A New Approach to Induced Hypertension for Large Vessel Stroke
Key findings
- In the care of patients with large vessel stroke, new approaches are needed to preserve penumbral tissue and prevent growth of core occlusions, thereby increasing the number of candidates for endovascular thrombectomy and improving its results
- In small human studies, induced hypertension was found to be safe and improved function as one component of treating acute ischemic stroke
- Neurosurgeons at Massachusetts General Hospital have developed an algorithm for treating large vessel stroke with induced hypertension
- The most likely candidates for induced hypertension are patients with expected delay to endovascular thrombectomy and those with persistent large vessel occlusion afterward
Subscribe to the latest updates from Neuroscience Advances in Motion
Endovascular thrombectomy has become the standard of care for eligible patients with large vessel occlusion, ushering in a new era in the field of stroke. The next step, according to a team of experts at Mass General, is to preserve penumbral tissue and prevent growth of core occlusions, thereby increasing the number of candidates for endovascular thrombectomy and improving its results.
Published in Frontiers in Neurology, the team reviews blood pressure manipulation as one component of “penumbral sustenance” and presents an algorithm for inducing hypertension. The authors, include James D. Rabinov, MD, Aman B. Patel, MD, Joshua A. Hirsch, MD, and Thabele M. Leslie-Mazwi, MD, of Mass General.
The researchers explain that preservation of blood flow to the penumbra depends on maintaining cerebral perfusion pressure. Because the ischemic areas are already maximally dilated with loss of autoregulation, even a minimal reduction in perfusion pressure may be detrimental to the pressure passive system. Allowing or inducing hypertension enhances cerebral blood flow, and therefore neuronal support in the penumbra.
Dr. Leslie-Mazwi’s team describes small human studies in which induced hypertension has been safe and effective as one component of treating acute ischemic stroke. The most widely researched approach is pressor therapy with phenylephrine, which has been less likely than norepinephrine and other vasoactive agents to cause tachyarrhythmias. The intervention is controversial, the authors acknowledge, but they find it analogous to inducing hypertension in patients with subarachnoid hemorrhage who are experiencing vasospasm.
Patients most likely to benefit from induced hypertension are those with expected delay to endovascular thrombectomy, persistent large vessel occlusion following thrombectomy (unsuccessful or partially successful recanalization) or those who are not candidates for thrombectomy for other reasons. The authors’ approach to the procedure is outlined in the figure (below).
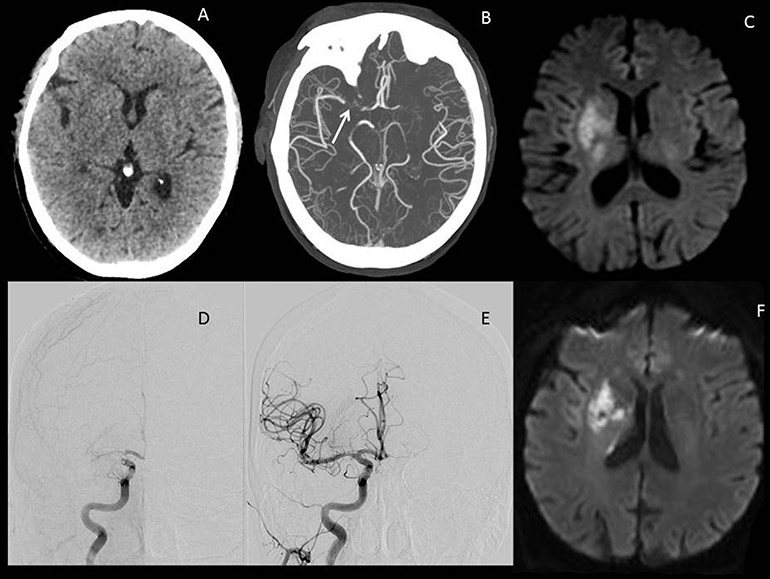
Figure 1
Illustrative images of a large vessel occlusion (LVO) stroke patient. Patient was a 67-year-old male presenting 4 h after onset with a full right middle cerebral artery (MCA) syndrome due to right MCA occlusion, NIHSS 14.
Dr. Leslie-Mazwi and colleagues caution that contraindications to induced hypertension for acute care of large vessel stroke generally include intracranial hemorrhage, congestive heart failure, active coronary ischemia (changes on electrocardiogram or troponin leak) or existing autoregulation to systolic blood pressure >200. Exposure to intravenous thrombolytic therapy is not a contraindication but limits the upper extent of blood pressure elevation, as research by others has shown that higher blood pressure is associated with worse outcomes and symptomatic hemorrhage in these patients.
The authors also review investigational treatments for patients who have large areas of cortical and white matter injury. These include neuroprotective agents, which act acutely, and agents designed to enhance repair of damaged tissue, which act from post-stroke weeks two to 12 and beyond. The latter agents will be particularly important, the authors say, as more patients survive the acute stroke period in the new era.
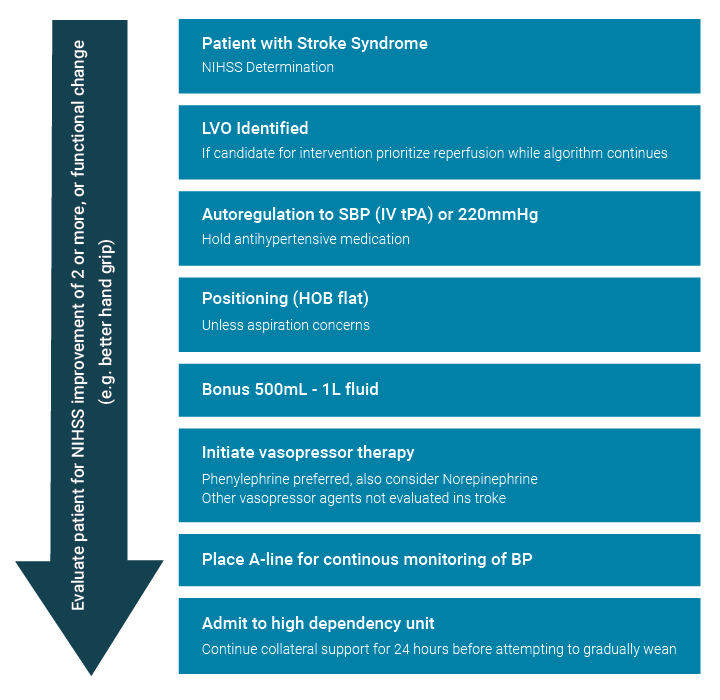
Figure 2
Algorithm for approach to hypertensive support for large vessel occlusion (LVO) patient. Reperfusion therapy should be the priority, but the algorithm provides for collateral support either while awaiting reperfusion (e.g., transfer to endovascular capable facility) or if reperfusion is not an option.
view original journal article Subscription may be required
Learn more about the Cerebrovascular Program at Mass General
Learn more about stroke care at Mass General