Infection Care Costs after THA Greatly Exceed Expectations
Key findings
- Modeled costs for standard of care to society for periprosthetic joint infections (PJI) after total hip arthroplasty (THA) greatly exceed previous cost estimates
- The cost differential between the current calculated results and prior estimates is attributed to factoring in indirect costs from lost wages and direct costs from failed treatments
- These findings add evidence to an existing argument that alternative treatment pathways should be explored
Subscribe to the latest updates from Orthopaedics Advances in Motion
Cost and outcome questions surround what constitutes optimal care for periprosthetic joint infections (PJI) after total hip arthroplasty (THA). To provide more financial clarity for future reviews, a Massachusetts General Hospital team calculated for the first time the long-term costs of PJI after THA, with the results of the study published in Clinical Orthopaedics and Related Research.
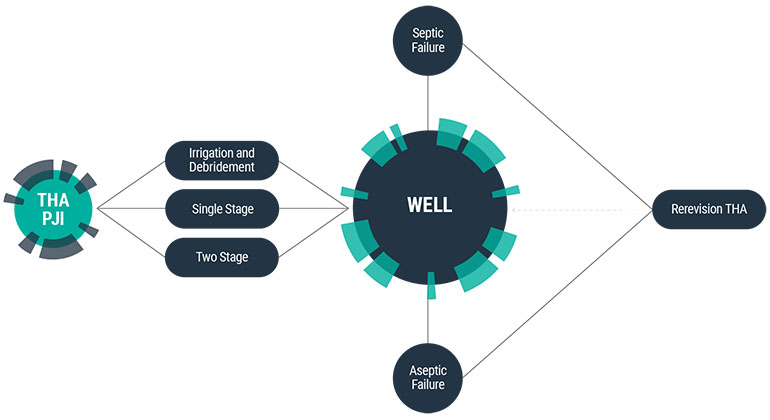
Fig. 1: The Flow Chart Shows the Different Health States of the Markov State-Transition Decision Model and the Various Pathways Along Which Patients May Transition with Time
A hypothetical “typical patient” model of standard of care, using real data, found a care-episode estimate that was more expensive than previous cost estimates. While other studies focused on direct costs only, Mass General researchers included indirect costs largely from lost income and direct costs from failed treatment.
To reach their conclusions, the team used a Markov state-transition model of a hypothetical patient of three working-age scenarios (55, 60 and 65 years). It assumed that a fixed percentage of patients underwent one of three treatments:
- Irrigation and debridement with modular exchange
- Single-stage revision
- The gold standard of two-stage revision
The Markov analysis’ algorithm used re-operation rates from septic and aseptic failure, and indirect and direct costs that were taken from peer-reviewed work in orthopedic and infectious disease journals and Medicare reimbursement data. Adjustments were made for uncertainty, incidence rates, costs of common complications and a 3% annual discount.
Researchers then compared their results with those of prior estimates of two-stage revision. The gold standard can have infection rates of up to 30%. Past studies revealed direct treatment costs of $100,000. The team’s new base case treatment estimate of $390,806 accounted for a 4.27% re-infection rate and the age of the patient at 65 with lost work and wages.
Results also evidenced that, as infection rates increased, overall costs did too. For example, a one-way sensitivity analysis revealed a care-episode range of $389,307 for a 65-year-old with a 3% re-infection rate and $412,091 at a 12% re-infection rate.
Also, the younger the patient at the time of infection, the more indirect costs rose. By lowering the patient’s age by five years to 60, total care costs went to $415,183 (assuming the base case 4.27% re-infection rate). For a patient at 55, costs were $441,986.
These findings add evidence to an existing argument that alternative treatment pathways should be explored. For example, mounting research supports single-stage revision over two-stage revision due to improved outcomes and lowered costs.
The Mass General team’s cost calculations are timely. Projections made within the orthopedic field are that a greater number of younger patients are undergoing THAs with a steady state of septic failures. As such, the estimates can be used for reference in future reviews of treatment paradigms.
view original journal article Subscription may be required
Learn more about the Center for Hip & Knee Replacement