The Toth Center: New Leadership, Novel Innovations
In This Article
- Conventionally, a tumor is visible after a CT or MRI is performed, but the physician cannot see this in real-time as they are operating to remove tumors. There is an urgent need to see the exact margin of a tumor when patients are open in surgery
- In the Kumar lab, the novel FLT imaging technique demonstrated 97% accuracy in distinguishing tumor tissue from healthy tissue in clinical patient trials performed at Mass Eye and Ear and collaborating hospitals
- Anand Kumar, PhD, director of the Toth Center at Mass Eye and Ear, received a R01 grant from the NIH to further develop and test an imaging device based on their technology to help surgeons visualize tumors better during surgery
- The Shalhout lab in the Toth Center focuses on using artificial intelligence (AI) to develop more effective therapies, enhance the understanding of tumor biology, and improve how physicians diagnose, treat, and manage cancer
- The Faden lab in the Toth Center concentrates on the development and use of liquid biopsies to detect human papillomavirus (HPV)-associated head and neck cancers
This article was written by Nicole Feldman and republished from the Spring 2024 Harvard Otolaryngology Magazine.
Subscribe to the latest updates from Otolaryngology Advances in Motion
The Mike Toth Head and Neck Cancer Research Center—named in memory of Mike Toth, a patient and friend of Mass Eye and Ear who courageously fought head and neck cancer but sadly succumbed to the disease—has been integral in pioneering innovative approaches to diagnosing, monitoring and treating cancers of the head, neck, and skin since 2019.
Under the new leadership of Anand T. N. Kumar, PhD, director of the Toth Center and associate professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School, the team continues to leverage the brightest minds to challenge current treatments and improve future outcomes for patients with these diseases.
"The Toth Center is composed of an extraordinary group of interdisciplinary investigators, all with the same goal to eradicate head and neck cancer," shared Dr. Kumar. "We have a lot of areas to continue to explore, and as the new director, I look forward to building and growing a collaborative center."
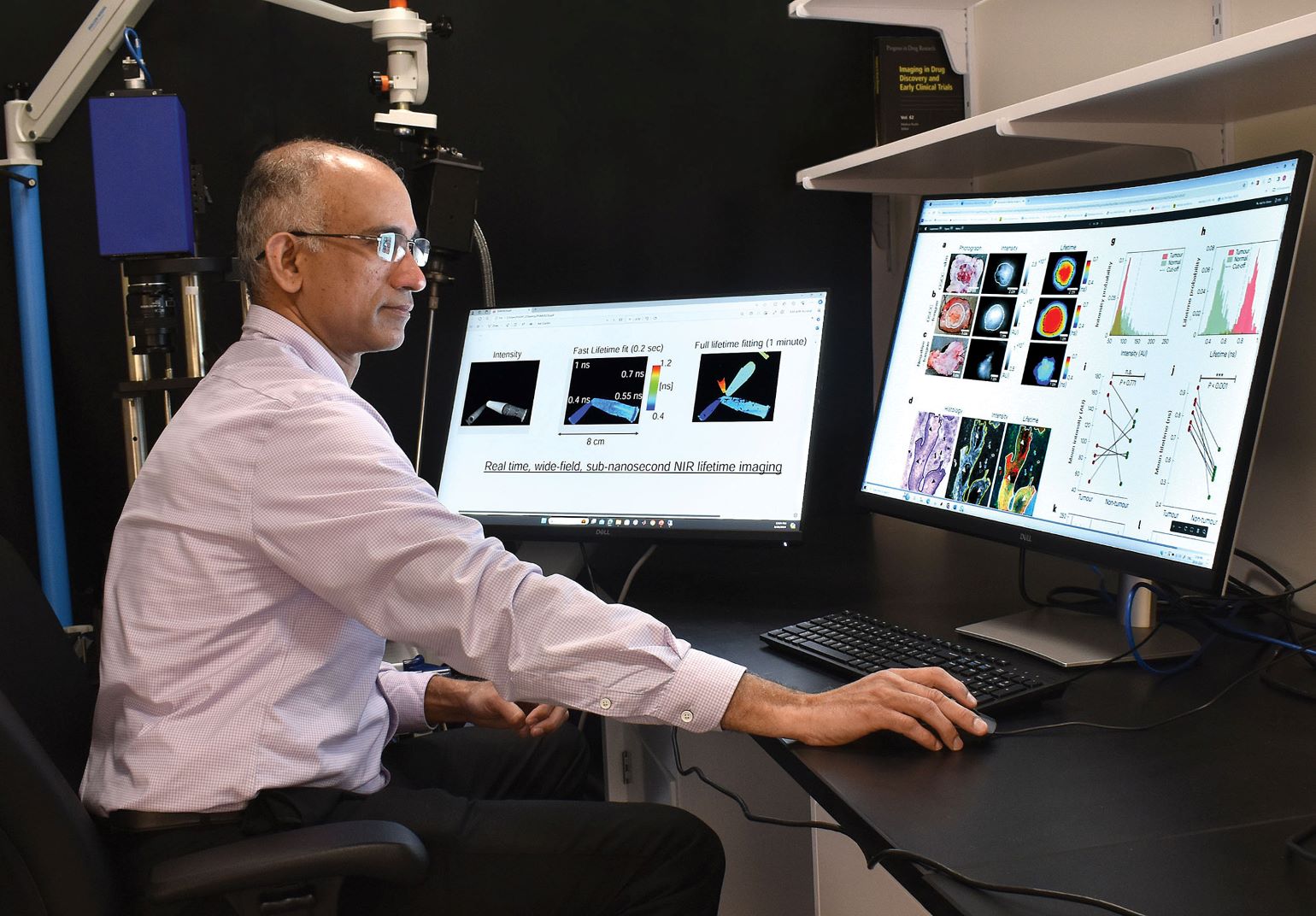
Figure 1
Anand T. N. Kumar, PhD, director of the Mike Toth Head and Neck Cancer Research Center, in his laboratory viewing images of fluorescence lifetime enhancement and microscopic cancer specificity in head and neck cancers.
