Changing Lives With a Device for the Tongue
In This Article
- For the first time ever, a multicenter clinical trial led by Christopher J. Hartnick, MD, and Brian Skotko, MD, MPP, has established the efficacy and safety of hypoglossal nerve stimulation in children with Down syndrome
- They have also found reason to believe the treatment could improve neurocognition among the patient cohort
- Published in JAMA Otolaryngology–Head & Neck Surgery, findings from the trial revealed that 73.2% of patients experienced a change in their apnea-hypopnea index (AHI) from severe to moderate one year after implantation
- The average decrease in AHI across the total number of participants was greater than 50%
- OSA-18 quality-of-life surveys reported significant improvements in daily functioning, behavior and language, and more than three-fourths of all patients demonstrated either moderate or large improvements to survey scores
Subscribe to the latest updates from Otolaryngology Advances in Motion
Children with Down syndrome seldom enjoy a good night's rest. Just ask their parents, who often notice their child tossing and turning, snoring, or waking up throughout the night. The lack of quality sleep might cause their child to wake up irritated with little energy and less willingness to engage in school or with peers.
Clinicians have attributed much of these bedtime woes to a condition called obstructive sleep apnea (OSA), which occurs when breathing stops and restarts during sleep. The condition arises from an obstructed airway and runs rampant in children with Down syndrome; about 80 percent of children with Down syndrome have OSA, compared to five percent of the general pediatric population.
An adenoidectomy and tonsillectomy—surgical procedures to remove the adenoids and tonsils from the back of the throat—are the first treatments available to children with OSA. Removing these structures widens the airway, and, if OSA symptoms persist, a continuous positive airway pressure, or CPAP machine, can provide further relief. Unfortunately, several anatomic and physiologic features characteristic of children with Down syndrome can render these treatments ineffective. The wide tongue base and low muscle tone common among these children can further restrict the airway, and hypersensitivity around their faces can make the masks used for CPAP feel unbearable.
"Many of our patients with Down syndrome simply cannot tolerate CPAP despite lots of committed attempts at desensitization techniques," said Brian Skotko, MD, MPP, the Emma Campbell endowed chair on Down Syndrome at Massachusetts General Hospital. "We would reach a point where we simply ran out of good options to treat apnea in these patients, which was frustrating for their families."
In recent years, hypoglossal nerve stimulation has intrigued clinicians as another possible solution. But, despite its approval by the U.S. Food and Drug Administration (FDA) for adults, the government agency has yet to approve the treatment for children, prompting Christopher J. Hartnick, MD, professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School and division director of Pediatric Otolaryngology–Head and Neck Surgery at Mass Eye and Ear, to set a new precedent.
For the first time ever, a multicenter clinical trial led by Drs. Hartnick and Skotko has established the efficacy and safety of hypoglossal nerve stimulation in children with Down syndrome and, in the process, revealed an unexpected, albeit galvanizing, finding.
"It was one thing for us to see these kids sleeping better and feeling less tired," said Dr. Hartnick, whose study was published in JAMA Otolaryngology–Head & Neck Surgery. "But we didn't expect parents to tell us how much better their children were speaking, following conversations, and performing in school."
A Pacemaker for the Tongue
Hypoglossal nerve stimulation relies on a battery-powered device implanted under the skin of the chest that stimulates the hypoglossal nerve, which controls the tongue. When activated by a remote, the device moves the tongue forward, thereby clearing the airway while a person sleeps. Prior to Dr. Hartnick's study, the device was approved by the FDA in 2014 as a secondary treatment for adults with OSA who cannot tolerate using a CPAP machine.
In 2019, Mass Eye and Ear opened its Hypoglossal Nerve Stimulator Program and has since established itself as a world leader for the treatment. According to Phillip A. Huyett, MD, assistant professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School and director of Sleep Surgery at Mass Eye and Ear, the hospital has already implanted the most stimulators in New England—more than 300 devices have been implanted over the past three years. Inspire Medical Systems, Inc., the manufacturer of the only FDA-approved hypoglossal nerve stimulator, has recognized the hospital as one of nine programs nationally with a "Physician of Excellence," a distinction attributed not only to the total volume of devices implanted, but to the overall quality of care provided.
Thanks to its high volume of patients, Mass Eye and Ear has made remarkable strides toward streamlining the treatment. According to Dr. Huyett, the time required to implant the device has shrunk from approximately three hours to well under 60 minutes, and more than 80 percent of those patients implanted at Mass Eye and Ear have responded positively.
