Racial Gap Amongst U.S. Shoulder Arthroplasty Patients Persists
Key findings
- This retrospective study of nationally representative U.S. hospital data examined the prevalence of total shoulder arthroplasty (TSA) and reverse TSA (RTSA) among Black and white patients
- In 2012, the incidence of TSA/RTSA per 100,000 persons was 18.7 for white patients and 5.1 for Black patients; in 2017, the respective figures were 36.9 and 10.8
- These disparities were evident regardless of insurance type
- On average, Black patients had longer hospital stays, compared with white patients, and were significantly more likely to be discharged to a secondary facility (e.g., rehab or nursing home)
- Additionally, Black patients had increased odds of complications and death after TSA/RTSA
Subscribe to the latest updates from Orthopaedics Advances in Motion
In 2011, the U.S. Department of Health and Human Services launched a comprehensive action plan to reduce racial disparities in medicine, which prompted several orthopedic-specific initiatives. However, no national study since 2011 has examined whether racial disparities persist in the number of patients undergoing total shoulder arthroplasty (TSA) or reverse TSA (RTSA).
Matthew J. Best, MD, Sports Medicine fellow, and Scott D. Martin, MD, director of the Joint Preservation Service within the Department of Orthopaedics Sports Medicine Center at Massachusetts General Hospital, and colleagues have determined that racial differences in TSA/RTSA not only persist but have widened since a national study examined the years 1998–2011. Their report appears in the Journal of Shoulder and Elbow Surgery.
Study Methods
The researchers made use of the U.S. government's National Inpatient Sample (NIS), which provides information on more than 35 million hospitalizations. They reviewed all records in which TSA or RTSA was the primary listed procedure between 2012, when the NIS improved its sampling method, to 2017, the most recent year available.
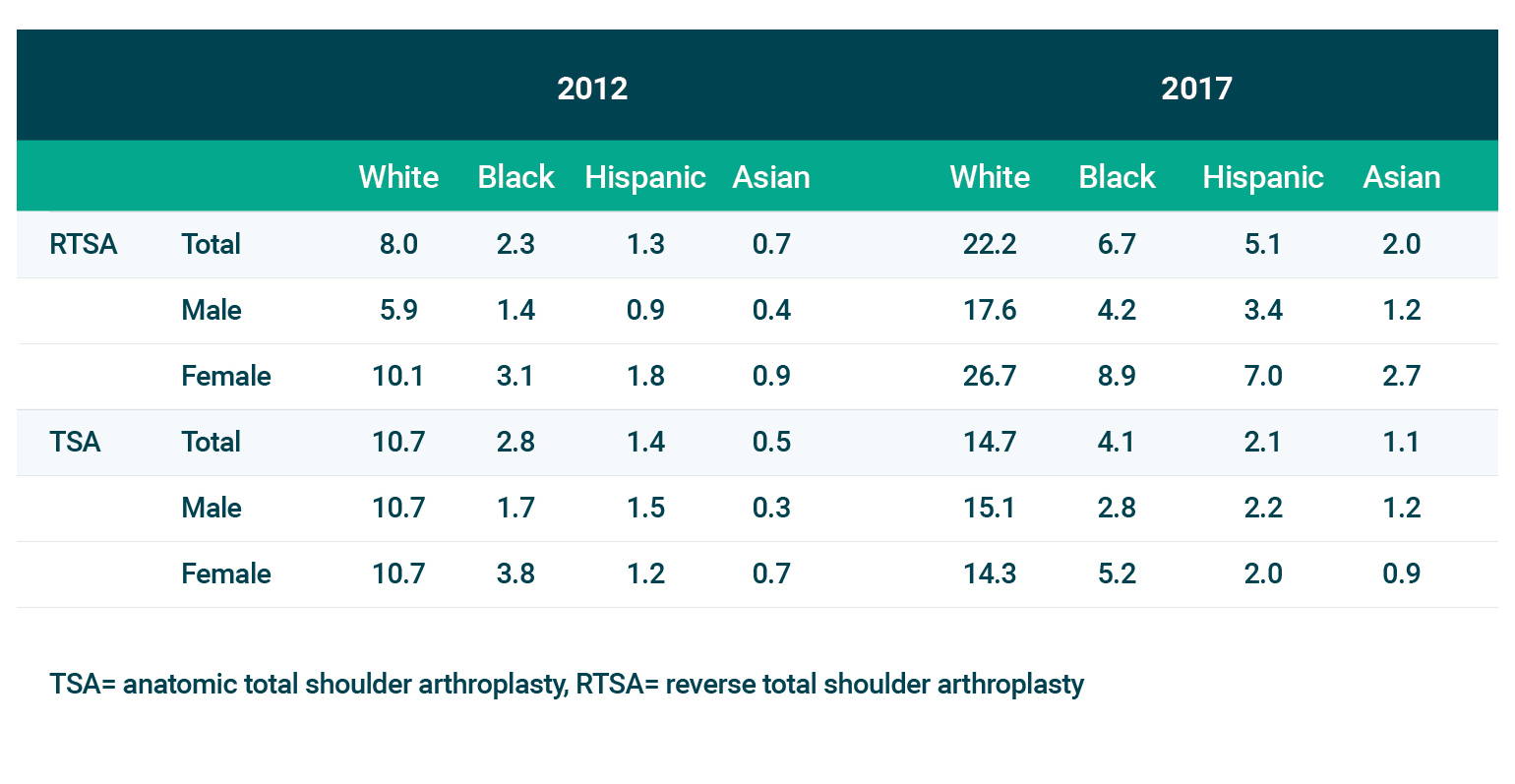
To be in alignment with previous research, the team focused on white patients (n=382,600) and Black patients (n=19,030). Data on Latinx and Asian patients are presented in the supplemental table below.
