Use of Puncture Capsulotomy During Hip Arthroscopy
In This Article
- Massachusetts General Hospital clinician Scott Martin, MD, is revisiting puncture capsulotomy, a promising technique for performing hip arthroscopy and treating femoroacetabular impingement
- Puncture capsulotomy offers improvements over extended T-capsulotomies
- Normal anatomy is preserved with minimal impact on stability and iliofemoral ligament
- Biomechanics is maintained with improved recovery
The art of hip arthroscopy has progressed immensely in the last 20 years—from simple surgical techniques to complex procedures such as labral repair, femoroacetabular osteoplasty, labral reconstruction and cartilage repair. The arthroscopic hip-joint exposure and instrument maneuverability required for these complex procedures is challenging and has led to the common surgical technique of extended capsulotomy. This can solve the problem of exposure and maneuverability, but can also lead to other problems such as instability, heterotopic bone formation, seromas and excessive adhesions that lead to stiffness of the hip joint.
Subscribe to the latest updates from Orthopaedics Advances in Motion
For several years, Scott D. Martin, MD, director of the Joint Preservation Service within the Department of Orthopaedics Sports Medicine Center at Massachusetts General Hospital, has been revising a surgical approach for performing hip capsulotomy, called puncture capsulotomy (PC). This approach creates small, rounded holes in and around the hip, including the iliofemoral ligament, instead of surgically incising or resecting the ligament (Figure 1).
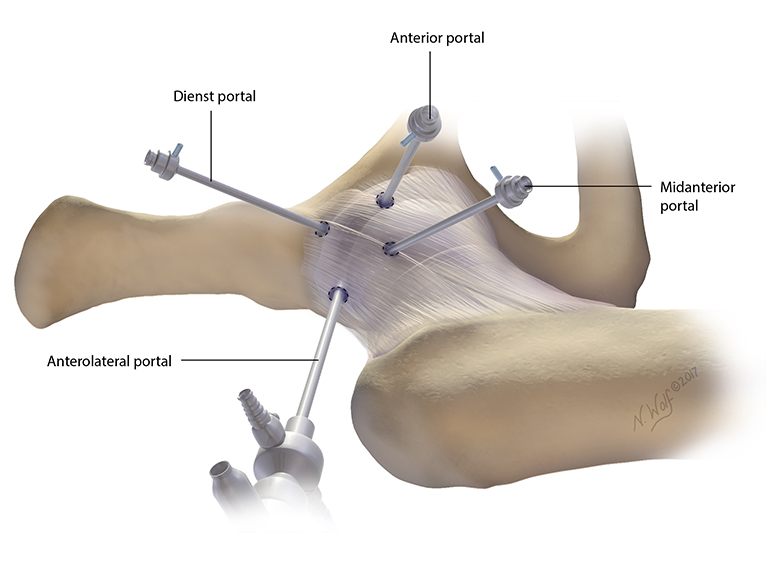
Figure 1: Puncture capsulotomy showing anterolateral (viewing), anterior, mid-anterior and Dienst portals. Illustration by Nicole Wolf, MS, © 2017.
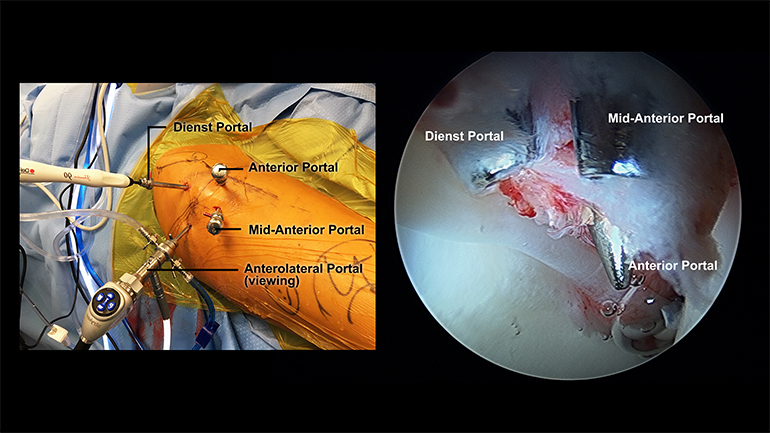
Figure 2: Quadrilateral orientation of the portals. Photos courtesy of Scott D. Martin, MD, © 2017.
