Advantages of Robot-assisted Techniques for Urologic Surgeries
In This Article
- Robotic surgery can decrease blood loss and patient pain, and lead to a shorter recovery time than a traditional laparoscopic approach
- A robotic approach can also offer surgeons a shorter learning curve
- Surgeons and engineers are working to improve robotic instrument feedback and imaging
Subscribe to the latest updates from Urology Advances in Motion
Robot-assisted approaches to complex surgeries of the urinary tract and male reproductive organs have key advantages over open surgery and even traditional laparoscopic surgical techniques, according to a 2014 meta-analysis in the American Journal of Robotic Surgery. While rates of success and complications are similar with robotic versus open or traditional laparoscopic surgery, the findings reveal that robotic surgery decreases blood loss, patient pain and analgesic requirements. It also shortens hospital stays and recovery time for urologic procedures. The downsides to robotic surgery are higher costs, longer time in the operating room and uncertainty about long-term outcomes, as the technology is relatively new.
Robot-Assisted Surgery
A decade ago, Douglas Dahl, MD, chief of Urologic Oncology at Massachusetts General Hospital, introduced a surgical robot to the hospital’s Department of Urology, making the department one of the first in the country to adopt the new technology. Building upon their extensive experience in minimally invasive surgery techniques, Dr. Dahl and Shahin Tabatabaei, MD, director of the Prostate Health Program, began using the robot to perform radical prostatectomies, with 500 currently performed annually at Mass General.
Urology departments nationwide have become leaders in robot-assisted surgery, says Dr. Dahl, because precision is so critical for surgeries of the pelvis. Not only is the pelvic region tightly packed with sensitive organs, it is also highly vascular—crowded with easily punctured arteries and veins. Robot-assisted surgery also has a shorter learning curve than open or laparoscopic surgery, and that has contributed to its growing popularity, according to a 2014 study published in European Urology. But using a robot does not obviate the need for surgical experience. The robot is “more of an avatar than a robot,” says Dr. Dahl. “Successful robotic surgery still has everything to do with the surgeon’s skill.”
Advantages of a Robotic Approach
Robot-assisted surgery, essentially an enhanced laparoscopic technique, has the following benefits:
- 3-D visualization and magnification of the operating site
- Enhanced brightness and resolution
- Deamplification of movement: scaling the movement of tools to distances that are up to five times smaller than the surgeon’s hand would make
- Improved wrist articulation
These capabilities allow for greater precision, miniaturization of instruments and smaller incisions than traditional laparoscopic approaches. Today, seven Mass General urology surgeons are licensed and trained to operate surgical robotic technology, which enables them to perform hundreds of complex urologic surgeries every year with both increased precision and less-invasive techniques (Figure 1).
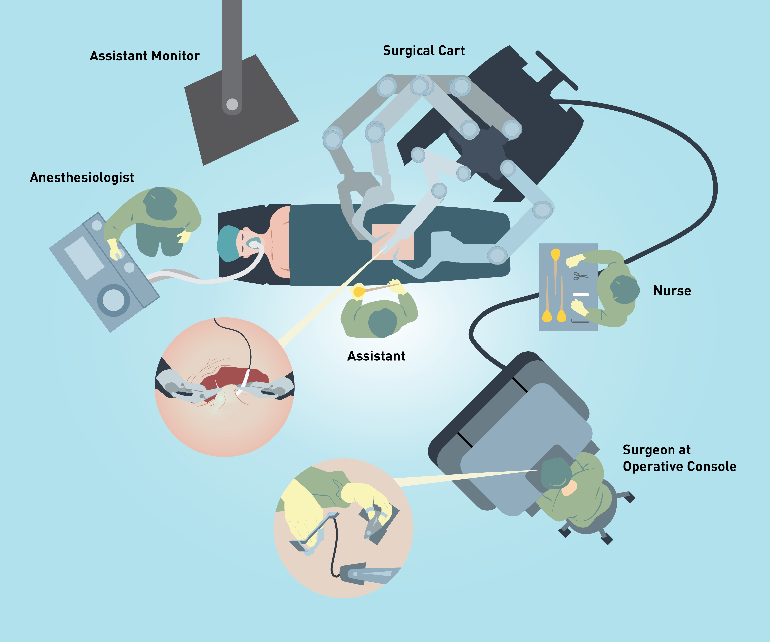
Figure 1: Operating Room Setup
Robot-assisted technique allows the surgeon at the operative console to remotely control miniature instruments with precision and with a magnified view of the surgical site. The interchangeable instruments follow the surgeon’s hand and wrist movements.
