Survivors of Critical Illness in COVID-19
The FLARE Four
- The majority of survivors of shock and respiratory failure develop post-intensive care syndrome (PICS). PICS is defined as new or worsened impairment after critical illness, which persists beyond hospital discharge, in one or more of three domains: cognition, mental health, or physical function. Similarly, PICS-Family (PICS-F) describes mental health impairments experienced by families of ICU patients
- Risk factors for developing PICS include shock, mechanical ventilation, prolonged sedation, delirium, and long periods of immobility. During an ICU course, assessment and management of pain/agitation/delirium, minimization of sedation, spontaneous awakening and breathing trials, early mobilization, and family engagement may improve patient and family outcomes. After hospital discharge, post-ICU clinics and peer support groups likely play an important role
- PICS can persist for months to years and may severely impair quality of life. These impairments may impact patients’ ability to return to work, adding to caregiver burden and compounding the financial toxicity of critical illness. Survivors of critical illness in general have reduced health-related quality of life, a higher risk of rehospitalization, and decreased long-term survival
- It remains unclear how many patients will experience PICS after COVID-19. However, given the increased number of patients experiencing critical illness, ARDS, and often long periods of sedation/immobility, we should be prepared to support a large population of patients and families experiencing long-term impairments after the ICU
Many people are saying...we need to understand and address the long-term outcomes of COVID-19 ICU survivors.
Subscribe to the latest updates from FLARE Advances in Motion
What are PICS and PICS-Family (PICS-F)?
Post-intensive care syndrome (PICS) is generally defined as new or worsened impairment following critical illness that persists beyond hospital discharge in at least one of three domains: cognition, mental health, or physical function (Needham et al. 2012). PICS is strikingly common, and often severe and enduring. The majority of ICU survivors have impairment in at least one PICS domain 12 months after hospital discharge, while 20-50% may experience persistent impairment in multiple domains (Maley et al. 2016; Marra et al. 2018; Needham et al., 2013; Pandharipande et al., 2013; Jackson et al., 2014) (yes - that Maley). Risk factors for development of PICS vary, but broadly include illness severity, duration of hospitalization, and ICU-related factors such as prolonged sedation, duration of delirium, and mechanical ventilation. Severe sepsis and ARDS, in particular, are associated with higher levels of cognitive, psychiatric, and physical dysfunction (Iwashyna et al., 2010; Mikkelsen et al, 2012).
Relatedly, PICS-Family (PICS-F) refers to impairments in mental health among family members or caregivers of ICU patients. PICS-F can similarly last for months to years after a loved one’s critical illness. PICS-F may manifest as anxiety, depression, complicated grief, sleep deprivation, and post-traumatic stress disorder (Davidson, Jones, and Bienvenu 2012).
Finally, survivors of critical illness (and their families) commonly experience joblessness and financial toxicity, which is defined as burdens associated with cost of medical care, lack of health insurance coverage, or other financial aspects of healthcare that may lead patients to debt and bankruptcy after the ICU (Kamdar et al. 2017; Hauschildt et al. 2020). They also report changes to family dynamics and interpersonal relationships as a result of PICS and the need for family members to serve in caregiver roles. All of these challenges, cumulatively, serve as tremendous challenges to the recovery and well-being of ICU survivors and their families.
Clinical Manifestations of PICS
The full magnitude of impairment in any of the three domains may not be apparent without the use of validated screening instruments, highlighting the importance of comprehensive assessment.
1) Cognitive impairment:
Screening for cognitive impairment can be performed at hospital discharge or in post-acute care settings via the Modified Mini-Mental State examination (MMSE), the Mini-Cog, or the Montreal Cognitive Assessment (MoCA). Of these, the MoCA, which incorporates tests of executive function, may be a more sensitive test for mild impairment, especially among previously high-functioning individuals (Nasreddine et al. 2005).
