New ICU Data from Italy
The FLARE Four
- To date, most published data on critical illness in association with COVID-19 consist of uncontrolled case series with relatively small numbers
- Grasselli et al. have reported the experience of 1591 ICU patients with COVID-19 in the Lombardy region of Italy
- Median P:F was 160 mmHg in this cohort. Little data on respiratory mechanics is provided but median PEEP was 14 cmH2O. The ICU population, therefore, consisted mostly of mild-to-moderate ARDS by Berlin criteria and was broadly similar to prior ARDS observational cohorts such as LUNG-SAFE
- Follow-up was limited in the Italian study, but ICU mortality to date is reported as 26%. The majority of patients described (58%), however, were still in the ICU at the end of the follow-up period
Subscribe to the latest updates from FLARE Advances in Motion
Many people are saying....few critically ill patients with COVID-19 survive.
Earlier this week, Grasselli et al. published data on the largest ICU cohort of patients with COVID-19 to date (Grasselli et al., 2020).
What are the highlights of this manuscript? How does it add to our current understanding of critical illness from COVID-19?
Basic Summary of the Paper
Research Plan
Research question:
What are the characteristics and outcomes of COVID-19 patients admitted to ICUs in the Lombardy region of Italy?
Design:
Retrospective observational study of 1591 patients with SARS-CoV-2 identified on PCR admitted to any of the 72 ICUs in the COVID-19 Lombardy ICU Network.
Study period:
February 20-March 18, 2020. Follow-up through March 25, 2020.
Results
Patient Characteristics:
- 82% male, gender distribution similar across all age groups
- Median age 63 (IQR 56-70, range 14-91)
- 68% of patients with 1 or more comorbidities: 49% with HTN, 21% CVD, 18% HLD, 4% COPD
Respiratory Support Data During the First 24 Hours:
- 88% received mechanical ventilation (MV) within 24 hours of admission to ICU. There was no difference in rate of MV by age
During the First 24 Hours:
- Median PEEP: 14 cmH2O (IQR 12-16), maximum of 22 cmH2O
- Median FiO2: 89% required FiO2 50% or greater; higher in older patients
- Median PaO2/FiO2: 160 (IQR 114-220); higher in younger patients
- At ICU admission, 27% (240/875) were placed in prone position
- At ICU admission, 1% (5/498) were treated with ECMO
Outcomes:
- ICU mortality rate: 26%; significantly lower in patients < 64 years (15% vs 36%, p < 0.001)
- Median ICU LOS: 9 days (IQR 6-13)
Associations:
- The authors spend a substantial portion of their analysis evaluating for associations between hypertension (the most common comorbidity in this cohort) and outcomes. There were no apparent differences in respiratory parameters for patients with hypertension, although of the patients who died, more had hypertension than those who were discharged from the ICU (63% vs 40%, p < 0.001). These findings should be interpreted with caution since 58% of patients were still in the ICU at the time of reporting.
Criticisms
- Substantial amounts of missing data (missing respiratory support data from nearly 300 (20%) patients)
- No data included about clinical presentation or laboratory values
- Minimal data included about respiratory mechanics
- No information included about adjunctive therapies, such as neuromuscular blockade, vasopressor use, renal replacement therapy or therapies directed towards SARS-CoV-2 (such as antivirals)
- 58% of patients were still in ICU at the time of report
- Limited follow-up period
What Does This Study Add?
This is by far the largest published study of critically-ill patients with COVID-19. Given the large numbers of patients, these data inform our understanding of critically-ill COVID-19 patients in two ways. First, we see the characteristics of the critically ill COVID-19 patients in this cohort: they often require invasive mechanical ventilation, with high levels of PEEP, and high levels of FiO2. Second, we begin to note the probability of survival in this patient population, although mortality remains unknown because over 50% of the patients remain in the ICU at the time of the report.
Though criteria for ARDS were not addressed in this paper, a median P/F ratio of 160 would be consistent with moderate ARDS (assuming other Berlin criteria were met) (ARDS Definition Task Force et al., 2012).
How Does This Compare to Other ICU Cohorts?
Below is a table summarizing the major peer-reviewed publications of critically ill COVID-19 patients thus far. Importantly, there is variation in which ICU treatments are reported. Across these studies, there is a wide range of ICU mortality, use of mechanical ventilation, vasopressors and renal replacement therapy. Use of extracorporeal membrane oxygenation is generally rare.
