Cell Therapy That Repairs Cornea Damage With Patient's Own Stem Cells Achieves Positive Phase I Trial Results
In This Article
- A multicenter team led by clinician scientist Ula Jurkunas, MD, reports the results of a phase I trial of a revolutionary stem cell treatment called cultivated autologous limbal epithelial cell transplantation (CALEC)
- CALEC was safe and well-tolerated over the short term in four patients with significant chemical burns in one eye
- According to the study, the patients who were followed experienced restored cornea surfaces—two were able to undergo a corneal transplant, and two reported significant improvements in vision without additional treatment
A multicenter team led by Ula Jurkunas, MD, associate director of the Cornea Service at Mass Eye and Ear, reports the results of a phase I trial of a revolutionary stem cell treatment called cultivated autologous limbal epithelial cell transplantation (CALEC), which was found to be safe and well-tolerated over the short term in four patients with significant chemical burns in one eye. According to the study published in Science Advances, the patients who were followed for 12 months experienced restored cornea surfaces—two were able to undergo a corneal transplant, and two reported significant improvements in vision without additional treatment.
Subscribe to the latest updates from Ophthalmology Advances in Motion
In CALEC, stem cells from a patient's healthy eye are removed via a small biopsy and then expanded and grown on a graft via an innovative manufacturing process at the Connell and O'Reilly Families Cell Manipulation Core Facility at Dana-Farber Cancer Institute. After two to three weeks, the CALEC graft is sent back to Mass Eye and Ear and transplanted into the eye with corneal damage.
While the phase I study was designed to determine preliminary safety and feasibility before advancing to a second phase of the trial, the researchers consider the early findings promising.
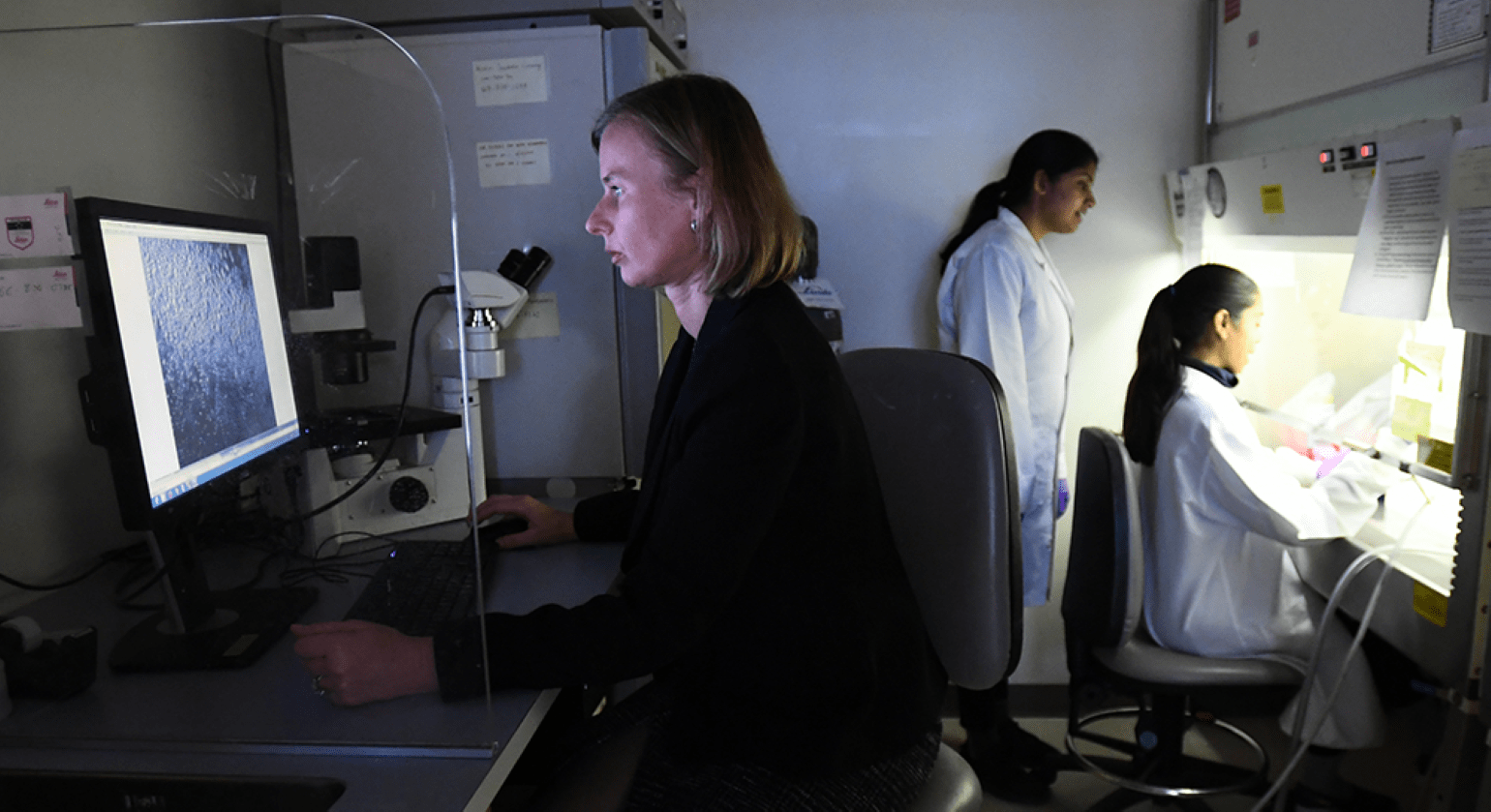
Figure 1
Dr. Ula Jurkunas (left) at monitor with researchers in her laboratory. Image courtesy of Ula Jurkunas, MD.
"Our early results suggest that CALEC might offer hope to patients who had been left with untreatable vision loss and pain associated with major cornea injuries," said principal investigator and lead study author Dr. Jurkunas. "Cornea specialists have been hindered by a lack of treatment options with a high safety profile to help our patients with chemical burns and injuries that render them unable to get an artificial cornea transplant. We are hopeful with further study, CALEC can one day fill this crucially needed treatment gap."
The CALEC project is a collaboration between Jurkunas and colleagues in the Cornea Service at Mass Eye and Ear, researchers at Dana-Farber Cancer Institute, led by Jerome Ritz, MD, Boston Children's Hospital, led by Myriam Armant, PhD, and the JAEB Center for Health Research. The clinical trial represents the first human study of a stem cell therapy funded by the National Eye Institute (NEI), a part of the National Institutes of Health (NIH).
Learn more about research in Ophthalmology at Mass Eye and Ear/Mass General
Refer a patient to Mass Eye and Ear/Mass General