Cognitive impairment was well-described in the landmark BRAIN-ICU study (Pandharipande, Girard, and Ely 2014), the largest observational study to date of cognitive sequelae following critical illness. Among 821 survivors of respiratory failure or shock (6% of whom had cognitive impairment at baseline), 40% had cognition scores 1.5 standard deviations below population means (similar to that of moderate traumatic brain injury) and 26% had scores 2 standard deviations below population means (similar to that of mild Alzheimer's disease) at 3 months following hospital discharge (Figure 1). Impairment remained prevalent through the 12-month follow up. Longer duration of delirium was independently associated with impairment in cognitive and executive function at 3 months, and this impairment persisted at 12 months. Aspects of cognition commonly affected include memory, attention/concentration, executive function, and mental processing speed. Impairment in these areas may prevent individuals from following discharge plans (e.g. fluid/dietary restriction, medication adherence), as well as carrying out both daily functions and the higher-order complex cognition necessary for returning to work.
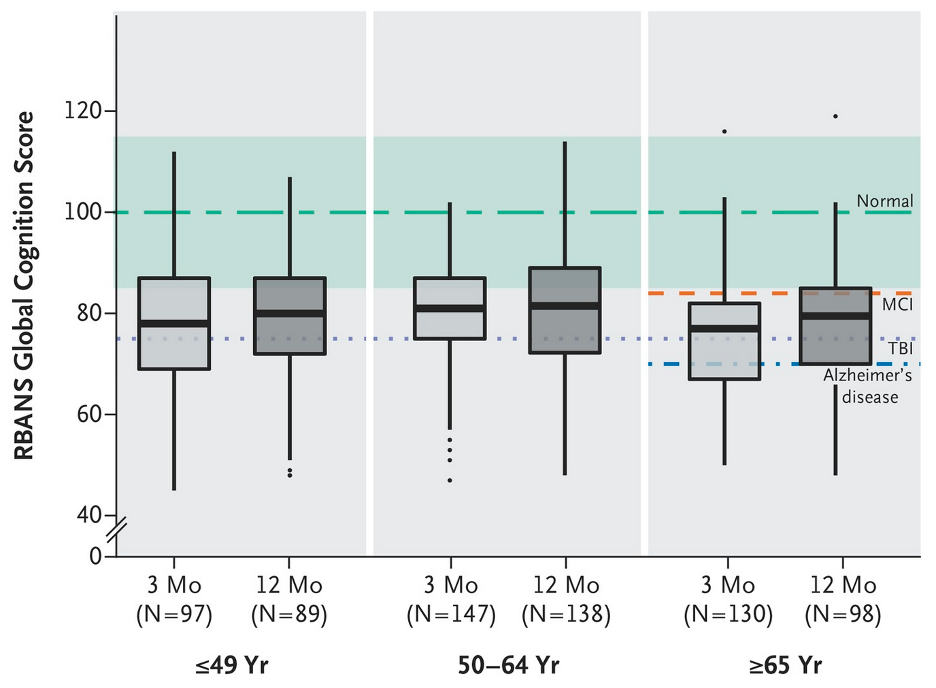
Figure 1
Age-adjusted global cognition scores on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS). Lower scores, indicating worse global cognition, are shown for ICU survivors at 3 and 12 months in patients after critical illness compared to the age-adjusted population mean for healthy adults (green dashed line and green band). Also included are the expected population means (based on prior cohort studies) for mild cognitive impairment (MCI, orange dashed line), moderate traumatic brain injury (TBI, dotted line), and mild Alzheimer's disease (blue dashed line). Adapted from Pandharipande, Girard, and Ely 2014.
Cognitive deficits after critical illness can often be striking when survivors are asked to carry out complex tasks on validated tests (Figure 2).
