Preserving the Chondrolabral Junction
In This Article
- Mass General orthopedists introduce new techniques for treating femoral acetabular impingement
- The techniques are able to contour bone growths without damaging the junction
- This technique offers a new frontier in stem cell treatment
Femoral acetabular impingement (FAI) is increasingly recognized as a cause of hip pain and early osteoarthritis, according to a 2014 study in the American Journal of Sports Medicine. Cam and pincer lesions or the bony growths associated with FAI can cause tears where the labrum joins the articular cartilage of the acetabulum. The articular cartilage covers the surface of the ball and the socket; it normally provides smooth movement within the chondrolabral junction.
Subscribe to the latest updates from Orthopaedics Advances in Motion
“That junction is critical in maintaining the health of the hip and preventing arthritis,” says Scott Martin, MD, director of the Joint Preservation Service within the Sports Medicine Center at Massachusetts General Hospital.
With FAI and labral tears, one of the first symptoms may be a subtle loss of motion in the hip region. By the time pain is present, significant damage has likely occurred.
“Young, active athletes will forcefully push their hip motion and then will compensate for any further lack of motion through the hemipelvis. That can lead to secondary injuries, such as hip flexor strains, adductor strains and lower back and sacroiliac joint problems, when the core problem is the hip joint itself,” says Dr. Martin, who has pioneered and implemented two new surgical strategies at Mass General to repair damage to this area.
Chondrolabral Junction Preservation and Capsular Augmentation
Many current surgical techniques for repairing the chondrolabral junction involve working through the defect itself. “But in so doing, these acetabuloplasty techniques can do more damage to the junction by detaching the labrum and compromising labral vascularity,” explains Dr. Martin.
For the past six years, Dr. Martin has been performing a new surgical approach that maintains the chondrolabral junction during acetabuloplasty, documented in a 2013 study published in the American Journal of Orthopedics. This approach doesn’t seem to have the limitations of more traditional ones that may disrupt the junction, such as by compromising labral blood flow and thus impairing healing ability.
For this approach, the surgeon enters underneath the capsule—above the injured area—and removes excess bone from the acetabular rim, while preserving the labrum and chondrolabral junction. FAI-causing bone growths are contoured without damaging the junction and the labrum is sutured. Such an approach can preserve the zone between the articular surface of the acetabulum and the labrum (Figures 1A and 1B).
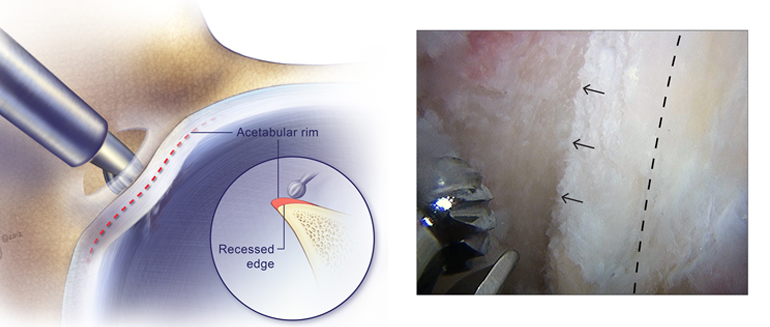
Figure 1A: Acetabular Recession of a Pincer Lesion (Original Location at Dashed Line) with a 4mm Round Abrader. Chondrolabral Junction (Arrows) Is Preserved
By avoiding a surgical lesion in this zone, the surgeon decreases the risk of predisposing the acetabulum to degeneration over time and developing early osteoarthritis. Since 2011, Dr. Martin’s team has performed over 1,500 labral repairs with this technique. Only a few university centers, including Mass General, currently perform these in high volume.
