Multiparametric MRI For Prostate Cancer
In This Article
- PSA screening for prostate cancer has led to the detection of a greater number of smaller, clinically insignificant cancers and, consequently, to overtreatment
- Use of multiparametric MRI to triage men with suspected prostate cancer could help guide biopsy for clinically insignificant cancers and increase confidence in ruling out men with clinically insignificant tumors
- A recent study suggests that multiparametric MRI can help with local staging of prostate cancer, improving treatment and prognosis in cancer patients
Prostate cancer is the second most common cause of cancer death in men, after lung cancer. Because of the aging population, its incidence is expected to approximately double by 2030. Tests for the biomarker prostate-specific antigen (PSA) are widely used for screening and diagnosis of prostate cancer, but there is still considerable debate about the extent to which these tests should inform decisions about performing biopsies in men with elevated levels of PSA, or even be used at all.
Subscribe to the latest updates from Radiology Advances in Motion
Much of this debate centers around the question of whether or not the cancers detected by PSA tests are clinically significant. Studies have linked the use of PSA screening to underdetection of clinically significant cancers and overdetection of clinically insignificant ones, leading to a greater number of unnecessary biopsies and tilting the risk-benefit analysis associated with screening. In recent years, researchers have been exploring ways to mitigate the additional risks by using multiparametric magnetic resonance imaging, in part by adding a "rule in/out" step after screening to help avoid biopsy in cases with positive PSA tests. Studies have shown this approach to be effective both in reducing the number of unnecessary biopsies and in targeting suspicious areas during biopsy.
The Downside of Detecting More Prostate Cancers with PSA Screening
Though prostate cancer is one of the leading causes of cancer death in men, most men diagnosed with prostate cancer do not die from it. According to the American Cancer Society, approximately one in nine men will be diagnosed with the disease in their lifetimes, but only about one in 41 will succumb to it. This disparity exists because smaller cancers are unlikely to progress far enough during the patients’ lifetimes to prove fatal. These cancers are considered clinically insignificant. However, clinically significant cancers are associated with a high probability of death within 10 years after diagnosis. Whether a cancer is considered clinically significant or insignificant is based on its Gleason score, the sum of a primary and a secondary grade assigned to the cancer by a pathologist.
Studies have shown men with clinically insignificant prostate cancers do not benefit from treatment. Still, many of these men end up receiving treatment as many clinicians, not wanting to miss any cancers, will err on the side of caution. This overtreatment has grown even more acute with increasing use of PSA screening. As a result, more men undergo biopsy, leading to anxiety and possible detrimental effects of further interventions. Other patients are placed in active surveillance programs after detection of clinically insignificant cancers with regular assessments over time, which involve risks for the patients and additional costs for the health care system. Clinicians now face the challenge of figuring out how to detach the likelihood of overtreatment from the higher rates of diagnosis that accompany PSA screening. In other words, how do providers achieve the optimal balance of benefits and risks?
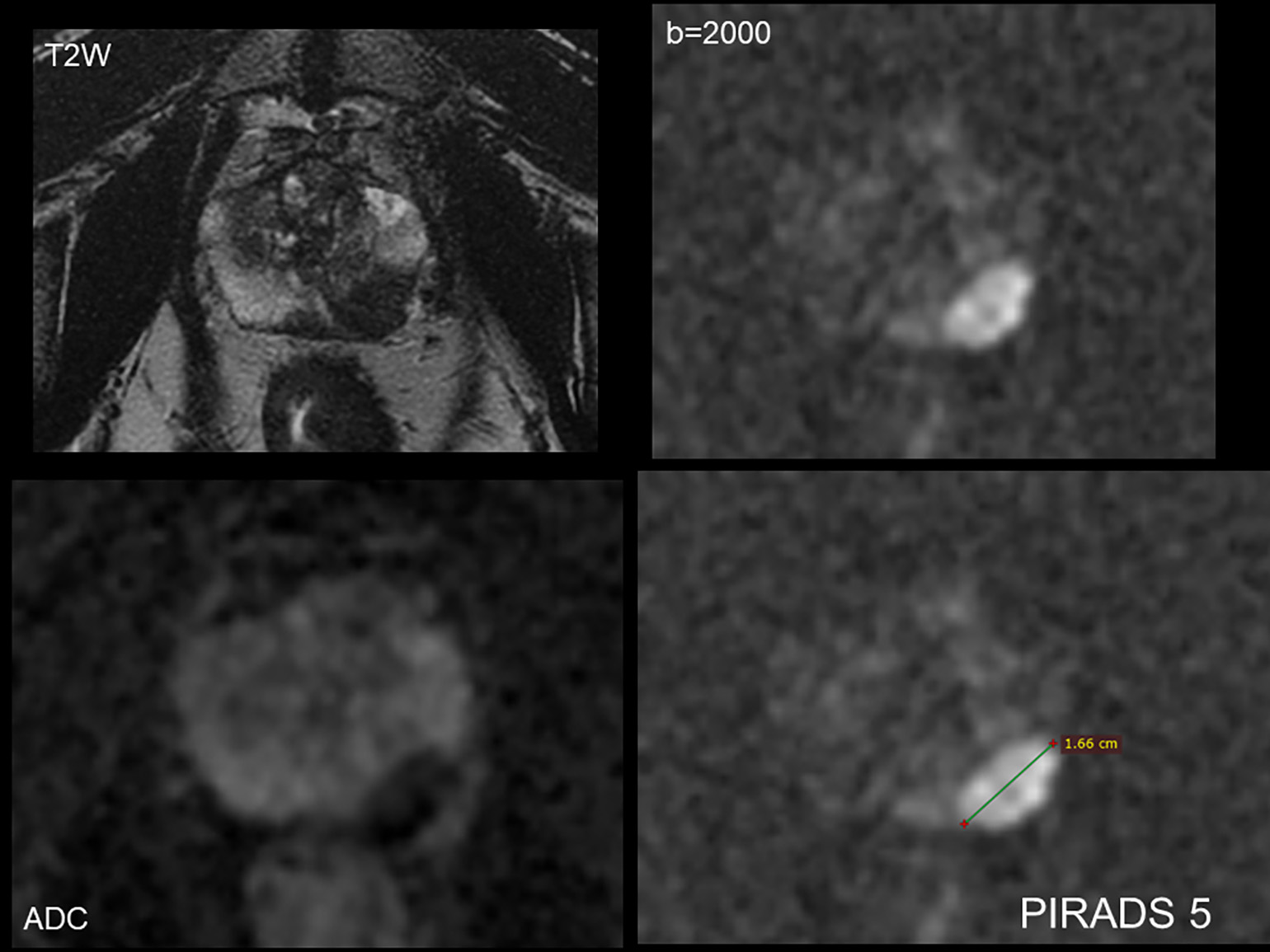
Figure 1
These images of the prostate shows a left mid-peripheral zone lesion with a high likelihood of diagnosis of cancer (PI-RADS 5). The lesion appears dark on T2-weighted MRI, showing restricted diffusion and measuring 1.6 cm.
Using Multiparametric MRI to Diagnose Clinically Significant Prostate Cancers