“As a result, the Mass General Department of Urology has become a major referral center for complex procedures that involve removal of prostate, kidney, ureter and pelvic cancers,” explains Dr. Dahl. “Other procedures include reconstructing urinary and reproductive organs following cancer treatment, cancer removal or other damage.”
In 2016, for instance, the hospital used the robot to perform 40 pyeloplasties, a reconstructive procedure that repairs the proximal part of the ureter (Figure 2). In addition, the Department of Urology uses robot-assisted surgery to perform many ureteral re-implantations—which repair damage to the ureter from other types of surgery, cancer or radiation treatment—as well as nephroureterectomies.
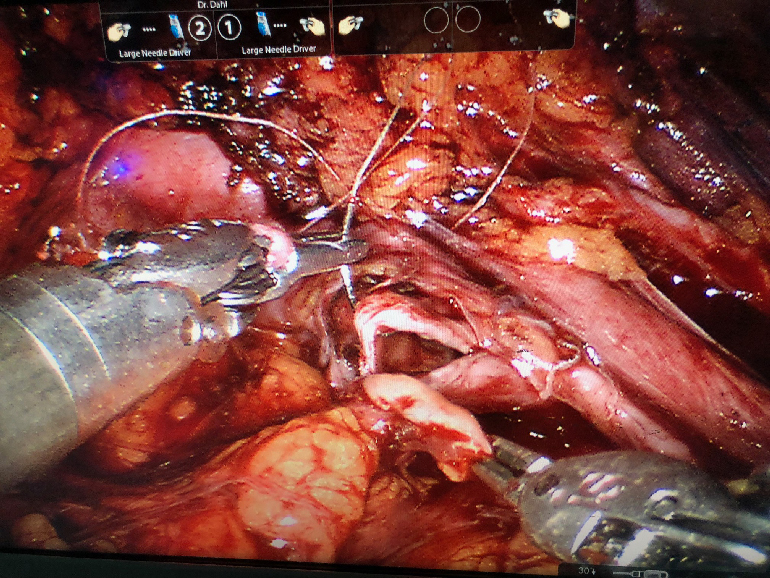
Figure 2: Robot-Assisted Laparoscopic Pyeloplasty as Seen on Monitor
The robot places an initial stitch through the apex of the ureteral spatulation, an incision in the cut end of a tubular structure that splays it open to a dependent portion of the pelvis. Ureteral spatulation is one of the most delicate, complex and critical steps in a laparoscopic pyeloplasty.
Next-Gen Robotics
Mass General has partnerships with Harvard University and MIT through the Consortia for Improving Medicine with Innovation and Technology (CIMIT) to advance robotic technology and develop new robotic techniques. One challenge they are working on is creating haptic feedback: transmitting resistance and pressure to the surgeon’s fingers from the robot’s tools. With this process, surgeons can feel how hard they are pulling on instruments or tissue, or how tightly they are sewing a stitch. This would help to prevent tearing or tissue damage.
CIMIT is also working on incorporating magnetic resonance imaging into the robotic system, as well as the ability to shine different wavelengths of light into the surgical site. These additions would allow a surgeon to see things not visible to the naked eye, such as blood flow to a particular area or the precise location of cancer cells.
“These technologies are improving incrementally, and it's amazing the new things that can be done as we gain experience,” concludes Dr. Dahl.
About Mass General Urology robotics and minimally invasive surgery