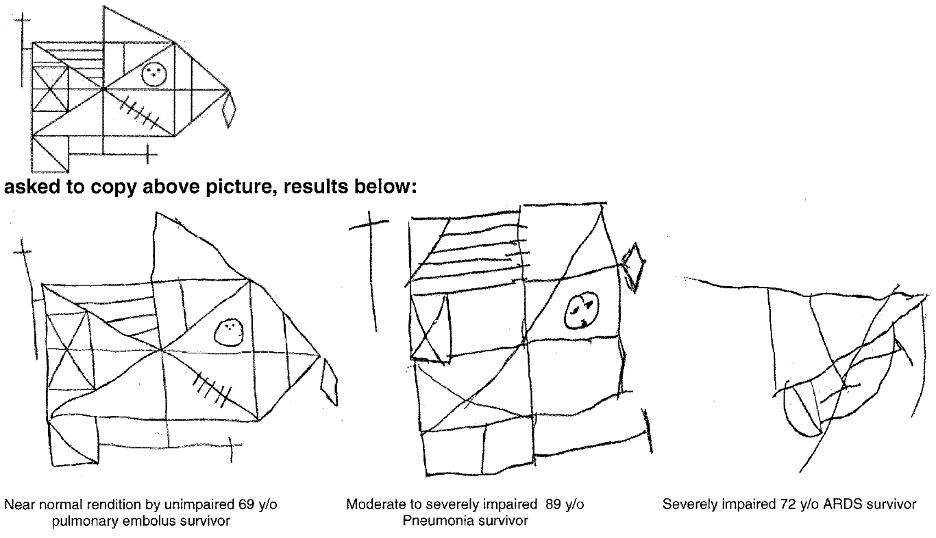
Figure 2
Rey Osterrieth Complex Figures. Six months after hospital discharge, patients were asked to copy the above figure as a test of visuo-construction. Patients shown had no detectable baseline cognitive deficits prior to critical illness. Adapted from Jackson et al. 2003.
2) Psychiatric impairment:
The most common mood disorders of PICS include anxiety (excessive irritability, worry, restlessness), depression (fatigue, loss of interest, sense of hopelessness, insomnia, poor appetite), and post-traumatic stress disorder (PTSD; flashbacks, intrusive recollection of experiences, severe anxiety and hyperarousal). These disorders can be highly disabling, leading to reduced quality of life (Mikkelsen et al. 2012; Wunsch et al. 2014; Patel et al. 2016).
3) Physical impairment:
Patients with PICS may manifest ICU-acquired weakness, ranging from generalized muscle weakness and poor mobility to quadriparesis. Complications may include falls and inability to perform activities of daily living and instrumental activities of daily living. Impairment may also be compounded by malnutrition, weight loss, or contractures due to prolonged immobility (Needham et al. 2013; Fan et al. 2014).
Manifestations of PICS across domains are often interrelated. For example, if a previously independent person is unable to perform simple activities of daily living after critical illness, this may contribute to worsened depression and anxiety.
Prevention and Treatment
Mitigating harm from sedation and delirium, and prioritizing early physical and occupational therapy are the interventions for which there is the strongest evidence. A longer duration of delirium and higher benzodiazepine dosages are independent risk factors for worsened cognitive function (Pandharipande, Girard, and Ely 2014). Interestingly, a recent study by Hayhurst and colleagues demonstrated that longer duration of hypoactive delirium in particular was independently associated with worse cognitive function at 12 months, while hyperactive delirium was not associated with long-term cognitive impairment in that cohort (Hayhurst et al. 2020).