Major published reports of cohorts of ICU COVID-19 patients are summarized here:
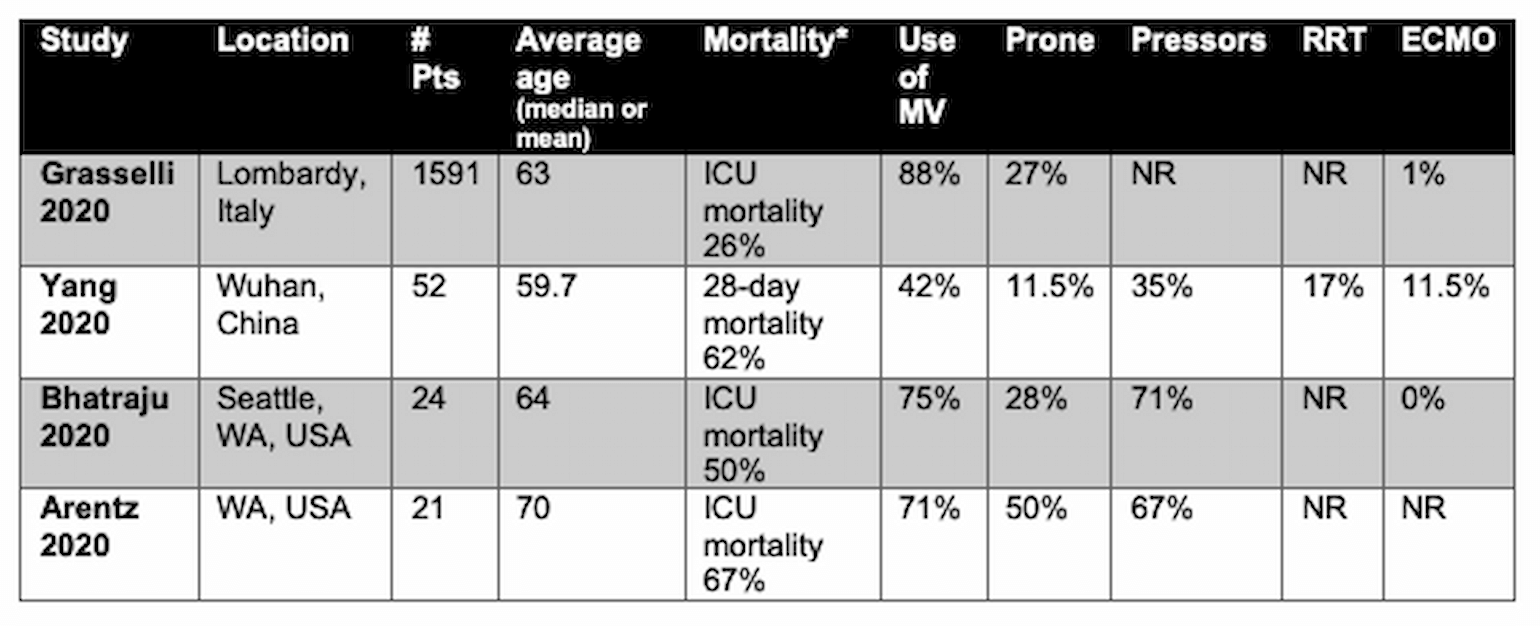
Table 1
*rates of ICU mortality may change with follow-up. IMV = invasive mechanical ventilation, , RRT = renal replacement therapy, ECMO = extracorporeal membrane oxygenation, NR = not reported.
Commentary
This large cohort is characterized by respiratory failure with mild-to-moderate impairment in gas exchange. Despite speculation elsewhere about the unique attributes of patients with COVID-19 associated respiratory failure, the patients described here are broadly similar to the largest observation cohort of ARDS in the pre-COVID-19 era, LUNG-SAFE (Bellani et al., 2016). The Large Observational Study to Understand the Global Impact of Severe Acute Respiratory Failure (LUNG-SAFE) was an international, multicenter study of 3,022 patients with ARDS from 459 ICUs across 50 countries. This study is often referenced to understand the epidemiology, respiratory characteristics, and worldwide outcomes of contemporary patients with ARDS. In this cohort, the mean age was 61 (compared to 63 in the Italian study). The types of comorbidities (cardiac disease, lung disease, diabetes) were similar to Grasseli et al., as were the respiratory parameters: the median PaO2/FiO2 of the entire cohort was 161 mmHg and mean FiO2 was 0.65. A graphical comparison of the reported respiratory parameters reported by Grasseli et al. and LUNG-SAFE is shown below.
