition to mechanical ventilation for severe COVID-19, many patients undergo prone ventilation. As such, one may hypothesize that prone positioning could be a risk factor for laryngeal edema. In major trials of proning for ARDS (Abroug et al., 2008; Guérin et al., 2013), however, researchers did not report rates of laryngeal edema or post-extubation stridor.
We can look to the spine surgery literature, as prone position is used during certain surgical procedures. However, these data do not translate directly to the prone ICU population given the differences in medical illness severity and duration of intubation.
In a 2015 systematic review of 53 papers examining the complications of prone positioning during surgery, oropharyngeal swelling was only discussed in two papers (Kwee et al., 2015). The authors propose that distortion of the salivary duct blood vessels and lymphatics with the neck in full flexion may lead to obstruction and thereby swelling of local structures. Further, the endotracheal tube itself may cause increased compressive trauma on a fully flexed neck compared to a neck in the neutral position while supine (Hans et al., 2006; Sinha et al., 2001).
In a prospective study (which was presented at a national meeting but never published), Szabo et al. observed increased laryngeal edema (graded by anesthesiologists blinded to patient position reviewing videolaryngoscopy clips), based on cuff leak and videolaryngoscopy evaluation, in patients who were operated on in the prone position compared to the supine position for operations lasting at least 3 hours, but they did not observe any evidence of postoperative airway obstruction measured via flow-volume loop (Szabo et al., 1997).
How Do I Assess Airway Patency Prior to Extubation?
Because the available epidemiology does not provide a reliable method to identify patients who may have edema or stridor after extubation, several tests have been developed to make this determination. In order of evidence base and frequency of use, these include cuff leak, laryngeal ultrasonography, and video laryngoscopy.
Cuff Leak
A cuff leak is the presence of air movement around the endotracheal tube.
Qualitative cuff leak: Cuff of the endotracheal tube is deflated and practitioner listens for audible leak.
Quantitative cuff leak:
- Patient is placed on a volume control mode of ventilation, so a known tidal volume is delivered.
- Volume controlled breath delivered to the patient while the cuff is inflated.
- The cuff of the endotracheal tube is deflated.
- Expiratory volume is measured by the ventilator over 4-6 breaths; this number is averaged.
- Quantitative cuff leak = expiratory tidal volume with cuff inflated - average expiratory volume with cuff deflated.
The leak volume above which a cuff leak is defined as present is not standardized, but many practitioners use ≥ 110 mL based on a study by Miller and Cole, where the predictive value for the absence of post-extubation stridor in the presence of a cuff leak greater than 110 mL was 0.98 (Miller and Cole, 1996).
Ochoa et al. conducted a meta-analysis of 9 studies assessing the diagnostic accuracy of cuff leak test for upper airway obstruction in ICU patients ready for extubation (Ochoa et al., 2009). The overall incidence of upper airway obstruction was 6.9%. They found a pooled sensitivity of 0.56 (95% CI 0.48-0.63) and specificity of 0.92 (95% CI 0.90-0.93) for the test. The area under the summary ROC curve was 0.92 (95% CI 0.89-0.94).
In all, it appears a low cuff leak volume portends a high risk of airway obstruction, but it is not a good rule-out test.
Laryngeal Ultrasonography
Several studies have evaluated the use of air column width measured by laryngeal ultrasonography to predict post-extubation laryngeal edema. Air column width is measured before and after cuff deflation to calculate a width difference, and it has been hypothesized that smaller width differences portend a higher risk of edema or stridor. Results from most (Ding et al., 2006; Sutherasan et al., 2013; Zytoun et al., 2019), but not all (Mikaeili et al., 2014), studies support this assertion.
This method should be used with caution in light of the limited evidence and may be appropriate only in the hands of an experienced operator.
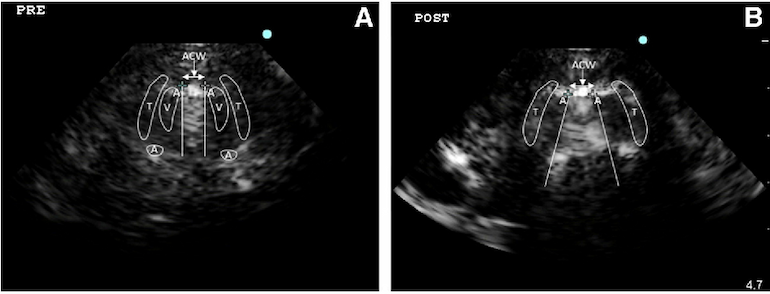
Figure 1
The imaging from laryngeal ultrasound demonstrates the air column width (ACW) deflation, the fan-shaped widening ACW obliterates surrounding structure thyroid cartilage; V, vocal cord; A, arytenoids cartilage) pre- and post- cuff deflation (Sutherasan et al., 2013).