Multiparametric MRI, a technique that combines standard anatomical MRI with functional imaging such as dynamic contrast-enhanced (DCE) MRI or diffusion-weighted imaging (DWI), offers an alternative diagnostic pathway to help improve the risk-benefit analysis for men with clinical suspicion of prostate cancer. In current practice, men with PSA readings above a given threshold (often 4.0 ng per ml) typically undergo transrectal ultrasound-guided biopsy to determine whether the readings show clinically significant or clinically insignificant cancers. Ideally, men in the latter group would not have to undergo the procedure. Multiparametric MRI could move clinicians closer to this goal. Over the past decade, the technique has emerged as a possible means of triage before biopsy by detecting clinically significant cancer or ruling it out, avoiding biopsy and its attendant risks.
In cases with positive findings, multiparametric MRI can also be used to target the suspicious areas during biopsy. In a study reported in 2018 in The New England Journal of Medicine, a team of investigators sought to determine the efficacy of MRI-targeted biopsy, particularly as compared to ultrasound-guided biopsy. The multicenter, randomized trial followed 500 participants, 252 of whom were assigned to an MRI-targeted biopsy group and 248 of whom were assigned to a standard ultrasound-guided biopsy group. The researchers found that MRI was noninferior and, in fact, generally superior to the ultrasound-guided approach. It detected more clinically significant cancers and fewer clinically insignificant ones and, in cases of biopsy, fewer biopsy cores were obtained. Multiparametric MRI also helped more men in the trial avoid biopsy altogether.
The question isn't yet settled. Following a 2017 study published in Lancet showing that 10-15% of clinically significant cancers could be missed with MRI-targeted biopsies alone, some clinicians believe that MRI-guided biopsies should be performed in conjunction with ultrasound-guided ones of areas that look normal on MRI. However, this approach would increase, rather than decrease, the number of clinically insignificant cancers found.
In any event, multiparametric MRI isn’t yet ready for widespread clinical implementation. Especially given the costs of operating MRI, more work needs to be done to validate the findings of the New England Journal of Medicine study. Still, the findings underscore a possible role for multiparametric MRI in reducing the number of clinically insignificant prostate cancers detected, thus improving the risk-benefit analysis associated with PSA screening.
Staging Prostate Cancer with MR Imaging of Extraprostatic Extension of Cancer Cells
Other work in recent years points to the use for multiparametric MRI in local staging for prostate cancer. Research has shown that local extraprostatic extension (EPE) of cancer cells is an important indicator in determining the prognosis of men with prostate cancer and that multiparametric MRI offers a robust means of imaging EPE. Until earlier this year, though, no one had proposed a systematic approach to staging prostate cancer using MRI.
In Radiology in March 2019, a team of investigators described a grading system based on imaging assessment of three features of EPE: large capsular contact, capsular bulge and gross EPE. Using multiparametric imaging in a cohort of 553 patients, they showed the system can predict pathologic EPE, with higher grading categories corresponding with a greater risk of EPE. With further validation, the system could be applied to treatment and prognosis of men with prostate cancer.
References
- Barry MJ. (2018). Screening for Prostate Cancer: Is the Third Trial the Charm? JAMA 319(9): 868-869.
- Eberhardt SC. (2019). Local Staging of Prostate Cancer with MRI: A Need for Standardization. Radiology 290(3): 720-721.
- Kasivisvanathan V, Rannikko AS, Borghi M, et al. (2018). MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N Engl J Med 378(19): 1767-1777.
Visit Mass General Imaging
Refer a patient to the Department of Urology