Most Patients Believe Marijuana Is Effective for Pain Relief After Musculoskeletal Injury
Key findings
- Most adults surveyed after orthopedic trauma believe marijuana is a valid treatment for post-injury and postoperative pain
- Most patients who used marijuana during their recovery from musculoskeletal injury say it helps alleviate their pain and reduces their use of opioid medication
- Most orthopedics patients surveyed are comfortable discussing medical marijuana with their health care provider
Do patients believe that marijuana is a valid medical treatment for pain after musculoskeletal injury? Researchers, led by orthopedic trauma surgeon Marilyn Heng, MD, MPH, FRCSC, and including chief of the Department of Orthopaedics Mitchel B. Harris, MD, of Massachusetts General Hospital, report in the Journal of Orthopaedic Trauma that most orthopedics patients they surveyed consider medical marijuana a valid treatment for post-injury and postoperative pain. Furthermore, in the subgroup of patients who used marijuana during their recovery, most said it helped alleviate their pain and reduced their use of opioid medication.
Subscribe to the latest updates from Orthopaedics Advances in Motion
When medical marijuana was legalized in Massachusetts in January 2013, physicians at two trauma clinics in that state fielded an increased number of inquiries about marijuana use during recovery from a fracture or soft-tissue musculoskeletal injury. The only highly validated evidence for marijuana as an analgesic comes from studies of chronic pain. Having no data about the benefits of medical marijuana for musculoskeletal injury, researchers surveyed 538 adult outpatients who had suffered a musculoskeletal injury one to six months earlier. Those patients were also asked to complete the PROMIS SF v1.0 – Anxiety 4a instrument, the Pain Catastrophizing Scale, and the short screening scale for DSM-IV posttraumatic stress disorder (PTSD).
Five-hundred patients (93%) completed the 35-question survey. Fifty percent were women, and the median age was 55 years (range, 18-93 years). Most of the patients (69%) had undergone surgery for their injury.
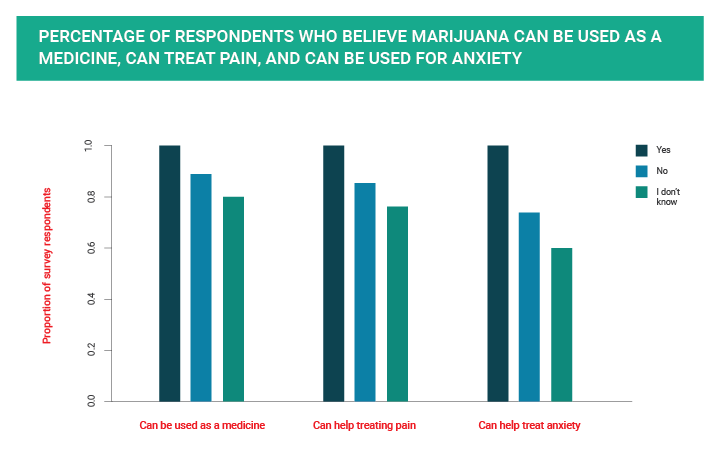
Asked whether marijuana can be used as a medical drug, 81% of respondents said yes, 12% were unsure and 7% said it cannot. Most patients believed marijuana can treat both pain (78%) and anxiety (62%), and older patients (age threshold not specified) were significantly less likely than younger adults to share these beliefs. Gender, type of injury and the need for surgery did not influence beliefs about the usefulness of marijuana as a medication.
Sixty percent of respondents reported having used marijuana at least once previously, including 21% who had used it within the past year and 13.6% (70 patients) who had used marijuana during their recovery from musculoskeletal injury.
Ninety percent of patients who used marijuana during recovery said it reduced their pain, and 81% said it reduced the amount of opioid medication they needed. Patients who use marijuana also had a significantly higher average anxiety score than patients who did not use marijuana during recovery. However, PTSD and PCS scores did not correlate with marijuana use during recovery.
A clear majority of respondents, 84%, said they would be very comfortable or comfortable discussing medical marijuana with their health care provider. Interestingly, only 59% knew that medical marijuana had been legalized in Massachusetts.
The researchers caution that this cross-sectional study cannot definitively correlate patients’ perceptions with actual improvement in pain or reduction in opioid use.
view original journal article Subscription may be required
About the Orthopaedic Trauma Center
Refer a Patient to the Orthopaedic Trauma Center