Video Laryngoscopy
This method was proposed in a small case series by Newmark et al., but has not been systematically evaluated (Newmark et al., 2013).
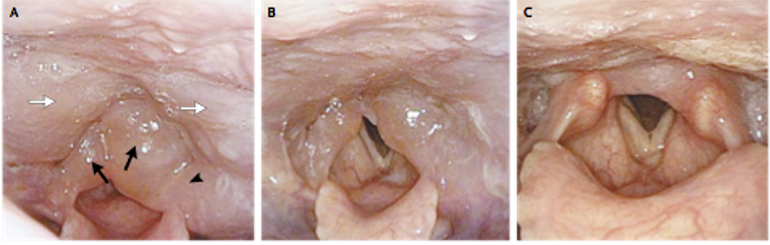
Figure 2
Images from serial fiberoptic laryngoscopy performed on a patient. Panel A: marked mucosal edema of the arytenoids (black arrows), aryepiglottic fold (arrowhead), and posterior wall of the pharynx (white arrows). Panel B: improvement in laryngeal edema one hour after glucocorticoid treatment. Panel C: near complete resolution one week later (Watanabe and Nakaya, 2011).
How Can We Treat (and Prevent) Post-extubation Laryngeal Edema?
General Prevention
Appropriate ETT sizing, maintenance of cuff pressure <25 cm H2O, and attempts to minimize the duration of intubation may all be expected to decrease the incidence of post-extubation complications.
Glucocorticoids
Aside from the above general measures, pre-extubation glucocorticoids are the best studied intervention for the prevention and treatment of stridor, laryngeal edema and/or reintubation.
The earliest studies, in which corticosteroids were administered only once 1 hour prior to extubation, failed to show benefit (Darmon et al., 1992; Ho et al., 1996). Cheng et al. demonstrated decreased post-extubation stridor when patients who failed a quantitative cuff leak test (< 24% of tidal volume) were treated with 1 or 4 doses of methylprednisolone in the 24 hours prior to extubation (Cheng et al., 2006).
Later double-blind RCTs in which steroids were given at set intervals over a longer duration (12-48 hours prior to extubation) did show significantly less laryngeal edema, reduced reintubation (François et al., 2007), and less stridor (Lee et al., 2007) in the treated groups. Cheng and colleagues found a benefit for a single dose of methylprednisolone 40 mg IV administered 4 hours prior to extubation (Cheng et al., 2011), suggesting longer courses and repeat dosing may not be necessary.
In the most recent trial, Abbasi et al. found a similar benefit to inhaled budesonide administered in 4 doses over 48 hours after extubation, although this therapy may not be appealing in the COVID-19 population due to aerosolization risk with nebulized medications.
Of note, both Francois et al. and Abbasi et al. did not require patients to meet a pre-specified high-risk criterion such as low cuff leak for inclusion, but still showed a benefit. This suggests steroids could be used in all-comers and still be beneficial.
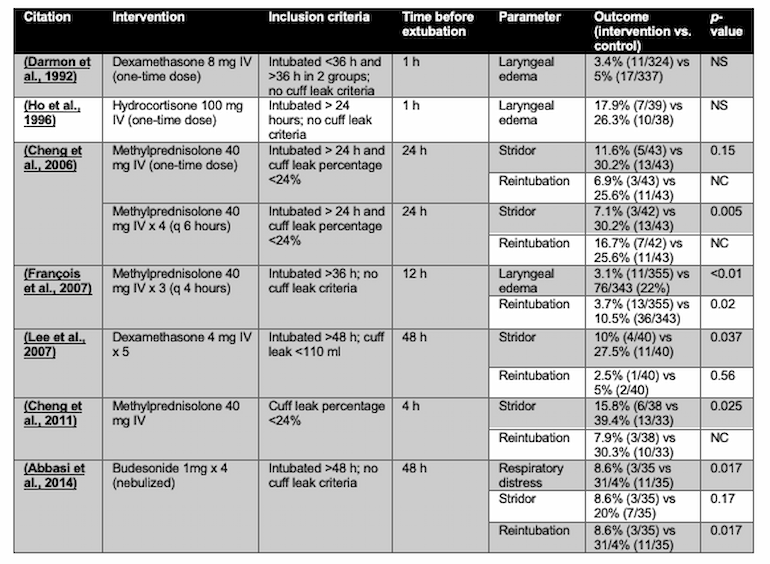
Table 2
The effect of glucocorticoids on post-extubation laryngeal edema, stridor, respiratory distress and reintubation. Adapted from (Pluijms et al., 2015). NS = p-value >0.05 or not reported. NC = not calculated.
In all, the body of evidence suggests that anticipatory glucocorticoids are effective in reducing the incidence of post-intubation laryngeal edema/stridor in adult patients undergoing prolonged intubation. However, the potential benefit of the use of steroids for laryngeal edema specifically in a viral pneumonia such as COVID-19 (in which long courses of steroids have been associated with harm (Ni et al., 2019)) has not been specifically studied.