In a prospective cohort study of over 15,000 ICU adults, the multi-pronged ABCDEF (“A2F”) bundle demonstrated a dose-response relationship - a greater percentage for eligible A2F components performed on a given day was associated with lower likelihood of numerous outcomes the next day including: death, continued mechanical ventilation, coma, delirium, physical restraint use, ICU readmission, and discharge to a facility other than home (Pun et al. 2019). This evidence, along with prior studies examining the individual components of the A2F bundle, provides strong support for its use -- in fact, few interventions in the ICU are associated with such a wide range of consistently improved outcomes.In a seminal study on early PT/OT of mechanically ventilated patients, Schweickert and colleagues randomized 104 mechanically ventilated patients to early exercise and mobilization versus standard care, and found marked improvements in return to function status at discharge (59% vs. 35%), less delirium (2 vs. 4 days) and more ventilator free days (Schweickert et al. 2009). A meta-analysis also found that protocols directed towards early mobilization were associated with shorter duration of mechanical ventilation (mean difference 2.7 fewer days) and increased ambulation at discharge (64% vs. 41%), leading to a conditional recommendation for early mobilization from the American Thoracic Society, the American College of Chest Physician, and the Society of Critical Care Medicine (Girard et al. 2017).
Other interventions have been studied with mixed effects. ICU diaries, maintained by family members and/or care providers, are intended to help patients reinforce factual memories after an ICU stay. Smaller randomized or observational studies have shown that patients and families randomized to utilize an ICU diary had reduced PTSD symptoms at three months (Jones et al. 2010) and 12 months (Garrouste-Orgeas et al. 2012). However, a recent larger randomized trial found no difference in PTSD symptoms at 3 months in patients or family members (Garrouste-Orgeas et al. 2019). Further study is needed to understand the impact of cognitive therapy delivered during or immediately after an ICU stay.
Treatment of specific impairments among ICU survivors is generally extrapolated from non-ICU populations with similar impairments (e.g. traumatic injury, dementia, depression, PTSD secondary to other etiologies). Two PICS-specific interventions have been highlighted in the field thus far – peer support groups (to help normalize patients’ symptoms, provide support necessary to facilitate recovery) and post-ICU clinics (Haines et al. 2019; McPeake et al. 2020). Further investigation is required to better characterize the impact of these interventions on patient outcomes. Multidisciplinary PICS clinics may involve critical care clinicians, pharmacists, psychologists/psychiatrists, social workers, respiratory therapists, physical and occupational therapists, and others who may help facilitate evaluation and treatment of post-ICU impairments. These exist at select sites throughout the United States and more extensively in the United Kingdom and Europe.
Lastly, it’s important to recognize that other critical care interventions - e.g. fluid management, intensive glucose control, lower oxygen targets, and neuromuscular blockade - may have unintended consequences for long term outcomes. For example, in a subset of patients from the original FACTT trial (Mikkelsen et al. 2012) who had long-term outcomes assessed, both conservative fluid management and lower arterial partial pressure of oxygen were associated with worse cognitive outcomes. Although this single finding is likely insufficient to dismiss active fluid management as harmful, it indicates the importance of incorporating assessment of long term outcomes into critical care trials of interventions focused elsewhere.
Financial Consequences
PICS is associated with decreased quality of life and inability to return to work, even as far out as a year after ICU discharge, compounding financial toxicities already associated with critical illness (Kamdar et al. 2017; Norman et al. 2016). In a recent study of ICU survivors who were part of the ROSE trial, Hauschildt and colleagues performed interviews 9-16 months post randomization to understand the financial burden that patients associated with their ARDS hospitalization (Hauschildt et al. 2020). Thirty-one of 46 survivors who participated reported at least one ARDS-related financial impact, with financial toxicity manifested via medical bills, changes in insurance coverage, and loss of employment income.
How Might Post-ICU Outcomes Differ in the Era of COVID-19?
ARDS in the setting of COVID-19 appears to require prolonged ventilation (Ziehr et al. 2020; Cummings et al. 2020) and deep sedation, which, as we have discussed, are associated with worse long-term outcomes among survivors of critical illness. Delirium has also been reported frequently. This may be in part due to the specific risk of delirium in ARDS patients and the prevalence of ARDS in the critically ill COVID-19 population. In a study of critically ill patients with respiratory failure, ARDS was independently associated with delirium, as compared with patients who were intubated for other causes of respiratory failure (Hsieh et al. 2015). Many patients with ARDS may also be treated with neuromuscular blockade, which has been associated with delayed mobility, though the most recent large trial did not demonstrate worsening of long-term outcomes as a secondary outcome (National Heart, Lung, and Blood Institute PETAL Clinical Trials Network et al. 2019). Additionally, due to visitor restrictions and infection control procedures, patients with COVID-19 and their families experience unprecedented isolation both during and following critical illness. These factors may compound the severity of PICS and PICS-F.