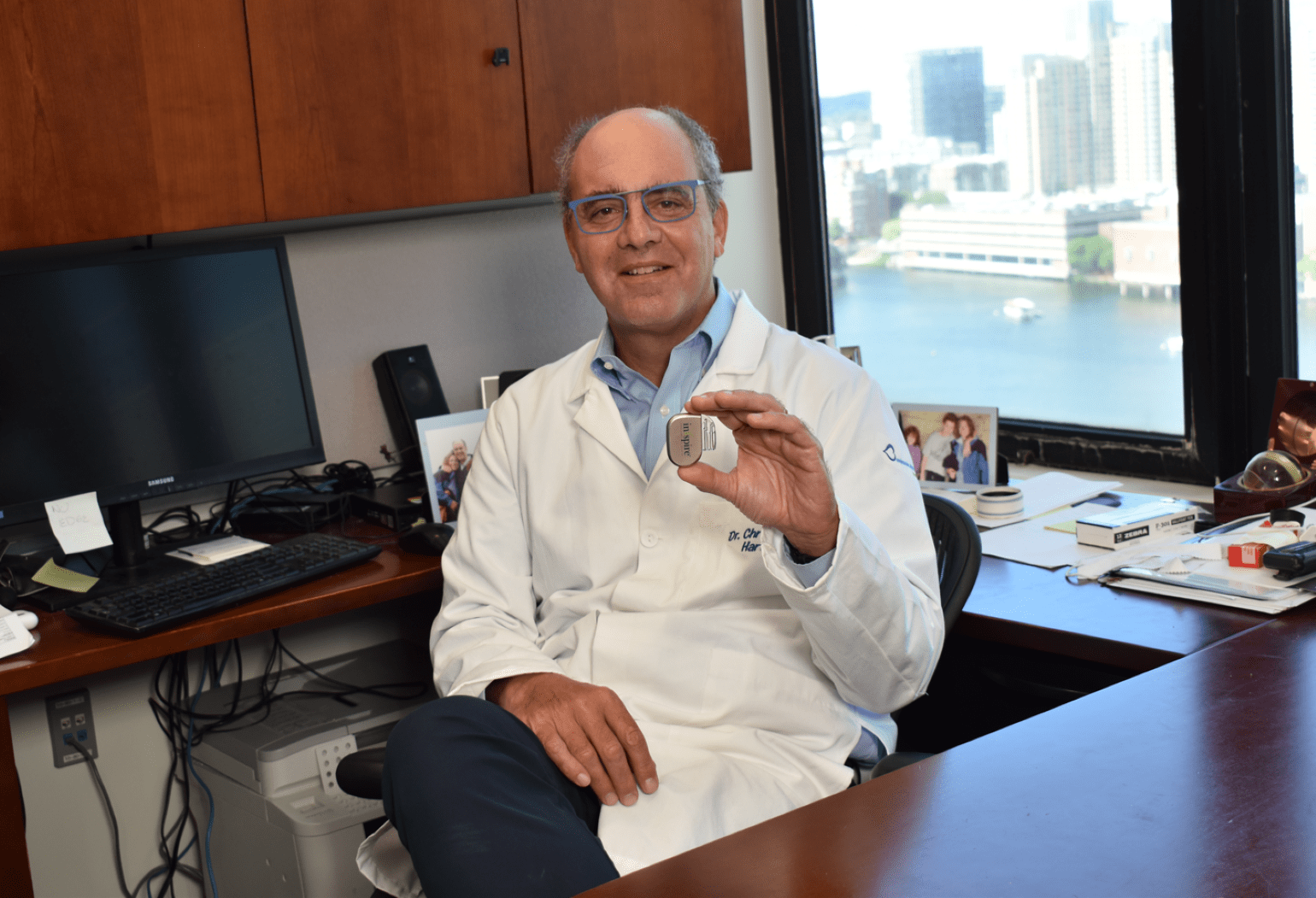
Figure 1
Christopher J. Hartnick, MD, holding a hypoglossal nerve stimulator device in his office. Image courtesy of Dr. Hartnick.
"It's not uncommon for adult patients and their bed partners to call this a life-changing therapy," said Dr. Huyett, who likens the device to a pacemaker for the tongue.
Understanding what patients with untreated OSA experience every night helps explain these extraordinary outcomes. Without realizing it, a person who stops and restarts their breathing while they sleep is actually arousing their brain out of its sleep cycle. According to Dr. Huyett, the subsequent fragmented sleep can affect all different facets of life, including daytime alertness and performance at work or school.
