Enhanced Glycolysis Is a Main Driver in Squamous Cell Carcinoma
Key findings
- In this study, researchers at the Massachusetts General Hospital Cancer Center investigated what metabolic adaptations might underlie squamous cell carcinoma (SCC)
- SIRT6, a protein deacylase that has a pivotal role in glucose metabolism, was found to act as a tumor suppressor in SCC by modulating glycolysis
- An aggressive SCC phenotype in Sirt6-deficient mice was linked to a significant increase in highly proliferating CD34+ tumor-propagating cells (TPCs)
- RNA sequencing of Sirt6-deficient TPCs showed enhanced glutathione metabolism, lipid metabolism and amino acid transport, suggesting "rewiring" of metabolism that is crucial to the tumorigenic potential of these cells
- These results suggest an opportunity to target a specific subpopulation of TPCs in SCC by modulating glucose metabolism
In 1931, Otto Warburg observed that cancer cells preferentially rely on aerobic glycolysis instead of oxidative phosphorylation for energy production. "The Warburg effect" has been considered a late adaptation of rapidly proliferating advanced tumors, but recently it's been noted in tumor-initiating cells in several cancer types.
Subscribe to the latest updates from Oncology Advances in Motion
Now Raul Mostoslavsky, MD, PhD, the Laurel Schwartz professor of oncology at the Massachusetts General Hospital Cancer Center, and colleagues have demonstrated that enhanced glycolysis is a main driver in squamous cell carcinoma (SCC). In Nature Metabolism, they also identify a subset of tumor-propagating cells (TPCs) as the cell of origin for the Warburg effect in SCC.
Sirt6 as Tumor Suppressor
The researchers correctly reasoned that SIRT6, a protein deacylase that has a pivotal role in glucose metabolism, could act as a tumor suppressor in SCC by modulating glycolysis:
- Almost all human samples and cell lines of head and neck SCC exhibited loss of SIRT6
- When mice were genetically engineered to lack Sirt6 in the skin epithelium and were injected with a carcinogen, they showed earlier SCC onset, larger tumors and greater tumor cell proliferation than wild-type mice
Evaluation of TPCs
Rather than being a late adaptation, enhanced glycolysis in SCC occurred in TPCs:
- The aggressive SCC phenotype was linked to a significant increase in highly proliferating CD34+ TPCs
- Highly glycolytic CD34+ TPCs were characterized by higher glutathione metabolism and stemness, providing a defense against oxidative stress that was robustly enhanced upon Sirt6 loss
Further Analyses
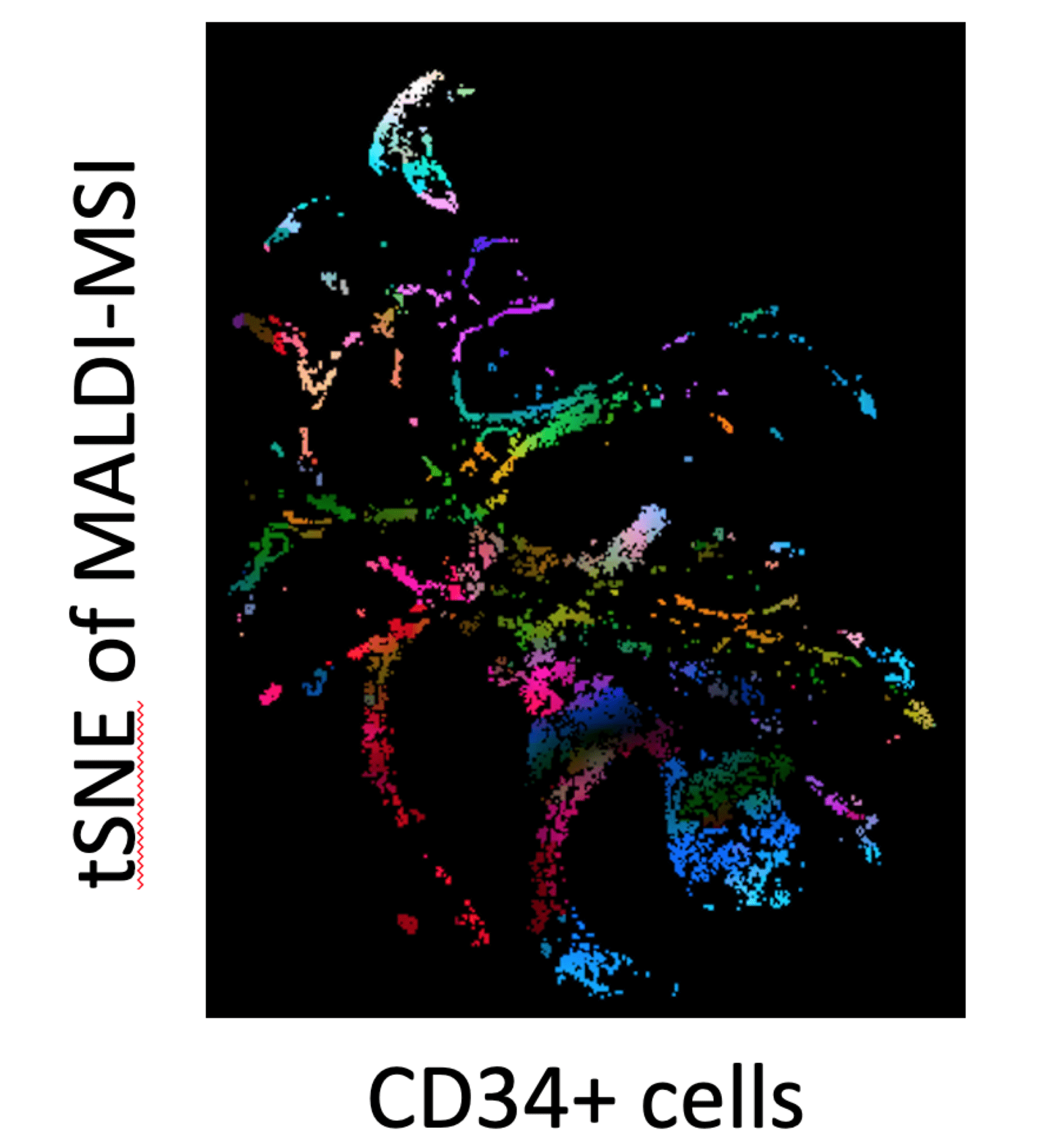
Figure 1
A t-distributed stochastic neighbor embedding (t-SNE) image of MALDI Mass Spectroscopy Imaging (MSI) showing metabolomic signatures in Squamous Cell Carcinoma Cells. Differences in color and position denotes differences in metabolites. The high range of colors and distances indicate high metabolic heterogeneity. Credit: Jeeeun Choi, Walid Abdelmoula, Nathalie Agar.
- Metabolite profiling showed that the generation of antioxidants and nucleotides through the oxidative phase of the pentose phosphate pathway was largely responsible for the aggressive SCC phenotype
- RNA sequencing of Sirt6-deficient TPCs showed enhanced glutathione metabolism, lipid metabolism and amino acid transport, suggesting "rewiring" of metabolism is crucial to the tumorigenic potential of these cells
Hope for the Future
TPCs have emerged as attractive therapeutic targets in SCC and other cancers because of their capacity for tumor initiation and self-renewal. These new results suggest an opportunity to target a specific subpopulation of TPCs in SCC by modulating glucose metabolism.
view original journal article Subscription may be required
Learn about the Mostoslavsky Lab
Refer a patient to the Mass General Cancer Center