It will be important that providers make every effort to maintain the high-quality, patient and family-centered approach to critical care that has evolved over the past decades. This includes ensuring the components of the ABCDEF bundle are performed daily for eligible patients. Within the limits of resource availability and infection control, early mobilization with physical and occupational therapy remains one of the best established treatments to improve outcomes among survivors of mechanical ventilation (Schweickert et al. 2009). Some elements of this care can be nursing-directed (Drolet et al. 2013; Zomorodi, Topley, and McAnaw 2012). Minimization of sedation (reviewed in May 2 FLARE) and appropriate use of SAT/SBT (reviewed in May 3 FLARE) is essential. Antipsychotic medications have not been shown to improve outcomes in either hyper- or hypo-active delirium and their use should be minimized (Girard et al. 2018; Page et al. 2013). With the use of oral sedation and analgesia in the setting of medication shortages, careful attention should be paid to tapering and discontinuing these medications (e.g. oral opioids) upon transfer to the medical wards and prior to hospital discharge. In addition, many hospitals have made efforts to maintain close communication with families (joining rounds via phone, video conferencing with patients and clinicians) and minimize the isolation that patients and families experience.
Given extensive literature on joblessness and financial toxicity from critical illness, the current economy will likely serve to compound this challenge. This is particularly important when considering follow-up of ICU survivors and support services to aid in recovery.
Conclusions
Patients surviving critical illness due to COVID-19 are at high risk for PICS and other long-term consequences of critical illness. Thus far, one randomized, controlled, single-blind, single-center clinical trial has been registered at clinicaltrials.gov studying an intervention to reduce PICS specifically related to COVID-19. While more research is needed to understand the best treatments for PICS, optimizing long-term outcomes begins with high-quality ICU care, including an approach of minimizing sedation, assessing and managing pain and delirium, protocolized ventilator liberation, involving family in care through telephone and videoconferencing, and emphasizing early mobility. Post-ICU clinics and peer support are likely an important aspect of care following COVID-19 and many resources exist to guide clinicians interested in improving long-term outcomes and supporting ICU survivors. We provide a list of some of these online resources below.
Resources
- Critical Illness, Brain Dysfunction and Survivorship (CIBS) Center
- SCCM THRIVE initiative
- Critical and Acute Illness Recovery Organization
- Mayo Clinic ICU Discussion Board
- Johns Hopkins Outcomes After Critical Illness and Surgery (OACIS)
References:
- Cummings, Matthew J., Matthew R. Baldwin, Darryl Abrams, Samuel D. Jacobson, Benjamin J. Meyer, Elizabeth M. Balough, Justin G. Aaron, et al. 2020. “Epidemiology, Clinical Course, and Outcomes of Critically Ill Adults with COVID-19 in New York City: A Prospective Cohort Study.” The Lancet, May. https://doi.org/10.1016/S0140-6736(20)31189-2.
- Davidson, Judy E., Christina Jones, and O. Joseph Bienvenu. 2012. “Family Response to Critical Illness: Postintensive Care Syndrome-Family.” Critical Care Medicine 40 (2): 618–24.
- Drolet, Anne, Patti DeJuilio, Sherri Harkless, Sherry Henricks, Elizabeth Kamin, Elizabeth A. Leddy, Joanna M. Lloyd, Carissa Waters, and Sarah Williams. 2013. “Move to Improve: The Feasibility of Using an Early Mobility Protocol to Increase Ambulation in the Intensive and Intermediate Care Settings.” Physical Therapy 93 (2): 197–207.
