Multidisciplinary Care for Pulmonary Embolism
In This Article
- Pulmonary embolism calls for a coordinated clinical approach
- In October 2012, physicians at Massachusetts General Hospital created a multidisciplinary, rapid-response team to coordinate care for PE patients
- Since the introduction of the Mass General Pulmonary Embolism Response Team (PERT), the first such program in the United States, PE-mortality for patients with massive PE fell to 25%, which is less than half when compared to some national reports
Pulmonary embolism (PE) is a major cause of death in hospitalized patients, and its incidence in the United States is on the rise. PE is fatal in about 10% of cases in the first hour if not recognized and treated, and mortality can be up to 50% at three months for those with higher-risk forms of the condition.
Subscribe to the latest updates from Cardiovascular Advances in Motion
In October 2012, physicians at Massachusetts General Hospital created a multidisciplinary, rapid-response team to coordinate care for PE patients. Since the introduction of the Mass General Pulmonary Embolism Response Team (PERT), the first such program in the United States, PE-mortality for patients with massive PE fell to 25%, which is less than half when compared to some national reports. Figures from the first 30 months of the program were published in the August 2016 issue of Chest.
“Our purpose is to advance the diagnosis, treatment and outcomes of patients with PE,” says Rachel Rosovsky, MD, MPH, a hematologist and PERT executive committee member at Mass General. “We want to respond expeditiously, leverage the rich input from a multidisciplinary team of experts, coordinate the care of all the services, provide the most appropriate therapeutic options and collect data on treatments and outcomes. Ultimately, we want to develop better protocols.”
How PERT Activation Works
When a PE is suspected or documented at Mass General, the physician calls a live, 24-hour hotline. A page is sent to the PERT fellow on call who does the initial patient evaluation with direct involvement of an attending physician. The two decide whether to activate a broader team. If so, every specialist on the team is paged to attend a web-based meeting, conducted using HIPAA-compliant channels, within approximately 90 minutes. The team reviews each patient’s clinical course and images, and sometimes even the patient or family members are included on the call.
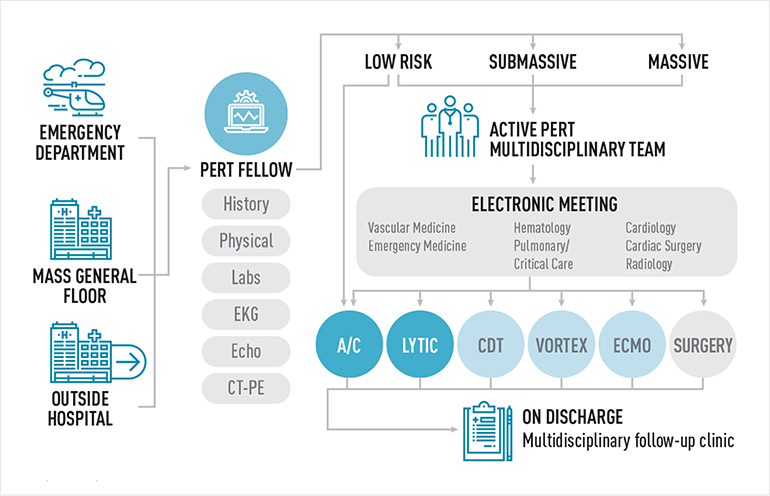
Fig. 1: The Process of PERT Activation
When a pulmonary embolism is diagnosed or suspected at Mass General, a PERT fellow is paged, gathers pertinent clinical information and assesses the severity of the case. If necessary, the entire multidisciplinary team is activated and attends an electronic meeting. Treatment options are discussed and necessary resources are mobilized. Once discharged, the patient follows up in a multidisciplinary outpatient setting.
“We discuss the case, review the pros and cons for each option, generate diagnostic and treatment recommendations and assemble appropriate resources if advanced therapies are needed,” says Dr. Rosovsky. “By creating this system, we hope to improve the decision making, efficacy and orchestration of care for PE patients.”
Since its inception, the team has responded to 689 PERT contact calls. About 63% have engaged the entire multidisciplinary team. Between 6-15 people attend each PERT call. If particular non-PERT specialists are needed, they are paged separately and are provided relevant case specifics.
In August 2014, PERT members implemented a multidisciplinary follow-up clinic for every patient associated with a PERT call to help improve the transition of care from inpatient to outpatient. The PERT specialists meet an hour before the clinic to discuss every patient and his/her treatment and decide short- and long-term follow-up goals and care. More than 180 patients have been seen in this clinic.
“The PERT concept is growing rapidly as a new paradigm to treat patients with PE,” says Dr. Rosovsky, who, along with the other members of the PERT executive committee, including Kenneth Rosenfield, MD; Richard Channick, MD; and Christopher Kabrhel, MD, MPH, has been instrumental in organizing a PERT Consortium. The consortium hosted its second annual meeting in June 2016 with more than 150 professionals from 90 medical institutions attending. Through this channel, Dr. Rosovsky and colleagues are collecting data on PERT patients seen not only at Mass General but also at 14 other PERT sites as a pilot study with the goal of devising better, evidence-based guidelines.
NOTE: Cardiovascular Landing Website Image: A large pulmonary embolism at the bifurcation of the pulmonary artery (saddle embolism). This is an edited version of the source image made for use in the "Anatomist" iOS and Android app and shared here under the terms of the source image's Share Alike Creative Commons license.
For more information, call 866-576-0690
Refer a patient to the Fireman Vascular Center