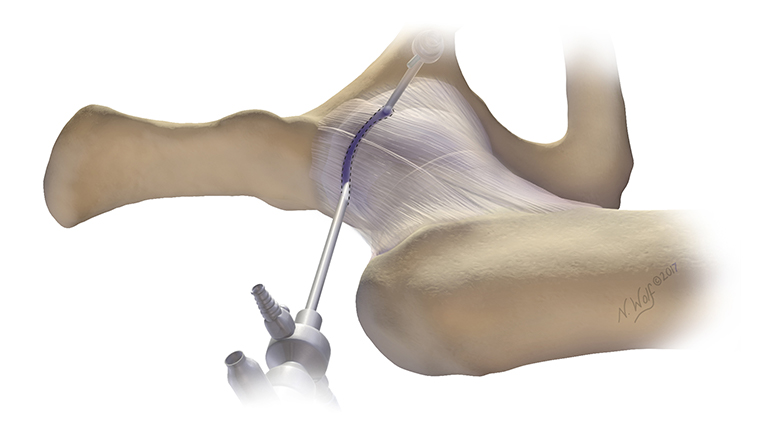
Figure 3a: Interportal capsulotomy. Illustration by Nicole Wolf, MS, © 2017.
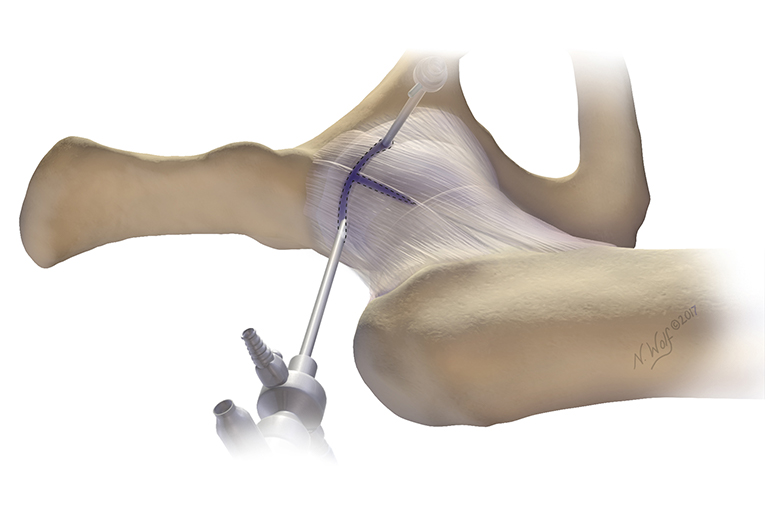
Figure 3b: T-capsulotomy. Illustration by Nicole Wolf, MS, © 2017.
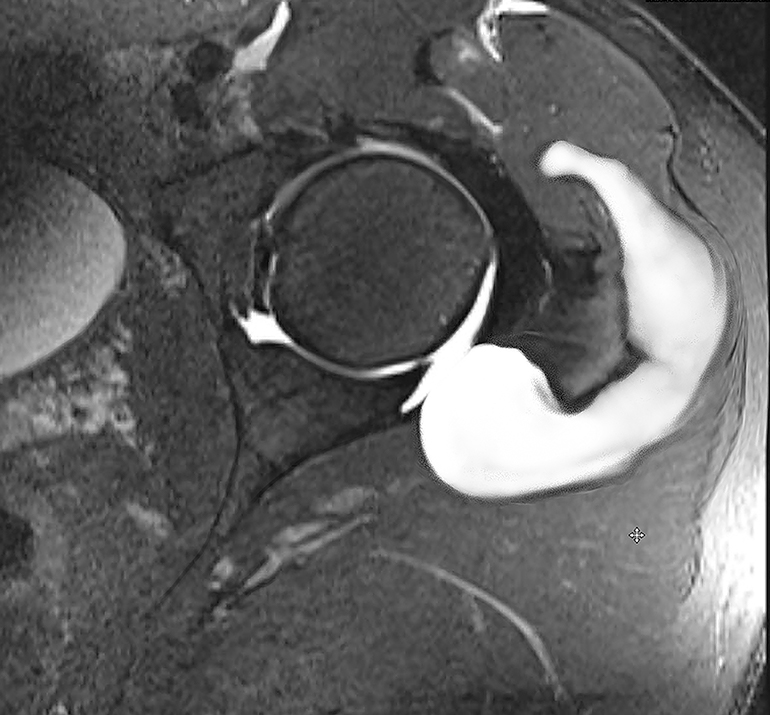
Figure 4: MRI of the left hip, demonstrating a seroma. Photo courtesy of Scott D. Martin, MD, © 2017.
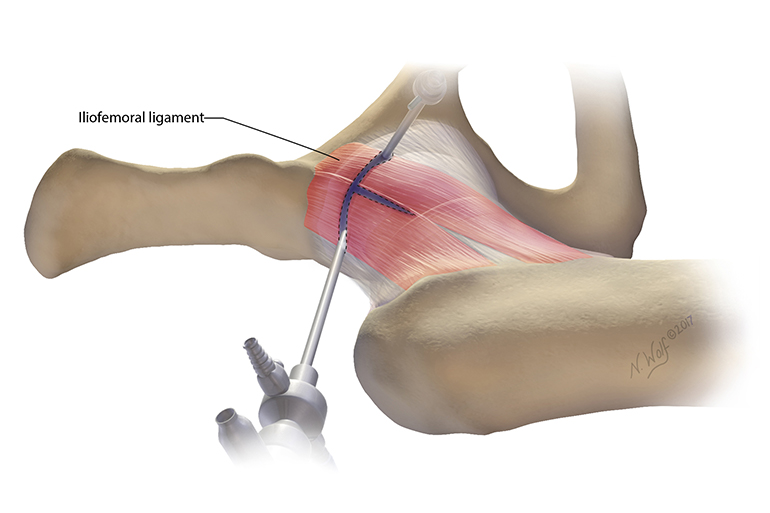
Figure 5: T-capsulotomy slices the iliofemoral ligament. Illustration by Nicole Wolf, MS, © 2017.