- Fan, Eddy, David W. Dowdy, Elizabeth Colantuoni, Pedro A. Mendez-Tellez, Jonathan E. Sevransky, Carl Shanholtz, Cheryl R. Dennison Himmelfarb, et al. 2014. “Physical Complications in Acute Lung Injury Survivors: A Two-Year Longitudinal Prospective Study.” Critical Care Medicine 42 (4): 849–59.
- Garrouste-Orgeas, Maité, Isaline Coquet, Antoine Périer, Jean-François Timsit, Frédéric Pochard, Frédéric Lancrin, François Philippart, et al. 2012. “Impact of an Intensive Care Unit Diary on Psychological Distress in Patients and Relatives.” Critical Care Medicine 40 (7): 2033–40.
- Garrouste-Orgeas, Maité, Cécile Flahault, Isabelle Vinatier, Jean-Philippe Rigaud, Nathalie Thieulot-Rolin, Emmanuelle Mercier, Antoine Rouget, et al. 2019. “Effect of an ICU Diary on Posttraumatic Stress Disorder Symptoms Among Patients Receiving Mechanical Ventilation: A Randomized Clinical Trial.” JAMA: The Journal of the American Medical Association 322 (3): 229–39.
- Girard, Timothy D., Waleed Alhazzani, John P. Kress, Daniel R. Ouellette, Gregory A. Schmidt, Jonathon D. Truwit, Suzanne M. Burns, et al. 2017. “An Official American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from Mechanical Ventilation in Critically Ill Adults. Rehabilitation Protocols, Ventilator Liberation Protocols, and Cuff Leak Tests.” American Journal of Respiratory and Critical Care Medicine 195 (1): 120–33.
- Girard, Timothy D., Matthew C. Exline, Shannon S. Carson, Catherine L. Hough, Peter Rock, Michelle N. Gong, Ivor S. Douglas, et al. 2018. “Haloperidol and Ziprasidone for Treatment of Delirium in Critical Illness.” The New England Journal of Medicine 379 (26): 2506–16.
- Haines, Kimberley J., Joanne McPeake, Elizabeth Hibbert, Leanne M. Boehm, Krishna Aparanji, Rita N. Bakhru, Anthony J. Bastin, et al. 2019. “Enablers and Barriers to Implementing ICU Follow-Up Clinics and Peer Support Groups Following Critical Illness: The Thrive Collaboratives.” Critical Care Medicine 47 (9): 1194–1200.
- Hauschildt, Katrina E., Claire Seigworth, Lee A. Kamphuis, Catherine L. Hough, Marc Moss, Joanne M. McPeake, Theodore J. Iwashyna, and National Heart, Lung, and Blood Institute (NHLBI) Prevention and Early Treatment of Acute Lung Injury (PETAL) Network. 2020. “Financial Toxicity After Acute Respiratory Distress Syndrome: A National Qualitative Cohort Study.” Critical Care Medicine, May. https://doi.org/10.1097/CCM.0000000000004378.
- Hayhurst, Christina J., Annachiara Marra, Jin H. Han, Mayur B. Patel, Nathan E. Brummel, Jennifer L. Thompson, James C. Jackson, et al. 2020. “Association of Hypoactive and Hyperactive Delirium With Cognitive Function After Critical Illness.” Critical Care Medicine, April. https://doi.org/10.1097/CCM.0000000000004313.
- Hsieh, S. Jean, Graciela J. Soto, Aluko A. Hope, Ana Ponea, and Michelle N. Gong. 2015. “The Association between Acute Respiratory Distress Syndrome, Delirium, and in-Hospital Mortality in Intensive Care Unit Patients.” American Journal of Respiratory and Critical Care Medicine 191 (1): 71–78.