"Think back to any time when you've had a rough night of sleep, or pulled an all-nighter," he said. "How well did you perform in school or at work the next day? Now imagine that in perpetuity."
For children with Down syndrome, this sleep disruption can put them at an even greater disadvantage.
Better Sleep, Better Quality-of-Life
Clinicians have long relied on tongue base reduction surgeries as secondary treatment options for OSA in children with Down syndrome. However, the treatment usually comes at a significant cost: Children typically spend a few days in an intensive care unit recovering from the surgery without any guarantee of a successful outcome.
Inspired by the success of hypoglossal nerve stimulation in the adult population, Dr. Hartnick took the first steps toward a less invasive, less painful approach in 2015 when he became the first surgeon in the United States to implant a hypoglossal nerve stimulator in a pediatric patient. Determined to convince the FDA of its efficacy and safety in children with Down syndrome who are under the age of 18, Dr. Hartnick subsequently launched a phase I clinical trial across five U.S. medical centers.
Forty-two patients with Down syndrome between the ages of 10 and 22—all exhibiting persistent, severe OSA after the removal of their tonsils and adenoids—were enrolled in the FDA-approved trial. Before and after implanting the device in each patient, the team measured the patients' apnea-hypopnea indexes (AHI). Experts use AHI to measure the severity of sleep apnea by counting the number of sleep apnea events per hour during a sleep study. A higher AHI, therefore, indicates a more severe case of sleep apnea.
According to results published in JAMA Otolaryngology–Head & Neck Surgery, 73.2% of patients experienced a change in their AHI from severe to moderate one year after implantation, and the average decrease in AHI across the total number of participants was greater than 50%. Just under 12% of patients reported temporary tongue or oral discomfort—the most common complication from the procedure—which resolved within a two-week span, and no patients required removal of their device.
In addition to validating the safety and efficacy of the device, feedback from families hinted at how the device might help improve neurocognition. OSA-18 quality-of-life surveys reported significant improvements in daily functioning, behavior and language, and more than three-fourths of all patients demonstrated either moderate or large improvements to survey scores. The survey asked questions related to sleep disorders, physical distress, emotional distress, diurnal problems and caretaker occupation before and after the child's implantation, and parents marveled at their child's improved ability to engage socially and speak clearly.
"These children were no longer the first ones sleeping through their classes, nor were they the first ones heading to bed at a sleepover," Dr. Hartnick said. "This is the next step forward in allowing them to participate in school, transition from childhood into adulthood and hold jobs."
New Questions on Neurocognition and Speech Recognition
Dr. Hartnick speculates that hypoglossal nerve stimulation could improve neurocognition and speech recognition in children with Down syndrome for a variety of reasons. The most obvious, he believes, is the device's ability to improve the quality of sleep these children receive, which leads to higher levels of energy and an increased attention span. Another plausible thought, he added, is the long-term effect of the device on a child's enlarged tongue base. By stimulating the tongue overnight, the device might inadvertently strengthen the muscles of the tongue and improve the child's ability to move it during the day. Enhanced tongue mobility would allow the child to better annunciate their words, vastly improving their speech.
To find a definitive answer, Drs. Hartnick and Skotko are pivoting their research with the support of a $4 million, five-year grant from the National Institutes of Health. Under the grant, the researchers will collaborate with neuropsychologists and speech-language pathologists to examine measurements of IQ, memory, mood, and expressive language among children with Down syndrome before and after implantation of the hypoglossal nerve stimulator.
Meanwhile, Mass Eye and Ear will continue to test new ways of improving intervention strategies for treating OSA. In July 2022, Dr. Huyett became the first surgeon in New England to implant a Genio device,* an experimental type of hypoglossal nerve stimulator that is not implanted into the chest and does not rely on a battery. Instead, the device uses two electrodes connected to both sides of the hypoglossal nerve underneath the chin. During bedtime, patients place an activation chip under their chin, which clears the airway by activating both electrodes.
The device is not being used in Drs. Hartnick and Skotko's future studies on neurocognition but offers plenty of excitement about future innovations to the treatment.
"Mass Eye and Ear is home to some of the most exciting work happening in hypoglossal nerve stimulation and sleep apnea," said Dr. Skotko. "I couldn't think of a better place for us to conduct the next stage of our research."
*Please note: Nyxoah Genio is an investigational device limited by Federal (or United States) law to investigational use.
Learn more about the Department of Otolaryngology–Head and Neck Surgery at Mass Eye and Ear
Refer a patient to Mass Eye and Ear/Mass General Brigham