Vocal Cord Paralysis Commonly Asymptomatic in Patients With Recurrent Laryngeal Nerve Invasion by Thyroid Cancer
Key findings
- This study examined clinical characteristics, surgical management and outcomes of 65 patients who had recurrent laryngeal nerves (RLNs) invaded by a primary thyroid tumor or its nodal metastasis and underwent nerve-monitored surgery
- Preoperative voice complaints were reported by only 24 (39%) of the 61 patients who had data available, but vocal cord paralysis (VCP) was documented in 27 (44%) of the 62 patients who underwent preoperative laryngoscopy
- Radioactive iodine therapy was the only statistically significant factor associated with improved five-year recurrence-free survival (P=0.006) or overall survival (P= 0.004), regardless of RLN resection status
- Preoperative laryngoscopy is especially important for patients undergoing thyroidectomy who have suspected RLN invasion; otherwise, surgeons may miss the true functional status of the vocal cords
The recurrent laryngeal nerve (RLN) is one of the structures most commonly invaded by thyroid carcinoma. RLN invasion is strongly associated with malignancy and higher recurrence rates, and its detection affects surgical decision-making.
Subscribe to the latest updates from Otolaryngology Advances in Motion
Gregory W. Randolph, MD, FACS, FACE, director of the Thyroid and Parathyroid Endocrine Surgery Division at Mass Eye and Ear, and colleagues recently completed one of the largest single-center studies of nerve-monitored surgery devoted exclusively to RLNs invaded by a primary thyroid tumor or its nodal metastasis.
Along with other specifics about postoperative outcomes, they report in The Laryngoscope that five-year survival was unrelated to whether the invaded RLN was resected or the tumor was completely resected from the RLN.
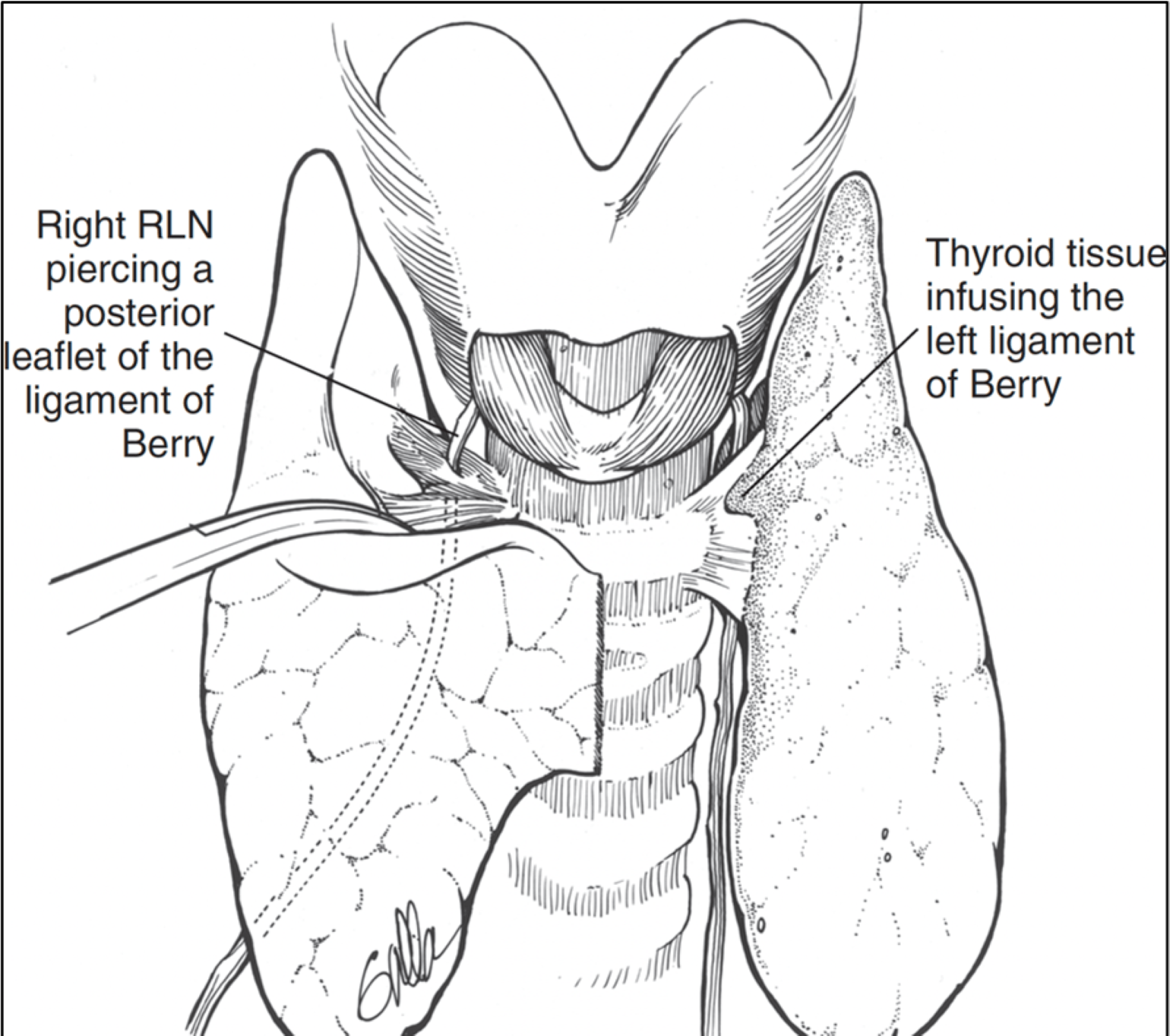
Figure 1
Anterior view of the thyroid and airway, showing how close the thyroid tissue comes to the recurrent laryngeal nerve (RLN). With invasive thyroid cancer, the lesion may therefore invade the RLN.
Methods
The researchers identified 65 patients with RLN invasion by thyroid carcinoma (59%), nodal metastases (31%) or both (10%) who were operated on between December 1995 and December 2015. RLN invasion was documented on the right side in 55% of patients, on the left in 43%, and bilaterally in 1.5%.