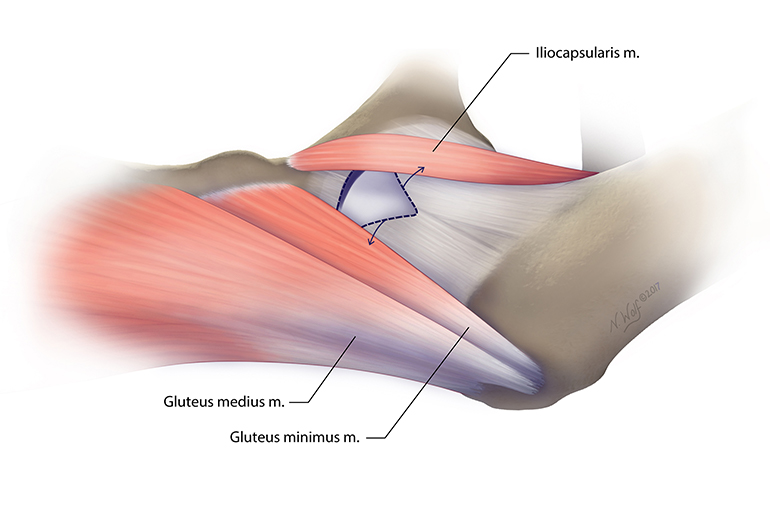
Figure 6: The iliocapsularis and gluteus minimus/medius pull the capsule in opposing directions during flexion and external rotation of the hip. Illustration by Nicole Wolf, MS, © 2017.
Puncture Capsulotomy: Minimizing Capsule and Ligament Damage
Using a puncture capsulotomy technique to cleanly pierce through the ligament to place his surgical portals, Dr. Martin creates an average of three to four portal-access punctures to achieve maximal visualization of and surgical access to the hip joint (Figure 2).
“I prefer this technique because I don’t want to cut across the iliofemoral ligament, the strongest ligament of the hip, and then trust that my repair of the ligament is going to hold up postoperatively,” says Dr. Martin. “Using this technique, I’ve had no problems accessing the central or peripheral compartments, or performing complex procedures.”
Dr. Martin has conducted more than 1,500 hip arthroscopic procedures using this technique, with great success.
The State of the Art
The most commonly used methods of hip capsulotomy include the interportal and extended T-capsulotomies. Both involve capsular release by cutting thorough the capsule to connect arthroscopy portals (Figures 3a and 3b). For T-capsulotomy, the surgeon must cut through the main stabilizing ligament of the hip, the iliofemoral ligament, then cut across it to connect the horizontal end to the vertical end, making the shape of a T (Figure 5).
While T-capsulotomy offers improved visualization to see the whole hip, including the central and peripheral compartments, the capsular release often means patients can develop internal scarring, as well as heterotopic ossification and poor capsular healing with the development of seromas (Figure 4). It can be made worse if the surgeon fails to repair the extended capsulotomy, allowing the body to repair the surgical injury on its own.
“The problem is that when your muscles contract, the iliocapsularis—which is on the top of the hip—pulls that T-capsulorrhaphy repair in one direction, and the gluteus medius and minimus pull it in the opposite direction,” explains Dr. Martin. “Every time the patient flexes and rotates their hip, it strains the surgical site, which can lead to failure of the capsular repair” (Figure 6).
“All of these potential side effects can leave patients with significant stiffness and hip instability,” he explains. His concern over these complications led him to reconsider and perfect PC, a technique more widely practiced before the introduction and popularity of extended capsulotomy.
Boosting Recovery and Tracking Outcomes
A notable benefit of the PC procedure is that immediately after surgery, patients can weight-bear as tolerated and perform activities of daily living without restrictions.
“I tell them not to intentionally attempt to stretch the hip or do yoga, but patients are immediately able to weight-bear, get into a car, dress and climb stairs,” Dr. Martin explains. Patients use crutches to maintain a balanced gait so the pelvis remains level when walking. In contrast, many surgeons protect weight-bearing and assist regaining motion after T-capsulotomy with derotational braces and continuous passive motion.
“I haven’t found one hip patient who I can’t do this with yet,” he says, including obese patients or those with complex cases. “I always say respect the anatomy, preserve it, and the patients will benefit.”
Learn more about the Center for Hip and Knee Replacement
Schedule an appointment with the Center for Hip and Knee Replacement