Introducing the Kumar Laboratory
As a physicist and biomedical engineer by training, it is only fitting that Dr. Kumar's lifelong dream is to create a medical device that physicians use directly to benefit patients. After joining Massachusetts General Hospital in 2002, Dr. Kumar quickly found his research niche—combining medical imaging devices and the power of light to diagnose disease, specifically cancer.
He carefully studied fluorescence imaging, a technique that uses fluorescent markers to visualize specific molecules within cells and tissues. Fluorescence imaging can use dyes to target cancer-specific molecules, however, standard imaging methods seem to have limited accuracy for detecting tumor margins due to varying levels of these molecules among different tumors.
The standard approach to differentiating between tumor tissue and normal tissue is to rely on sight and the physical touch of the tumor. However, this process often causes physicians to either leave some cancer behind or to remove more tissue than is needed during surgery, which particularly in the case of head and neck cancer, can result in drastically changing a patient's appearance.
"A tumor is clearly visible after a CT or MRI is performed, but the physician cannot see this in real time as they are operating to remove tumors," said Dr. Kumar. "There is an urgent need to see the exact margin of a tumor in real time when patients are open in surgery."
He and his team further studied a different imaging technique, called fluorescence lifetime (FLT) imaging, that looks at the duration of time that fluorescent molecules remain in their excited state before emitting light.
FLT refers to the average time it takes for fluorescent molecules to return to their ground state once they are excited by a short laser pulse. Similar to a half-life measure of radioactivity, FLT is the time it takes for fluorescence to decrease by half from its initial value. The difference is, while the half-life of radioactive substances can be years to thousands of years, the halflife of fluorescence is often a fraction of a billionth of a second. Imaging cameras can capture these rapid changes in fluorescence decay times. FLT has many benefits compared to standard fluorescence imaging, which is widely used in medicine but is limited in its ability to distinguish disease from normal tissues. While FLT imaging has been widely used in research settings, its application for clinical studies in humans had been limited.