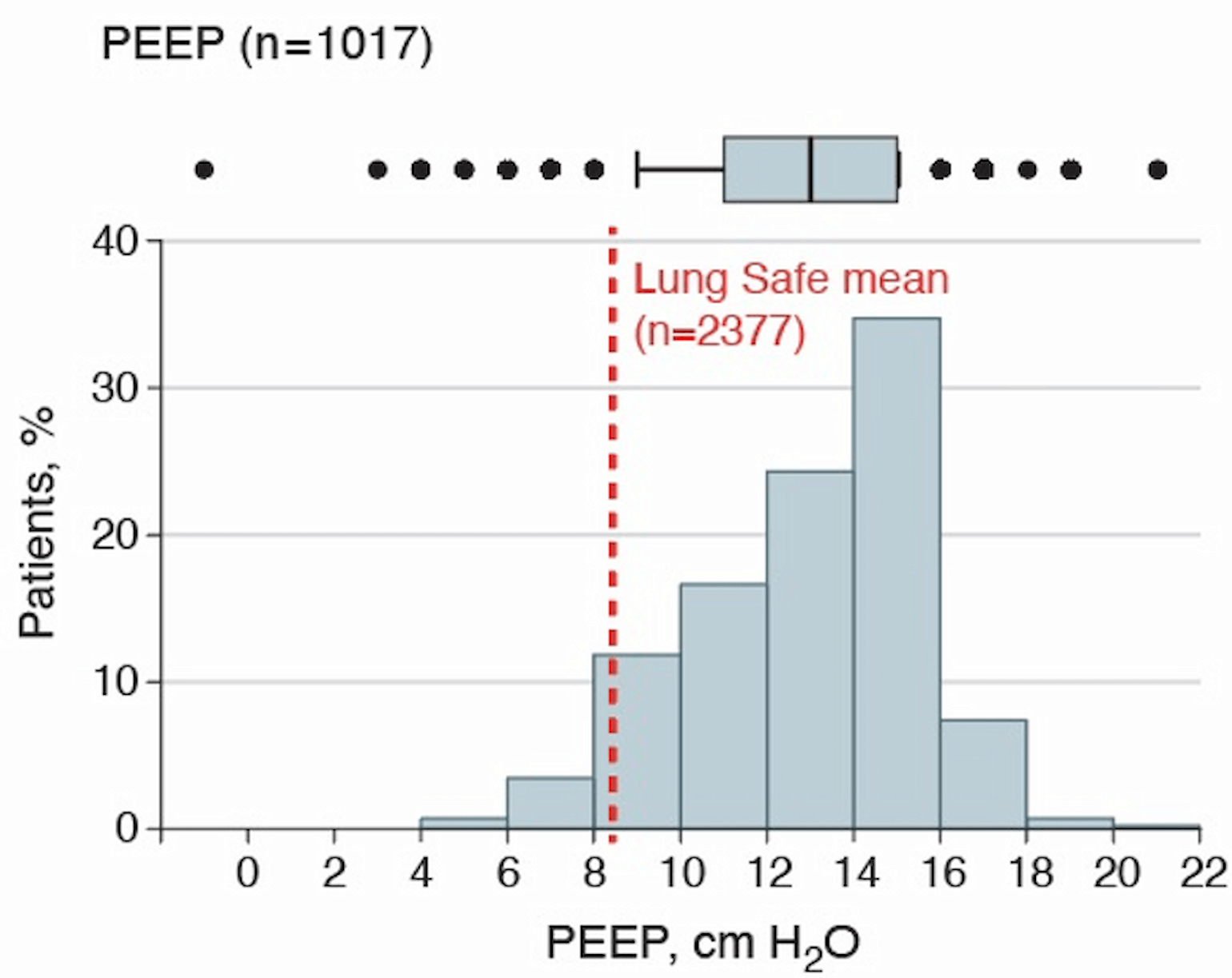
Figure 1
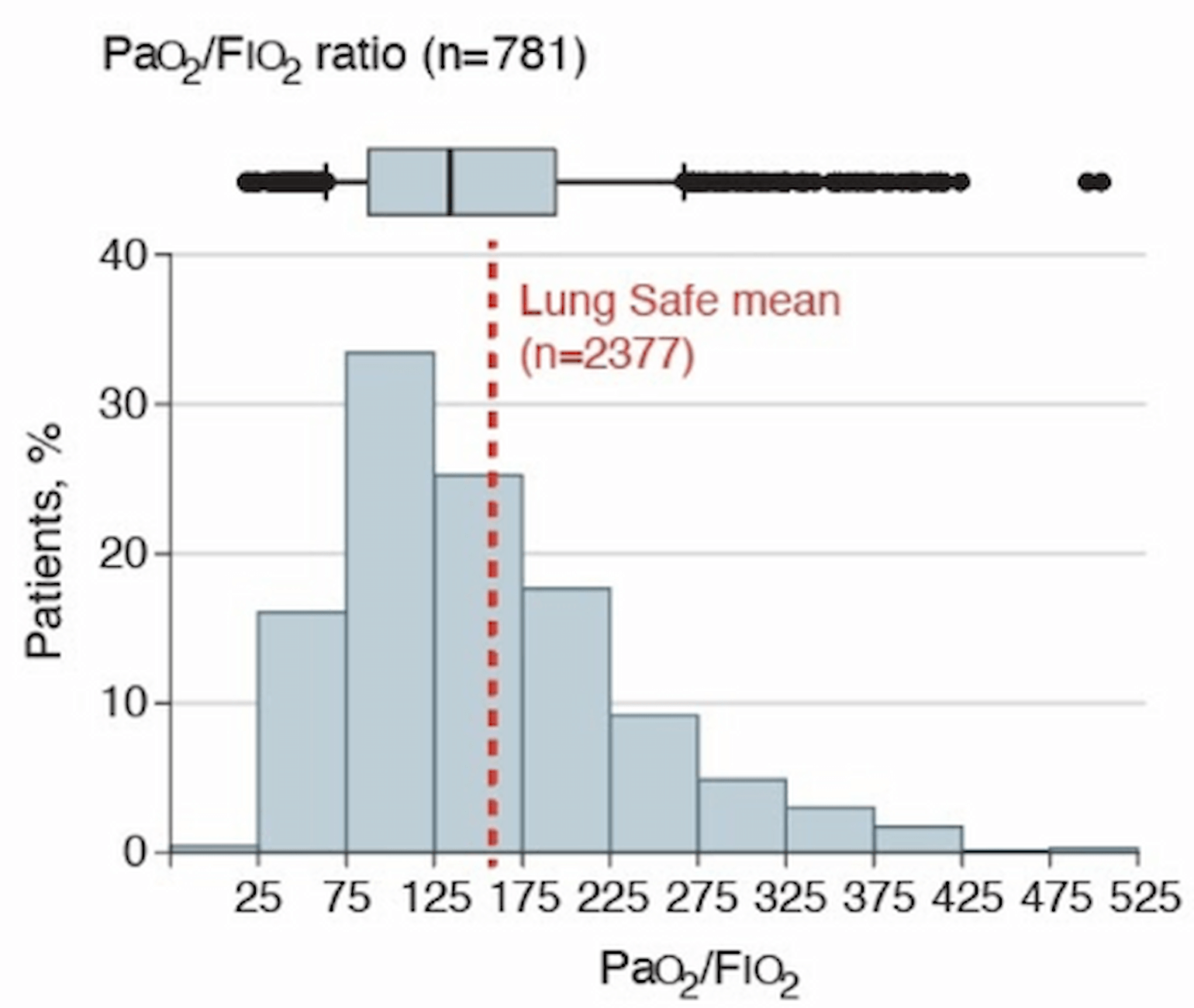
Figure 2
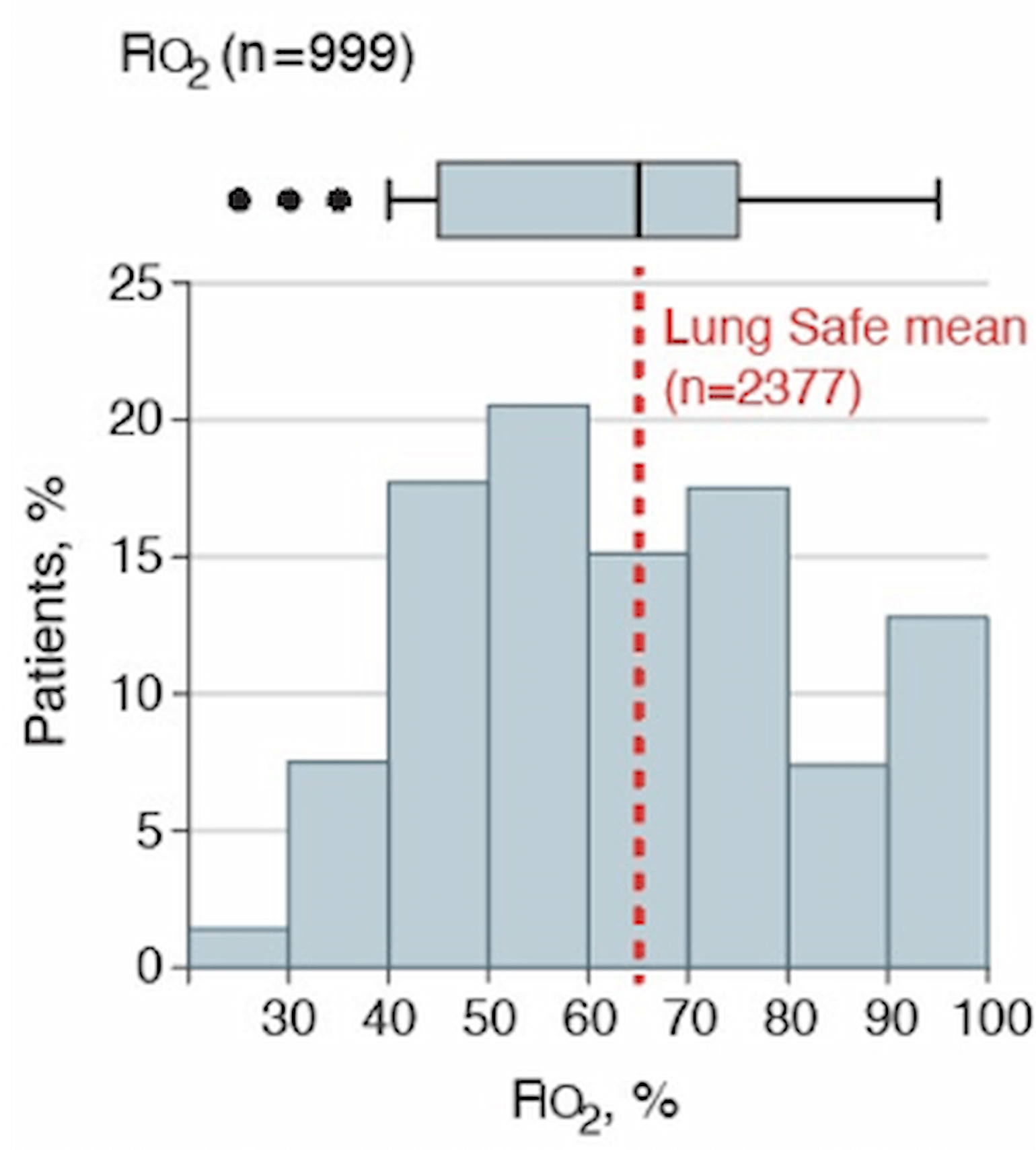
Figure 3
Figures 1-3:
Framing Lombardy ICU experience data with respect to LUNG-SAFE data. The panels show PaO2:FiO2, FiO2 and PEEP values across the Lombardy cohort. Means from the LUNG-SAFE cohort for comparison are superimposed over this data and indicated at the red dotted line (PaO2:FiO2 161, FiO2 0.65, PEEP 8.4 cm H2O).
Based on the similarities outlined above, we expect comparable outcomes in the cohort described by Grasseli et al., once sufficient time for follow-up has passed. Furthermore, overall mortality in LUNG-SAFE was 34.9%, and 28-day