Other Therapies
Racemic epinephrine and helium-oxygen mixture have also been used, but lack randomized-controlled trial data, especially in adults. Non-invasive positive pressure ventilation and high flow nasal cannula should be used with caution as they may delay re-intubation in a patient who truly needs it (Pluijms et al., 2015) and they are associated with aerosolization risk in the COVID-19 population.
Summary
Patients with COVID-19 have risk factors for laryngeal edema the most important of which is prolonged intubation. Available data suggest that glucocorticoids given approximately 4-12 hours prior to extubation can prevent reintubation as well as laryngeal edema and/or stridor. This can be done with or without measurement of cuff leak prior to extubation. We await further data reporting the incidence of post-extubation stridor, laryngeal edema, and need for reintubation specifically in the COVID-19 population.
References
- Abbasi, S., Moradi, S., Talakoub, R., Kashefi, P., and Koushki, A.M. (2014). Effect of nebulized budesonide in preventing postextubation complications in critically patients: A prospective, randomized, double-blind, placebo-controlled study. Adv. Biomed. Res. 3, 182.
- Abroug, F., Ouanes-Besbes, L., Elatrous, S., and Brochard, L. (2008). The effect of prone positioning in acute respiratory distress syndrome or acute lung injury: a meta-analysis. Areas of uncertainty and recommendations for research. Intensive Care Med. 34, 1002–1011.
- Barrasa, H., Rello, J., Tejada, S., Martín, A., Balziskueta, G., Vinuesa, C., Fernández-Miret, B., Villagra, A., Vallejo, A., Sebastián, A.S., et al. (2020). SARS-Cov-2 in Spanish Intensive Care: Early Experience with 15-day Survival In Vitoria. Anaesth Crit Care Pain Med.
- Bhatraju, P.K., Ghassemieh, B.J., Nichols, M., Kim, R., Jerome, K.R., Nalla, A.K., Greninger, A.L., Pipavath, S., Wurfel, M.M., Evans, L., et al. (2020). Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N. Engl. J. Med.
- Cheng, K.-C., Hou, C.-C., Huang, H.-C., Lin, S.-C., and Zhang, H. (2006). Intravenous injection of methylprednisolone reduces the incidence of postextubation stridor in intensive care unit patients. Crit. Care Med. 34, 1345–1350.
- Cheng, K.C., Chen, C.M., Tan, C.K., Chen, H.M., Lu, C.L., and Zhang, H. (2011). Methylprednisolone reduces the rates of postextubation stridor and reintubation associated with attenuated cytokine responses in critically ill patients. Minerva Anestesiol. 77, 503–509.
- Darmon, J.Y., Rauss, A., Dreyfuss, D., Bleichner, G., Elkharrat, D., Schlemmer, B., Tenaillon, A., Brun-Buisson, C., and Huet, Y. (1992). Evaluation of risk factors for laryngeal edema after tracheal extubation in adults and its prevention by dexamethasone. A placebo-controlled, double-blind, multicenter study. Anesthesiology 77, 245–251.
- Ding, L.-W., Wang, H.-C., Wu, H.-D., Chang, C.-J., and Yang, P.-C. (2006). Laryngeal ultrasound: a useful method in predicting post-extubation stridor. A pilot study. Eur. Respir. J. 27, 384–389.
- François, B., Bellissant, E., Gissot, V., Desachy, A., Normand, S., Boulain, T., Brenet, O., Preux, P.-M., Vignon, P., and Association des Réanimateurs du Centre-Ouest (ARCO) (2007). 12-h pretreatment with methylprednisolone versus placebo for prevention of postextubation laryngeal oedema: a randomised double-blind trial. Lancet 369, 1083–1089.
- Gattinoni, L., Tognoni, G., Pesenti, A., Taccone, P., Mascheroni, D., Labarta, V., Malacrida, R., Di Giulio, P., Fumagalli, R., Pelosi, P., et al. (2001). Effect of prone positioning on the survival of patients with acute respiratory failure. N. Engl. J. Med. 345, 568–573.
- Grasselli, G., Zangrillo, A., Zanella, A., Antonelli, M., Cabrini, L., Castelli, A., Cereda, D., Coluccello, A., Foti, G., Fumagalli, R., et al. (2020). Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA.
- Guan, W.-J., Ni, Z.-Y., Hu, Y., Liang, W.-H., Ou, C.-Q., He, J.-X., Liu, L., Shan, H., Lei, C.-L., Hui, D.S.C., et al. (2020). Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med.
- Guérin, C., Reignier, J., Richard, J.-C., Beuret, P., Gacouin, A., Boulain, T., Mercier, E., Badet, M., Mercat, A., Baudin, O., et al. (2013). Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 368, 2159–2168.