With this in mind, in 2016, Dr. Kumar's team evaluated a Food and Drug Administration (FDA)-approved fluorescent dye, known as indocyanine green (ICG), in cancer mouse models to evaluate whether FLT can help distinguish cancer better than standard fluorescence imaging. ICG typically accumulates in tumor tissue, but also settles in healthy tissue. Through multiple preclinical studies, Dr. Kumar's team found that the FLT of ICG in tumors is longer than the FLT in the normal tissue. This finding allowed the researchers to accurately distinguish between tumor tissue and normal tissue—a breakthrough, since most dyes currently being evaluated for tumor detection have non-specific uptake, like ICG, which limits their practical use.
After making this initial discovery in animal models, Dr. Kumar approached Kevin S. Emerick, MD, associate professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School and division director of Head and Neck Surgical Oncology at Mass Eye and Ear, and Mark A. Varvares, MD, FACS, John W. Merriam and William W. Montgomery professor and chair of the Department of Otolaryngology–Head and Neck Surgery at Harvard Medical School and chair of Otolaryngology–Head and Neck Surgery at Mass Eye and Ear and Mass General Hospital, about moving forward with patient trials. "Both Drs. Emerick and Varvares were extremely enthusiastic and confident that my laboratory was onto something monumental," said Dr. Kumar. "Their support was invaluable in the next steps of our study."
Initially, their human study analyzed tissue samples from patients who underwent liver surgery at Mass General Hospital and head and neck surgery at Mass Eye and Ear. Patients received an ICG injection one to three days before surgery.
In 2021, the first head and neck cancer patient (for this study) at Mass Eye and Ear was injected with ICG, and the tissue was analyzed with FLT imaging. Dr. Kumar and his team found that not only did the tumor tissue have a longer lifetime—or FLT—but zooming in at high resolution, they found that each individual cancer cell had a longer FLT as well.
Expanding on this research, the team collaborated with multiple institutions and assessed samples from more than 60 ICG injected patients with various cancer types, expanding the trial sites to include the University of Pennsylvania, University of Newcastle in the United Kingdom, and Leiden University in the Netherlands.
Dr. Kumar and colleagues were able to detect an FLT shift at the cellular level that was consistent across tumor types and in multiple patients. FLT imaging was also able to distinguish benign from metastatic lymph nodes. Overall, this novel technique demonstrated 97% accuracy in distinguishing tumor tissue from healthy tissue. These results were published in Nature Biomedical Engineering.
Although ICG is approved by the FDA for other uses, it is not yet approved for clinical use as a tumor marking agent. The researchers' next step is to conduct a large-scale clinical trial to evaluate the safety and efficacy of FLT imaging with ICG for tumor identification during surgery.
Dr. Kumar received a R01 grant from the National Institutes of Health for $2.2 million over five years to further develop and test an imaging device based on their technology to help surgeons visualize tumors better during surgery.
Drs. Emerick and Varvares will serve as co-investigators on this grant. The Kumar laboratory, which includes Rahul Pal, PhD, instructor of Otolaryngology–Head and Neck Surgery at Harvard Medical School, is now situated at Mass Eye and Ear, and the Mike Toth Head and Neck Cancer Research Center is well-positioned for upcoming research initiatives.
Advances in the Toth Center
Other exciting developments in the Toth Center come from the Shalhout and Faden laboratories. Sophia Z. Shalhout, PhD, assistant professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School and assistant scientist in the Toth Center, focuses on using artificial intelligence (AI) to develop more effective therapies, enhance the understanding of tumor biology, and improve how physicians diagnose, treat, and manage cancer. Daniel L. Faden, MD, FACS, assistant professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School and investigator in the Toth Center, concentrates on the development and use of liquid biopsies to detect human papillomavirus (HPV)-associated head and neck cancers.
In the Shalhout laboratory, a primary focus is to use AI to accelerate and enhance the drug discovery process. Notably, most patients do not respond to the current available therapies for advanced cancers of the head, neck, and skin, and those who respond at first often develop resistance or recurrence despite initial success. Dr. Shalhout recognizes that there is a dire need for new therapies and strategies to treat advanced cancers; currently, the drug development in oncology is labor-intensive, costly, and largely depends on trial and error.