63% of patients were female, the mean age was 56 years, and two patients (5%) reported prior head and neck radiation.
Surgical Management
37% of patients underwent total thyroidectomy, 43% hemithyroidectomy, and 20% revision surgery. 95% underwent central nerve dissection and 55% lateral nerve dissection as part of the surgery. Invaded RLNs were resected in 74% of patients.
Preoperative Voice Symptoms and VCP
Preoperative voice complaints were reported by only 24 (39%) of the 61 patients who had data available. Vocal cord paralysis (VCP) was documented in 27 (44%) of the 62 patients who underwent preoperative laryngoscopy.
Postoperative Voice Outcome
Fifty-five patients underwent postoperative laryngoscopy, and 45 of those patients (82%) had persistent VCP at six months. There was no significant difference in the frequency of postoperative VCP according to whether an RLN was invaded by a primary tumor or nodal metastases.
Metastasis and Outcomes
Over mean follow-up of 66 months, distant metastasis was documented in 36% of patients and locoregional recurrence in another 36%.
Radioactive iodine therapy was the only factor significantly associated with improved five-year recurrence-free survival (P=0.006) or overall survival (P= 0.004). Age (greater or less than 55), gender, use of adjuvant radiotherapy, and RLN resection status did not affect survival.
Guidance for Surgeons
Other data suggested RLN invasion may be a gradual process and some neural function is maintained throughout long periods of the invasive process. Taken together, the results emphasize the importance of preoperative laryngoscopy in patients undergoing thyroidectomy in general and especially in patients with suspected RLN invasion.
Without a direct laryngeal examination, surgeons may miss the true functional status of the vocal cords because RLN invasion has not affected vocal cord function preoperatively.
The lack of significant neural invasion on five-year recurrence-free survival or overall survival strongly suggests the current thyroid TNM staging should be revised so that RLN invasion is changed from a T4a designation to T3b, which deescalates staging from Stage III to Stage II.
view original journal article Subscription may be required
Learn more about the Department of Otolaryngology–Head and Neck Surgery at Mass Eye and Ear
Refer a patient to Mass Eye and Ear/Mass General Brigham