- Jackson, James C., Robert P. Hart, Sharon M. Gordon, Ayumi Shintani, Brenda Truman, Lisa May, and E. Wesley Ely. 2003. “Six-Month Neuropsychological Outcome of Medical Intensive Care Unit Patients.” Critical Care Medicine 31 (4): 1226–34.
- Jones, Christina, Carl Bäckman, Maurizia Capuzzo, Ingrid Egerod, Hans Flaatten, Cristina Granja, Christian Rylander, Richard D. Griffiths, and RACHEL group. 2010. “Intensive Care Diaries Reduce New Onset Post Traumatic Stress Disorder Following Critical Illness: A Randomised, Controlled Trial.” Critical Care / the Society of Critical Care Medicine 14 (5): R168.
- Kamdar, Biren B., Minxuan Huang, Victor D. Dinglas, Elizabeth Colantuoni, Till M. von Wachter, Ramona O. Hopkins, Dale M. Needham, and National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. 2017. “Joblessness and Lost Earnings after Acute Respiratory Distress Syndrome in a 1-Year National Multicenter Study.” American Journal of Respiratory and Critical Care Medicine 196 (8): 1012–20.
- Maley, Jason H., Isabel Brewster, Iris Mayoral, Renata Siruckova, Sarah Adams, Kelley A. McGraw, Angela A. Piech, Michael Detsky, and Mark E. Mikkelsen. 2016. “Resilience in Survivors of Critical Illness in the Context of the Survivors’ Experience and Recovery.” Annals of the American Thoracic Society 13 (8): 1351–60.
- Marra, Annachiara, Pratik P. Pandharipande, Timothy D. Girard, Mayur B. Patel, Christopher G. Hughes, James C. Jackson, Jennifer L. Thompson, Rameela Chandrasekhar, Eugene Wesley Ely, and Nathan E. Brummel. 2018. “Co-Occurrence of Post-Intensive Care Syndrome Problems Among 406 Survivors of Critical Illness.” Critical Care Medicine 46 (9): 1393–1401.
- McPeake, Joanne, Leanne M. Boehm, Elizabeth Hibbert, Rita N. Bakhru, Anthony J. Bastin, Brad W. Butcher, Tammy L. Eaton, et al. 2020. “Key Components of ICU Recovery Programs: What Did Patients Report Provided Benefit?” Critical Care Explorations 2 (4): e0088.
- Mikkelsen, Mark E., Jason D. Christie, Paul N. Lanken, Rosette C. Biester, B. Taylor Thompson, Scarlett L. Bellamy, A. Russell Localio, Ejigayehu Demissie, Ramona O. Hopkins, and Derek C. Angus. 2012. “The Adult Respiratory Distress Syndrome Cognitive Outcomes Study: Long-Term Neuropsychological Function in Survivors of Acute Lung Injury.” American Journal of Respiratory and Critical Care Medicine 185 (12): 1307–15.
- Nasreddine, Ziad S., Natalie A. Phillips, Valérie Bédirian, Simon Charbonneau, Victor Whitehead, Isabelle Collin, Jeffrey L. Cummings, and Howard Chertkow. 2005. “The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment.” Journal of the American Geriatrics Society 53 (4): 695–99.
- National Heart, Lung, and Blood Institute PETAL Clinical Trials Network, Marc Moss, David T. Huang, Roy G. Brower, Niall D. Ferguson, Adit A. Ginde, M. N. Gong, et al. 2019. “Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome.” The New England Journal of Medicine 380 (21): 1997–2008.
- Needham, Dale M., Judy Davidson, Henry Cohen, Ramona O. Hopkins, Craig Weinert, Hannah Wunsch, Christine Zawistowski, et al. 2012. “Improving Long-Term Outcomes after Discharge from Intensive Care Unit: Report from a Stakeholders’ Conference.” Critical Care Medicine 40 (2): 502–9.