Race-Adjusted Incidence
As calculated using U.S. Census population data for each year, the race-adjusted incidence of TSA/RTSA was:
2012:
- White patients: 18.7 per 100,000 persons
- Black patients: 5.1
- Difference: 13.6
2017:
- White patients: 36.9 per 100,000 persons
- Black patients: 10.8
- Difference: 26.1
Thus, the widening of the racial disparity from 2012–2017 was 12.5 per 100,000. Black patients underwent TSA/RTSA at lower rates, regardless of insurance type (Medicare, Medicaid or private insurance).
Other Measures
Compared with white patients, Black TSA/RTSA patients had significantly:
- Longer average hospital stays
- Higher rates of discharge to a facility
- Higher risk of certain complications:
- Acute myocardial infarction (OR, 1.43)
- Pulmonary embolism (OR, 1.97)
- Acute renal failure (OR, 1.40)
- Sepsis (OR, 1.68)
- Surgical site infection (OR, 2.19)
- Higher risk of death (OR, 2.88)
Addressing A Worsening Problem
A previous study, published in the Journal of Racial and Ethnic Health Disparities, examined NIS data on TSA for the years 1998 to 2011. The difference between white and Black patients in 2011 was 8.9 per 100,000—so the gap has nearly tripled since then.
In 2011, the American Academy of Orthopaedic Surgery, the Orthopaedic Research Society and the Association of Bone and Joint Surgeons jointly published in Clinical Orthopaedics and Related Research a "call to arms" for eliminating musculoskeletal health care disparities. It addresses both general musculoskeletal topics and some specifics, including lower-extremity arthroplasty. It seems that upper-extremity arthroplasty needs to be added to the list.
Additionally, surgeon education should be improved to raise awareness of the problem. A survey of the American Orthopaedic Association, published in 2017 in the Journal of Racial and Ethnic Health Disparities, showed only 9% of respondents believe patients often receive different orthopedic care based on race/ethnicity.
view original journal article Subscription may be required
Learn more about the Shoulder Service at Mass General
Refer a patient to the Department of Orthopaedic Surgery