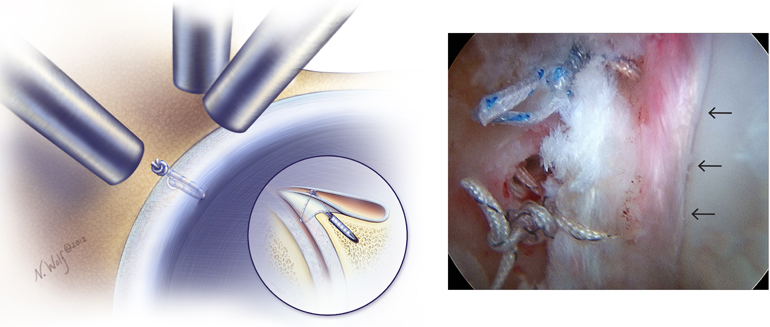
Figure 1B: Vertical Mattress Repair of the Torn Labrum with Restoration of the Labral Seal (Arrows) and No Labral Eversion
For cases in which the labrum is too damaged for reconstruction, Dr. Martin has developed an arthroscopic technique called capsular augmentation that restores labral structure without the use of grafted tissue from other regions of the patient’s body. This technique was published in Arthroscopy Techniques in 2015. With this approach, 5mm–8mm of hip capsular tissue located higher in the hip is surgically pulled down and attached to the labrum.
“It augments the repair and prevents the sutures from pulling through,” says Dr. Martin. He adds that using local capsular tissue is less complex and preserves the donor-tissue blood supply, in addition to preserving the chondrolabral junction to which the labrum is attached.
“This is a way to keep a patient’s own deficient labrum, by augmenting it with capsule and preserving the cartilage junction,” he explains. “It also provides an in-round seal.“
Maintaining a fluid seal is thought to protect the articular cartilage and minimize the risk of osteoarthritis. “When we do this, we have a very good seal,” he adds, which results in better outcomes. Since Dr. Martin developed the technique at Mass General, he has performed approximately 450 capsular augmentation procedures. He began performing the technique with higher frequency in 2013 after earlier successful results.
Recovery and Prevention
The Joint Preservation Service team at Mass General is also pursuing new biologics-based research using mesenchymal stem cells (MSC) harvested from the ilium to promote post-arthroscopic healing. The approach involves aspirating bone marrow from the ilium and then separating the MSCs by centrifuging in the operating room—enriching them with blood factors to form a “blood clot,” or “megaclot,” that is then placed over the repaired surface.
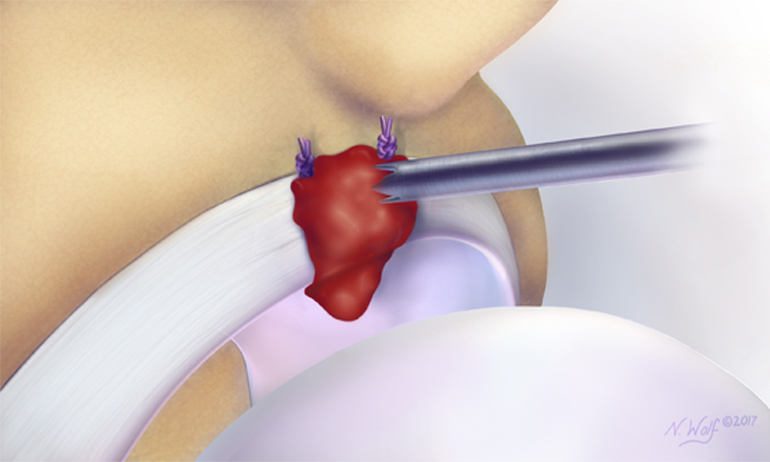
Fig. 2: “Megaclot” Application to the Chondrolabral Junction and Labral Repair Site.
“Our goal is not only to maintain what you have, but also to promote healing in that area,” says Dr. Martin, who has introduced this technique to nearly 100 patients within the past year and is planning a larger study (Figure 2).
Ideally, physicians would be able to diagnose the condition before serious damage has occurred. Newer imaging techniques, says Dr. Martin, allow viewing of the chondrolabral junction to diagnose lesions that would not show up for several more years on conventional imaging.
“Most of the surgery we currently perform is to halt progression of the arthritic disease process in the hip,” he says. “The whole point is to prevent cartilage degradation and preserve the joint before it’s too late.”
Learn about Mass General’s Sports Medicine Center
Refer a Patient to Mass General’s Sports Medicine Center