- Hans, P., Demoitié, J., Collignon, L., Bex, V., and Bonhomme, V. (2006). Acute bilateral submandibular swelling following surgery in prone position. Eur. J. Anaesthesiol. 23, 83–84.
- Ho, L.I., Harn, H.J., Lien, T.C., Hu, P.Y., and Wang, J.H. (1996). Postextubation laryngeal edema in adults. Risk factor evaluation and prevention by hydrocortisone. Intensive Care Med. 22, 933–936.
- Kwee, M.M., Ho, Y.-H., and Rozen, W.M. (2015). The prone position during surgery and its complications: a systematic review and evidence-based guidelines. Int. Surg. 100, 292–303.
- Lee, C.-H., Peng, M.-J., and Wu, C.-L. (2007). Dexamethasone to prevent postextubation airway obstruction in adults: a prospective, randomized, double-blind, placebo-controlled study. Crit. Care 11, R72.
- Mikaeili, H., Yazdchi, M., Tarzamni, M.K., Ansarin, K., and Ghasemzadeh, M. (2014). Laryngeal ultrasonography versus cuff leak test in predicting postextubation stridor. J Cardiovasc Thorac Res 6, 25–28.
- Miller, R.L., and Cole, R.P. (1996). Association between reduced cuff leak volume and postextubation stridor. Chest 110, 1035–1040.
- Newmark, J.L., Ahn, Y.K., Adams, M.C., Bittner, E.A., and Wilcox, S.R. (2013). Use of video laryngoscopy and camera phones to communicate progression of laryngeal edema in assessing for extubation: a case series. J. Intensive Care Med. 28, 67–71.
- Ni, Y.N., Chen, G., Sun, J., Liang, B.M., and Liang, Z.A. (2019). The effect of corticosteroids on mortality of patients with influenza pneumonia: a systematic review and meta-analysis. Crit. Care 23, 99.
- Ochoa, M.E., Marín, M. del C., Frutos-Vivar, F., Gordo, F., Latour-Pérez, J., Calvo, E., and Esteban, A. (2009). Cuff-leak test for the diagnosis of upper airway obstruction in adults: a systematic review and meta-analysis. Intensive Care Med. 35, 1171–1179.
- Pluijms, W.A., van Mook, W.N., Wittekamp, B.H., and Bergmans, D.C. (2015). Postextubation laryngeal edema and stridor resulting in respiratory failure in critically ill adult patients: updated review. Crit. Care 19, 295.
- Sinha, A., Agarwal, A., Gaur, A., and Pandey, C.K. (2001). Oropharyngeal swelling and macroglossia after cervical spine surgery in the prone position. J. Neurosurg. Anesthesiol. 13, 237–239.
- Sud, S., Friedrich, J.O., Taccone, P., Polli, F., Adhikari, N.K.J., Latini, R., Pesenti, A., Guérin, C., Mancebo, J., Curley, M.A.Q., et al. (2010). Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med. 36, 585–599.
- Sutherasan, Y., Theerawit, P., Hongphanut, T., Kiatboonsri, C., and Kiatboonsri, S. (2013). Predicting laryngeal edema in intubated patients by portable intensive care unit ultrasound. J. Crit. Care 28, 675–680.
- Szabo, M., Denman, W., Marota, J., and Roberts, J. (1997). EVALUATION OF AIRWAY EDEMA IN PATIENTS OPERATED ON IN THE PRONE POSITION. J. Neurosurg. Anesthesiol. 9, 380.
- Wang, Y., Lu, X., Chen, H., Chen, T., Su, N., Huang, F., Zhou, J., Zhang, B., Li, Y., Yan, F., et al. (2020). Clinical Course and Outcomes of 344 Intensive Care Patients with COVID-19. Am. J. Respir. Crit. Care Med.
- Watanabe, K., and Nakaya, M. (2011). Images in clinical medicine. Laryngopharyngeal edema. N. Engl. J. Med. 364, e55.
- Wittekamp, B.H.J., van Mook, W.N.K.A., Tjan, D.H.T., Zwaveling, J.H., and Bergmans, D.C.J.J. (2009). Clinical review: post-extubation laryngeal edema and extubation failure in critically ill adult patients. Crit. Care 13, 233.
- Yang, X., Yu, Y., Xu, J., Shu, H., Xia, J. ’an, Liu, H., Wu, Y., Zhang, L., Yu, Z., Fang, M., et al. (2020). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med.
- Zytoun, T., Noeman, Y., Abdelhady, M.A., and Waly, A. (2019). The role of laryngeal ultrasound in predicting postextubation laryngeal edema. Research and Opinion in Anesthesia and Intensive Care 6, 294.
View all COVID-19 updates
Learn about research in the Division of Pulmonary and Critical Care Medicine