Dr. Shalhout's team is developing deep learning and generative AI models, using combined expertise in computer science and chemistry to develop new drugs through algorithms capable of analyzing vast amounts of biological, chemical and pharmacological data. The AI models consider various factors such as protein structures and target selection, while interrogating a huge chemical space to identify novel candidate molecules that are structurally diverse yet likely to interact with the target. AI offers a much faster and more comprehensive approach to drug discovery than current traditional pathways allow. By leveraging AI, the lab aims to expedite the initial stages of drug development, potentially reducing the current timeline of seven to 12 years to a scale of months.
Another major project in the Shalhout laboratory involves the design and development of novel AI software capable of creating computer simulations of an individual patient's head, neck or skin cancer. These models can be used to predict the best treatment to offer a specific patient. The patient simulations have the ability to 'test' outcomes virtually, before treating a patient. Using computational models, doctors can simulate a tumor's response to various treatment options before implementing them in the clinical setting.
The computer models learn from various data sources, including genetic information, tumor characteristics and medical history. The Shalhout laboratory relies on a multidisciplinary team, including clinical coordinators, computer scientists, bioinformaticians, imaging experts, and pathologists, to drive this research forward.
"The end goal is for physicians to use these simulations to help devise treatment plans tailored to the individual cancer patient," shared Dr. Shalhout.
The Faden laboratory is one of the largest surgeon-run laboratories at Mass Eye and Ear. Comprised of eight scientists and trainees from all over the world, one of the primary focuses of the lab is developing and applying blood-based cancer diagnostics, or liquid biopsies. The goal of the lab is to detect, diagnose, and monitor cancers more accurately than current approaches and to do so in a noninvasive way.
Currently, the scientists in the lab are most heavily focused on HPV-associated head and neck cancers. The team has developed several liquid biopsies for HPV-associated cancer, which have been shown to outperform standard-of-care approaches in various clinical settings—all through a single blood sample.
Most recently, the researchers in the Faden laboratory developed a next generation liquid biopsy called HPV-DeepSeek; this test is more than 25 times more sensitive than the original tests and can also look at many other cancer-related features, which are then analyzed using machine learning. HPV-DeepSeek is specifically designed for addressing low tumor burden settings such as asymptomatic cancer screening and minimal residual disease detection after surgery.
"Our goal in developing, validating, and applying liquid biopsy diagnostics like HPV-DeepSeek is to study large unmet needs in cancer care, such as blood-based cancer screening in high-risk patient populations, with the hope of increasing early cancer detection and thereby, decreasing cancer-related mortality," said Dr. Faden. "Our research is leading us into novel, and often unexpected directions, which is really quite exciting."
New Leadership, New Collaborations
According to Dr. Kumar, his vision for the future of the Toth Center begins with collaboration. Each laboratory has its specific focus, but all of the research is translational with the common goal of better identifying and curing cancer. With Dr. Kumar at the helm, the Toth Center scientists will have regular meetings to discuss ideas for collaborations that combine each research program's expertise, ultimately leading to new grant opportunities and publications.
Additional Toth Center transformational tactics include hosting a monthly seminar series with invited speakers, both within and outside the Mass General Brigham system, to present on innovative topics in relation to head and neck cancer research.
They will also host an annual workshop to showcase the cutting-edge imaging and computational tools for head and neck cancer imaging and treatment being developed at the Toth Center.
"A common theme at the Toth Center is leveraging our diverse backgrounds and expertise—from physics, engineering, chemistry and medicine—to advance our shared goal of improving diagnostic testing and treatment options for patients with head, neck and skin cancers," emphasized Dr. Kumar. "I am thrilled to have the opportunity to lead this renowned Center."
Learn more about the Department of Otolaryngology–Head and Neck Surgery at Mass Eye and Ear
Refer a patient to Mass Eye and Ear/Mass General Brigham