Multiparametric MRI/Ultrasound Fusion Biopsy Improves Prostate Cancer Detection
In This Article
- Active surveillance (AS) has become an accepted way to manage prostate cancer in men at lower risk
- Multiparametric MRI can be used in conjunction with the standard transrectal ultrasound (TRUS)-guided biopsy to improve detection of clinically significant cancers
- The three components of the multiparametric MRI -- the T2-weighted image, the diffusion-weighted image (DWI) and the dynamic contrast-enhanced (DCE) view -- can confer a higher level of confidence to a radiologist’s diagnosis of pathologic changes in tissue
Subscribe to the latest updates from Urology Advances in Motion
After cancers of the skin, prostate cancer is the most common form of cancer, and the second most common cause of cancer death in men. Because of concerns about overtreatment of the disease, active surveillance (AS) has become an accepted way to manage the condition in men at lower risk. AS typically has included close surveillance of patients through a combination of digital rectal exams, measurement of prostate specific antigen (PSA) levels and interval prostate biopsies.
The standard transrectal ultrasound (TRUS)-guided biopsy that is part of AS and used for interval prostate biopsies can sometimes miss or understate clinically significant cancers. Multiparametric MRI—an imaging method that combines three inputs of functional and anatomic imaging to precisely map tissue anomalies (Figure 1)—can be used in conjunction with biopsy to improve detection of clinically significant cancers.
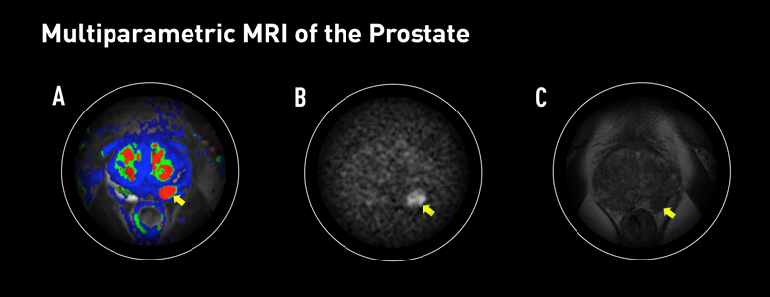
Figure 1: Multiparametric MRI of the Prostate
Multiparametric MRI can screen prostate cancer with more sensitivity and greater specificity than current technologies, which may miss or understage cancers. It uses a dynamic contrast enhancement color map (A), which shows intravenous contrast, allowing the radiologist to observe the rapidity with which the tissue is enhanced. Here, the image shows a focal area of abnormal perfusion indicated by the red color. The T2-weighted image (B) can identify tumors by their inherent difference from other areas of tissue. Diffusion-weighted imaging (C) displays the rate of water diffusion in tissues, which can assist in tumor delineation.
Urologists Adam Feldman, MD, MPH, and Matthew Wszolek, MD, both with the Massachusetts General Hospital Department of Urology and Mass General Cancer Center, have been successfully using multiparametric MRI-guided fusion biopsy in several types of patients:
- Men under AS who appear to have low-risk prostate cancer
- Men who have a prior negative TRUS-guided biopsy but still have clinical suspicion of significant cancer based on their PSA or other biomarkers, such as PCA3
- Men who have never had a biopsy, but have an elevated PSA or a questionable exam
Since beginning to use this approach in 2014, Drs. Feldman and Wszolek have tracked the use of fusion biopsy in their patients at Mass General. The team presented their results on the first 251 patients in September 2016 at the 85th Annual Meeting of the New England Section of the American Urological Association, published in The Journal of Urology.Their analysis of the data found that using the multiparametric MRI-guided fusion biopsy improves the detection of clinically significant prostate cancer over standard TRUS-guided biopsies alone (Figure 2).
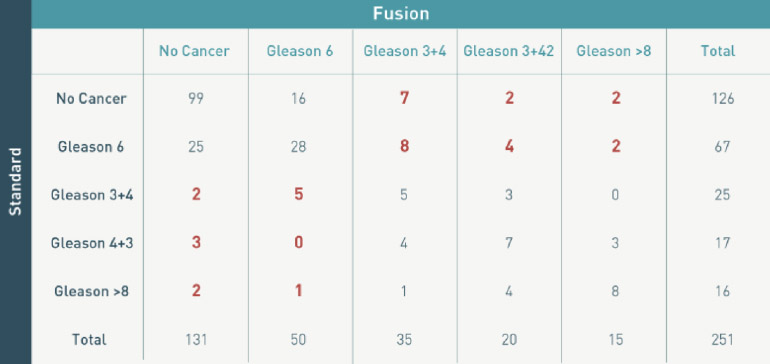
Figure 2: Detection Rates and Multiparametric MRI
Fusion biopsy improves the detection rate for clinically significant prostate cancer. The data also demonstrates that a significant proportion of Gleason Score 7 or higher lesions will not be detected by targeted biopsy alone, which indicates that standard template biopsies should remain an integral component of fusion biopsy programs.
However, their findings showed that a small but significant proportion of lesions with a Gleason Score of 7 or higher will not be detected by targeted biopsy alone. These findings point to the improved accuracy of fusion biopsy, but also indicate the necessary continued use of TRUS-guided biopsies in a fusion biopsy program.
Improving Outcomes with Better Imaging and Fusion Biopsy
In the fusion platform, the first procedure of fusion biopsy is a multiparametric 3 Tesla MRI, which is evaluated by a genitourinary radiologist specializing in prostate MRI. The evaluation has three components:
- The T2-weighted image identifies tumors by their inherent difference from other areas of tissue
- Diffusion-weighted imaging (DWI) displays the rate of water diffusion in tissue, leading to precise delineation of a clinically significant tumor
- Finally, a dynamic contrast-enhanced view (DCE) gives intravenous contrast and allows the radiologist to observe the rapidity with which the tissue is enhanced, helping to distinguish the tumor from normal tissue
Mass General Department of Radiology’s Mukesh Harisinghani, MD, director of Abdominal MRI, who is highly specialized in prostate cancer imaging and who also works as part of the Mass General Cancer Center’s multidisciplinary team of experts dedicated to prostate cancer care, notes that combining all three components can confer a higher level of confidence to a radiologist’s diagnosis of pathologic changes in tissue, dramatically improving accuracy. Before multiparametric MRI, areas of inflammation in the prostate gland were sometimes determined to be areas of tumor, yielding false positives.
Dr. Harisinghani emphasizes that there are also ways to optimize the multiparametric MRI to ensure a high quality of images, thereby allowing more precision in the detection of lesions. This allows radiologists to detect small foci of tumors, and its increased specificity improves accuracy, effectively determining non-cancerous tissue as well.
The second procedure of fusion biopsy is the biopsy itself. After the MRI, the radiologist outlines areas of suspicion. Those images are then transmitted to the computer in the procedure room and fused to the ultrasound image so that the anatomy of the prostate on the MRI matches what is seen on the ultrasound. Thus, the MRI guides the ultrasound evaluation and biopsy, allowing for more precise targeting of areas under investigation.
Learn more about the Department of Urology