Nerve Stretch–Reduction Protocol Reduces Risk of Nerve Injury During Latarjet Surgery
Key findings
- Based on findings during a previous study that relied on intraoperative neuromonitoring, shoulder surgeons at Mass General developed a new protocol for the open Latarjet procedure
- Nerve alerts means the nerve may be under tension and this could mean the potential for nerve "injury"
- The overall rate of clinically detectable nerve alerts decreased from 18.4% before implementation of the protocol to 6.3% afterward
- The rate of motor nerve alerts decreased from 10.5% to 4.2%
- The rate of permanent motor dysfunction decreased from 5.3% to 2.1%
Subscribe to the latest updates from Orthopaedics Advances in Motion
Latarjet is a proven treatment for recurrent anterior glenohumeral instability, with less risk of recurrent instability compared with Bankart repair. However, clinically detectable injury to the nerves of the brachial plexus has been documented in up to 20% of cases.
In a previous study, Jon J.P. Warner, MD, chief of the Shoulder Service at Massachusetts General Hospital, and colleagues used real-time neuromonitoring during open Latarjet surgery. It demonstrated a significant incidence of nerve dysfunction, presumably from nerve stretch.
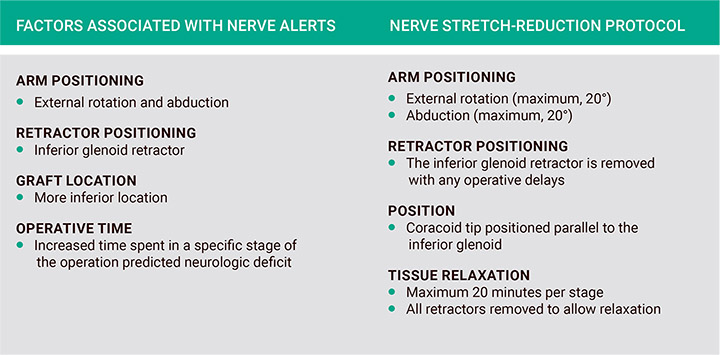
Fig. 1: Factors identified as high risk for intraoperative nerve alerts and surgical technique alteration.
Therefore, the researchers created a nerve stretch–reduction protocol for the Latarjet procedure (Figure 1) and conducted a nonrandomized, uncontrolled before-after study to evaluate its impact.
In the Journal of Shoulder and Elbow Surgery, they report that the protocol reduced the risk of motor and sensory deficits, although not significantly so.
The researchers evaluated how Dr. Warner's outcomes with the Latarjet procedure compared in two cohorts:
- 38 patients treated between January 1, 2008, and December 31, 2010, and followed for an average of 16.5 months (group 1)
- 48 patients treated between January 1, 2013, and December 31, 2015, after the nerve stretch–reduction protocol was implemented, and followed for an average of 7.5 months (group 2)
- At two, six and 16 weeks postoperatively the patients rated their pain on a visual analog scale and assigned a Subjective Shoulder Value (SSV) score
In both groups, there was no significant change in forward elevation or external rotation between the preoperative and postoperative evaluations. The average pain and SSV scores improved significantly from baseline in both groups, and the postoperative pain score was significantly better in group 2 than in group 1 (2.1 vs 0.19; =.01).
Nerve injuries were as follows:
- Group 1: Seven nerve injuries, including three isolated sensory deficits and four combined motor and sensory deficits. Four of the nerve injuries fully recovered at an average of 4.6 months, but three nerves did not completely recover
- Group 2: Three nerve injuries, including one isolated sensory deficit and two combined motor and sensory deficits. One of the motor deficits was due to a musculocutaneous nerve injury, which fully resolved within five months. The other was due to an axillary nerve injury. When it did not resolve, surgical exploration detected a neuroma. Following nerve transfer surgery the patient had residual motor weakness and sensory deficit
The overall incidence of nerve injuries was 18.4% in group 1 and 6.3% in group 2, and the respective rates of motor nerve injuries were 10.5% and 4.2%. The incidence of permanent motor dysfunction decreased from 5.3% to 2.1%.
None of these differences was statistically significant, which the researchers attribute to the small number of patients.
Dr. Warner and his colleagues conclude that surgical technique seems to be important in reducing the incidence of nerve injury during the Latarjet procedure. Their article gives a detailed description of their currently recommended technique.
view original journal article Subscription may be required
About the Shoulder Service at Mass General
Refer a patient to the Shoulder Service at Mass General