- Needham, Dale M., Victor D. Dinglas, Peter E. Morris, James C. Jackson, Catherine L. Hough, Pedro A. Mendez-Tellez, Amy W. Wozniak, et al. 2013. “Physical and Cognitive Performance of Patients with Acute Lung Injury 1 Year after Initial Trophic versus Full Enteral Feeding. EDEN Trial Follow-Up.” American Journal of Respiratory and Critical Care Medicine 188 (5): 567–76.
- Norman, Brett C., James C. Jackson, John A. Graves, Timothy D. Girard, Pratik P. Pandharipande, Nathan E. Brummel, Li Wang, Jennifer L. Thompson, Rameela Chandrasekhar, and E. Wesley Ely. 2016. “Employment Outcomes After Critical Illness: An Analysis of the Bringing to Light the Risk Factors and Incidence of Neuropsychological Dysfunction in ICU Survivors Cohort.” Critical Care Medicine 44 (11): 2003–9.
- Page, Valerie J., E. Wesley Ely, Simon Gates, Xiao Bei Zhao, Timothy Alce, Ayumi Shintani, Jim Jackson, Gavin D. Perkins, and Daniel F. McAuley. 2013. “Effect of Intravenous Haloperidol on the Duration of Delirium and Coma in Critically Ill Patients (Hope-ICU): A Randomised, Double-Blind, Placebo-Controlled Trial.” The Lancet. Respiratory Medicine 1 (7): 515–23.
- Pandharipande, Pratik P., Timothy D. Girard, and E. Wesley Ely. 2014. “Long-Term Cognitive Impairment after Critical Illness.” The New England Journal of Medicine.
- Patel, Mayur B., James C. Jackson, Alessandro Morandi, Timothy D. Girard, Christopher G. Hughes, Jennifer L. Thompson, Amy L. Kiehl, et al. 2016. “Incidence and Risk Factors for Intensive Care Unit-Related Post-Traumatic Stress Disorder in Veterans and Civilians.” American Journal of Respiratory and Critical Care Medicine 193 (12): 1373–81.
- Pun, Brenda T., Michele C. Balas, Mary Ann Barnes-Daly, Jennifer L. Thompson, J. Matthew Aldrich, Juliana Barr, Diane Byrum, et al. 2019. “Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15,000 Adults.” Critical Care Medicine 47 (1): 3–14.
- Schweickert, William D., Mark C. Pohlman, Anne S. Pohlman, Celerina Nigos, Amy J. Pawlik, Cheryl L. Esbrook, Linda Spears, et al. 2009. “Early Physical and Occupational Therapy in Mechanically Ventilated, Critically Ill Patients: A Randomised Controlled Trial.” The Lancet 373 (9678): 1874–82.
- Wunsch, Hannah, Christian F. Christiansen, Martin B. Johansen, Morten Olsen, Naeem Ali, Derek C. Angus, and Henrik Toft Sørensen. 2014. “Psychiatric Diagnoses and Psychoactive Medication Use among Nonsurgical Critically Ill Patients Receiving Mechanical Ventilation.” JAMA: The Journal of the American Medical Association 311 (11): 1133–42.
- Ziehr, David R., Jehan Alladina, Camille R. Petri, Jason H. Maley, Ari Moskowitz, Benjamin D. Medoff, Kathryn A. Hibbert, B. Taylor Thompson, and C. Corey Hardin. 2020. “Respiratory Pathophysiology of Mechanically Ventilated Patients with COVID-19: A Cohort Study.” American Journal of Respiratory and Critical Care Medicine, April. https://doi.org/10.1164/rccm.202004-1163LE.
- Zomorodi, Meg, Darla Topley, and Maire McAnaw. 2012. “Developing a Mobility Protocol for Early Mobilization of Patients in a Surgical/trauma ICU.” Critical Care Research and Practice 2012 (December): 964547.
View all COVID-19 Updates
Learn more about research in the Division of Pulmonary and Critical Care Medicine