Opioid Prescription Refills More Common after TKA Than THA
Key findings
- A Mass General study found that total knee arthroplasty (TKA) patients were twice as likely to require refills of opioid prescriptions and had a greater total morphine equivalent dose over a longer period post-operatively when compared to total hip arthroplasty (THA) patients
- For the TKA patients, a comorbidity such as obesity increased the risk of refills by 3.1 times, while anxiety or depression increased it by 2.5 times
- Out of all opioid-naive TKA and THA patients, 41% required at least one refill opioid prescription after surgery, with 63% requiring one refill, 25% two refills, and 12% more than two refills
- For both TKA and THA patients, 80% could control pain using over-the-counter medications one month after surgery, and 100% could at three months out
Subscribe to the latest updates from Orthopaedics Advances in Motion
With opioid use for musculoskeletal pain having increased by 50% in the last 15 years, researchers are increasing their focus on improving guidelines for post-surgical opioid use. A main goal is to prevent chronic use. To inform such guideline creation on joint replacement surgery, a Massachusetts General Hospital team set out to answer three questions, with the results of the study published in The Journal of Arthroplasty:
- What is the postoperative opioid use rate for opioid-naïve patients undergoing total joint replacement?
- Does opioid use differ between total knee replacement and total hip replacement patients?
- Are there factors associated with the need for refill opioid prescriptions following joint replacement?
The team conducted a retrospective review of 205 total knee arthroplasty patients (TKA) patients and 214 total hip arthroplasty patients (THA) from January 2016 to March 2017 to assess opioid use patterns. The study only included patients considered opioid-naïve, defined as no long-term narcotic use, including one year prior to surgery.
Using patients’ medical records and a state online prescription-monitoring program (that includes information from 20 other states), the team made calculations of the number of filled prescriptions (grouped by refill status), total morphine equivalent dose (MED), quantity of pills, and date of last opioid prescription. Data on prescriptions were 62 days post-operatively, as no prescriptions were filled beyond that time according to the online program. Also, during the post-operative period, no patient received a prescription for opioids from another provider.
To determine daily MED for each prescription and total MED for each patient, an online conversion tool was used. To determine differences in opioid use between TKA and THA, the groups were compared for overall means and independently for the refill and non-refill groups. Spearman Rho correlation coefficients were used to evaluate relationships between relevant comorbidities and the need for opioid refills. A stepwise multivariable logistic regression analysis separately assessed the THA and TKA groups to determine predictors for refill prescriptions.
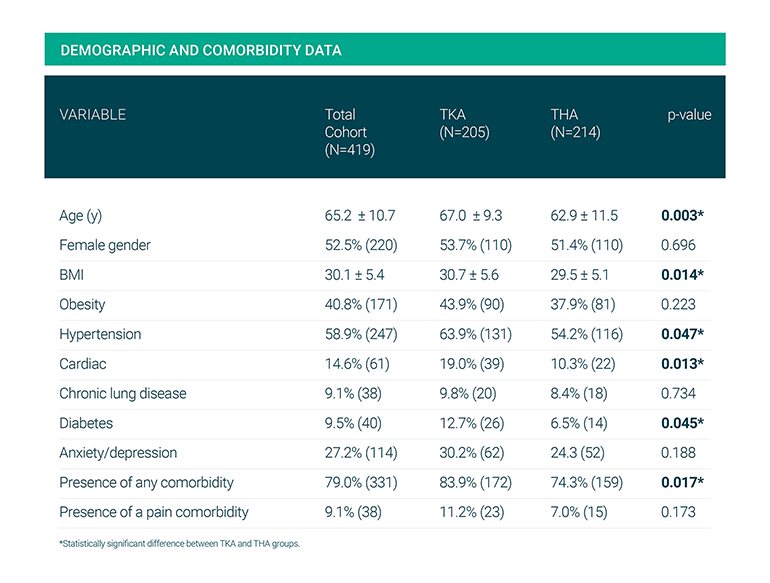
Fig. 1: Comorbidities Factored in Included Diabetes, Obesity, Hypertension, Congestive Heart Failure, Chronic Lung Conditions, Depression and Anxiety and Chronic Pain
A particular interest of the study was determining which factors influenced refills. Out of the total 205 TKA and THA patients, 36 patients (8.6%) did not fill a single prescription post-operatively and managed pain with over-the-counter medications. When compared to the patients who did fill a prescription, these patients were similar in composition as far as age (67.9 vs. 65.0), gender (61.1% female vs. 51.7% male), and BMI (29.1 vs. 30.2). The groups did not differ in prevalence of overall comorbidities, but a greater percentage of the patients with a filled opioid prescription were obese (42.6% vs. 22.2%) and had anxiety/depression (28.7% vs. 11.1%), compared to patients without a filled opioid prescription.
When researchers removed the 36 non-prescription fillers, the number of prescriptions, total quantity, MED and days on opioids were greater for TKA patients than for THA patients. More specifically, 56% of TKA patients had at least one refill compared to only 25% of THA patients (P < .001). In addition, 44% of TKA patients had more than two refills compared to only 20% of THA patients.
In the TKA group only, the risk of refills increased by 3.1 times if comorbidities were present (P = .003) and 2.5 times if patients were being treated for anxiety or depression (P = .004). TKA-associated refills, compared to THA-associated refills, were also for a greater quantity of pills and for a longer time period. On average, compared to the THA group, TKA patients were older (P =.003) and more likely to have a comorbidity (at 87% compared to 74.3%) and a higher BMI (P =.014).
Oxycodone accounted for over 80% of prescriptions written, while hydromorphone accounted for 10.7%, hydrocodone accounted for 1.8% and morphine sulfate accounted for 0.3%.
In conclusion, Mass General researchers found that 80% of patients could control pain using over-the-counter medications one month after surgery, and 100% could at three months out. While chronic use of opioids following joint replacement surgery is not common, this latest addition to research on post-surgical opioid use can inform those preparing future guidelines.
view original journal article Subscription may be required
Learn More About the Department of Orthopaedics
Refer a patient to the Department of Orthopaedics
