Venous Thromboembolism Disease Prophylaxis in Foot and Ankle Surgery
Key findings
- The role of venous thromboembolism disease (VTED) prophylaxis in foot and ankle surgery remains unclear because most data are of low quality
- Decisions about chemical VTED prophylaxis after foot and ankle surgery should be individualized based on risk factors
- Principal risk factors for VTED after foot and ankle surgery are history of VTED, history of recent malignancy and prolonged lower-extremity immobilization
Subscribe to the latest updates from Orthopaedics Advances in Motion
There are numerous society guidelines on how to prevent venous thromboembolism disease (VTED) in the hip and knee population. However, there is little guidance available on preventing VTED after foot and ankle surgery. The severity of injuries, surgical procedures and post-operative immobilization protocols vary widely when compared to hip and knee arthroplasty. Therefore, the recommendations used after hip and knee arthroplasty cannot be safely extrapolated to foot and ankle surgery.
Christopher DiGiovanni, MD, chief of the Mass General Foot & Ankle Center, Daniel Guss, MD, MBA, foot and ankle orthopedic surgeon at Massachusetts General Hospital and colleagues recently explored the literature on VTED prophylaxis after foot and ankle surgery. In Orthopedic Clinics of North America, they conclude that the indications for VTED prophylaxis, the types of prophylaxis recommended and the efficacy of prophylaxis all remain unsettled.
The few studies available are of low quality and contradictory, the authors say. Even the incidence of VTED after foot and ankle surgery has not been properly defined because of the diversity of injuries, procedures and host factors.
According to the American Orthopedic Foot & Ankle Society (AOFAS), there are three primary risk factors for VTED in foot and ankle surgery:
- Prior VTED
- History of recent malignancy
- Lower-extremity immobilization with plaster for at least five weeks
According to the AOFAS, the most often overlooked secondary risk factor is a family history of VTED. Non-weight-bearing status, hospitalization and bed rest greater than three days are also risk factors, as are a high injury severity score, use of general anesthesia, hindfoot arthrodesis, total ankle replacement surgery and both surgical and nonsurgical management of ankle fractures and Achilles tendon ruptures.
Besides malignancy, certain comorbidities are also associated with greater VTED risk: venous stasis/varicose veins, diabetes and connective tissue disorders. Still, other risk factors are obesity, age >40 and use of an oral contraceptive or hormone replacement therapy.
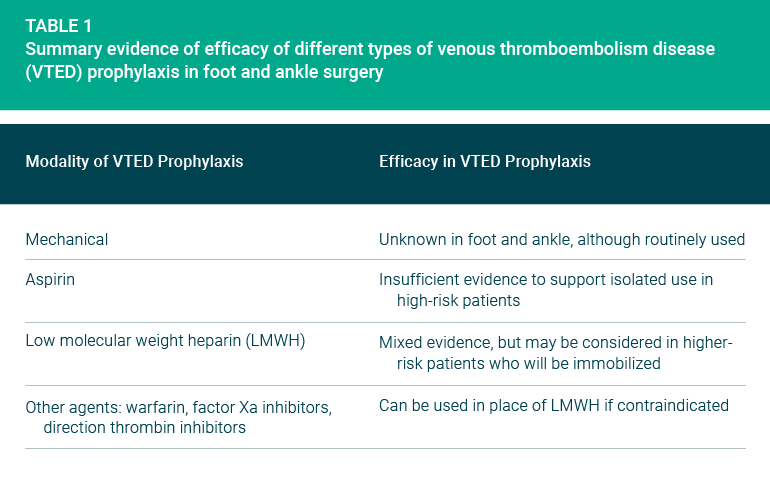
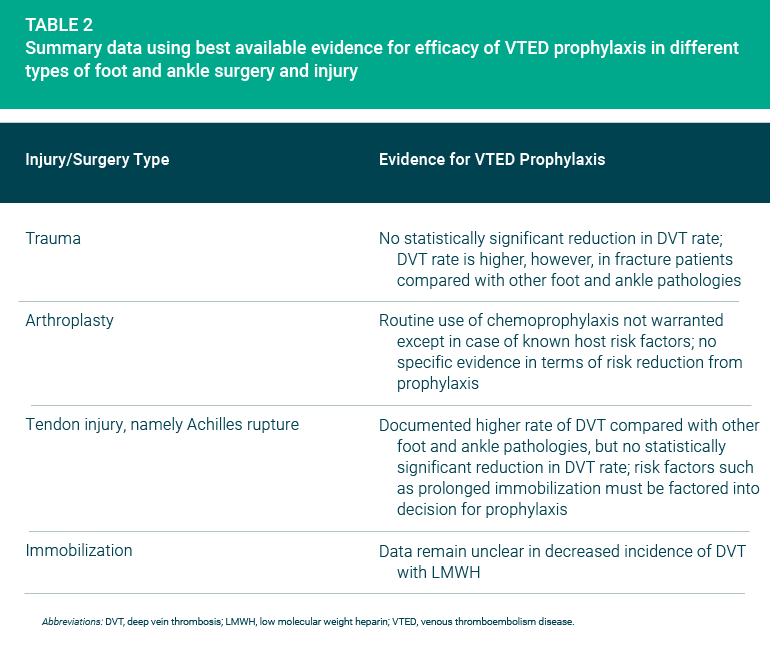
Only limited evidence is available about the efficacy of VTED prophylaxis. Table 1 summarizes the reviewers’ findings according to type of prophylaxis, and Table 2 summarizes their findings according to type of injury or surgery.
The authors do present three bottom-line recommendations about chemical VTED prophylaxis after foot and ankle surgery:
- It should be given to patients with previous history of VTED
- It’s unlikely to be needed by patients who do not have a previous history of VTED or other risk factors, as long as they can be mobilized post-operatively
- It should be considered for patients older than 50 who have an ankle fracture and those older than 40 who have an Achilles tendon injury
view original journal article Subscription may be required
Learn more about the Foot & Ankle Center