Trial Without Error: Using 3D Planning for Shoulder Replacement
In This Article
- Orthopedic surgeons perform shoulder arthroplasty less often than hip or knee replacement in the United States, but its frequency is on the rise
- Three-dimensional planning software may improve outcomes for shoulder arthroplasty
- A new technology allows surgeons to install the prosthetic joint with greater foresight and precision
Orthopedic surgeons perform shoulder arthroplasty less often than hip or knee replacement in the United States, but its frequency is on the rise. The number of such surgeries has increased between 8% and 12% per year, and that figure is expected to balloon to 600% from its current rate by the year 2030 as a consequence of an aging population.
Subscribe to the latest updates from Orthopaedics Advances in Motion
While the procedures can be complicated, three-dimensional (3D) planning software may improve outcomes (Figure 1). Jon Warner, MD, chief of the Massachusetts General Hospital Shoulder Service, uses a program in which a digital model of a patient’s shoulder is generated by a computer. This can be used both to plan the surgery and to generate a custom drill guide with 3D printing, which can facilitate the surgery on the patient (Figure 2).
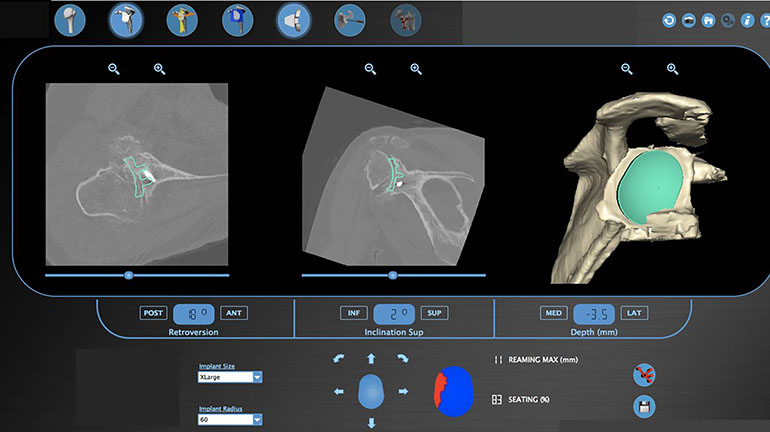
Fig. 1: Virtual Planning Software Showing Templates of the Glenoid Prosthesis.
The software automatically calculates and displays the reaming depth the surgeon will need to use and the component seating percentage.
There are several patient-specific software options for surgeons to choose from. According to a review in Current Review of Musculoskeletal Medicine, in 2016 there were four commercially available implant systems that offer comprehensive 3D planning software in which the surgeon uploads CT scans and designs their own preoperative plan and one that offers a 3D preoperative plan created by engineers based on the patient’s CT scans and sent to the surgeon for approval and/or revision.
The 3D planning technology allows surgeons undertaking a total shoulder arthroplasty to install the prosthetic joint with greater foresight and precision. A study published in the Journal of Shoulder and Elbow Surgery in 2015 found that one such system correlated accurately with the final procedure, and that the guides it produced caused no unforeseen complications. A review of studies published in Current Review of Musculoskeletal Medicine in 2016 concluded that recent studies showed “improved anatomic placement of glenoid components” as a result of the use of patient-specific instrumentation and computer-guided software. However, the authors note that since the technology is so new, more studies are needed to look at implant longevity and longer-term outcomes.
Challenges with Total Shoulder Replacement
Debilitating shoulder injuries can greatly impact quality of life, inhibiting a wide range of daily activities. They can also affect rest cycles; pain from shoulder osteoarthritis has a more profound effect on sleep than that from hip or knee arthritis.
Shoulder arthroplasty, however, presents significant anatomical challenges. In the shoulder joint, the head of the humerus articulates in the glenoid cavity of the scapula. For this surgery, the glenoid surface must be replaced with a prosthetic version. The specific position of the glenoid component is key for the success of the shoulder replacement. Placement is complicated by the anatomical features of the joint and the occlusion of view from muscle and other tissue.
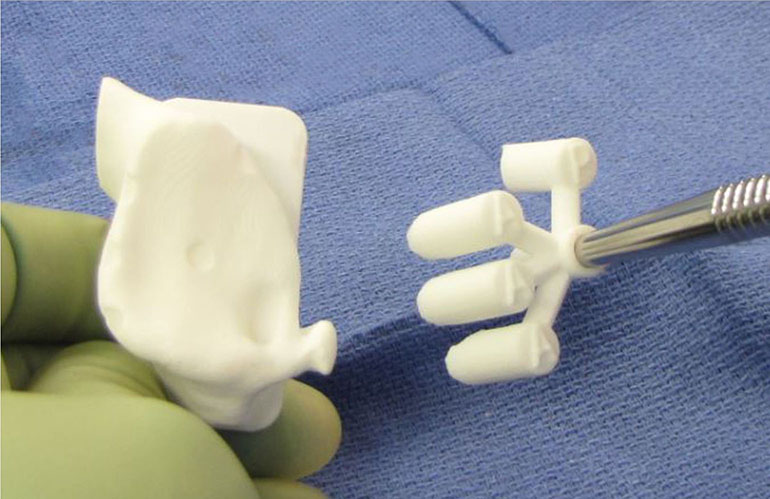
Fig. 2
Patient-specific 3D guide produced by virtual planning software.
Furthermore, most surgeons who perform joint replacements also perform comparatively fewer shoulder replacements. While most orthopaedic surgeons perform 50 to 100 hip and knee replacements annually, roughly 90% of orthopaedic surgeons perform five or fewer shoulder arthroplasties every year.
As a result, the failure rate of shoulder replacement surgery is higher than that of hip or knee replacement, with 9.8% of shoulder replacement surgeries requiring revision after 10 years.
Three-dimensional Virtual Shoulder Replacement Surgery
Virtual planning software aims to improve these outcomes. A candidate for surgery first undergoes multiple CT scans to capture the shoulder region on various planes. These images are then synthesized into a 3D digital model, a process that only takes minutes. This anatomically-accurate model is then provided to the surgeon, who can then perform a simulation of the procedure on a computer. These programs also include representations of prosthetics, allowing the surgeon to fit different sizes on the patient’s virtual shoulder.
“This is trial without error,” Dr. Warner says. “It allows me to anticipate any problems in advance, and to know exactly what steps I’m going to take and what specific replacement parts I will use.”
After walking through the surgery, a three-dimensional drill guide is created that helps the surgeon precisely position the glenoid guide pin that is used for placement of the new glenoid component specific to the patient. This cuts down on time in the operating room.
The available software implant systems vary slightly in how the planning tool works, the shape of the guide generated by the software and the anatomical landmarks used as reference for positioning the guide.
The virtual planning approach confers additional benefits for more complicated cases. Some patients might be better candidates for a reverse shoulder replacement, in cases where severe bony deformities or an absent or seriously damaged rotator cuff precludes a straightforward replacement. The simulator allows surgeons to try out conventional or reverse replacements in virtual space on the patient model.
While data on outcomes with 3D planning are still being collected, Dr. Warner emphasizes that using the simulator presents no risk for patients. The tool helps supplement the surgeon’s decision-making, may cut down on surgery time and allows for more planned and precise procedures.
“It’s analogous to a flight simulator for pilots,” says Dr. Warner. “It helps surgeons become better at what they do.”
Learn more about Mass General's Shoulder Service
Request a shoulder appointment