mortality in a previously published series of ICU patients from China was 28%. On this basis we may reasonably expect that the majority of critically ill patients with COVID-19 will survive.
References
- ARDS Definition Task Force, Ranieri, V.M., Rubenfeld, G.D., Thompson, B.T., Ferguson, N.D., Caldwell, E., Fan, E., Camporota, L., and Slutsky, A.S. (2012). Acute respiratory distress syndrome: the Berlin Definition. JAMA 307, 2526–2533.
- Arentz, M., Yim, E., Klaff, L., Lokhandwala, S., Riedo, F.X., Chong, M., and Lee, M. (2020). Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA.
- Bellani, G., Laffey, J.G., Pham, T., Fan, E., Brochard, L., Esteban, A., Gattinoni, L., van Haren, F., Larsson, A., McAuley, D.F., et al. (2016). Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 315, 788–800.
- Bhatraju, P.K., Ghassemieh, B.J., Nichols, M., Kim, R., Jerome, K.R., Nalla, A.K., Greninger, A.L., Pipavath, S., Wurfel, M.M., Evans, L., et al. (2020). Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N. Engl. J. Med.
- Grasselli, G., Pesenti, A., and Cecconi, M. (2020). Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA.
- Yang, X., Yu, Y., Xu, J., Shu, H., Xia, J. ’an, Liu, H., Wu, Y., Zhang, L., Yu, Z., Fang, M., et al. (2020). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med.
View all COVID-19 updates
Learn about research in the Division of Pulmonary and Critical Care Medicine