The Promise of Ventricular-Assist Devices (VADs)
In This Article
- New developments in ventricular-assist devices may address earlier problems
- VADs are becoming smaller and more durable, and associated risks are declining
- 50% of all VAD recipients survive to five years, despite estimated survival rates of less than 6 months
- Trials for the latest generation of VADs are under way
- Mass General data shows that VAD patients have a higher quality of life and improved heart failure
Ventricular circulatory assist devices now almost rival heart transplantation in terms of their impact on patient survival and quality of life. VADs are becoming smaller and more durable, and the associated risks are declining. Data from both the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) and Massachusetts General Hospital indicate that approximately half of all VAD recipients survive to five years, despite estimated survival rates of less than 6 months at the time of LVAD insertion.
Subscribe to the latest updates from Cardiovascular Advances in Motion
“Contrary to heart failure patients who received the earliest generation of pumps, today’s VAD recipients are doing quite well,” says David A. D’Alessandro, MD, surgical director, Heart Transplantation and Ventricular-Assist Devices at Mass General. The data also shows that VAD patients increasingly have a higher quality of life and improved heart failure classification by the New York Heart Association guidelines.
VAD Trials Underway
The Mass General Mechanical-Assist Team has an active and growing presence in providing VAD support for heart failure patients. “There was an almost 40% increment in our programmatic LVAD volume this year, in comparison to previous years, with patients successfully being bridged to cardiac transplantation and others who undergo VAD for destination therapy,” says Greg Lewis, MD, medical director, Cardiology ICU and Mechanical Circulatory Support Program at Mass General. Through October 2016, the team implanted 22 VADs and currently provides VAD support to more than 30 patients at home. In addition to other research efforts, the team also recently participated in the largest VAD trial of its kind: the MOMENTUM 3 study.
Approximately 1,800 patients with heart failure were randomized to either the latest generation VAD, the HeartMate 3 ™, or the HeartMate II ®, the current standard. Heart failure patients can now also enroll in the continuous access protocol at Mass General for the HeartMate 3, eliminating the need for patient randomization. According to Dr. D’Alessandro, “One of the Achilles’ heels of VADs has been gastrointestinal (GI) bleeding, which is a high driver of re-hospitalization. It appears to have a relationship with the loss of pulsatile blood flow.” The VAD team is hopeful that the HeartMate 3, which has reintroduced an artificial pulse, may have a positive impact on the incidence of GI bleeding. The new device, which has a modular design, would also negate a complete device exchange in the case of driveline replacement.
According to Dr. D’Alessandro, “One of the Achilles’ heels of VADs has been gastrointestinal (GI) bleeding, which is a high driver of re-hospitalization. It appears to have a relationship with the loss of pulsatile blood flow.” The VAD team is hopeful that the HeartMate 3, which has reintroduced an artificial pulse, may have a positive impact on the incidence of GI bleeding. The new device, which has a modular design, would also negate a complete device exchange in the case of driveline replacement.
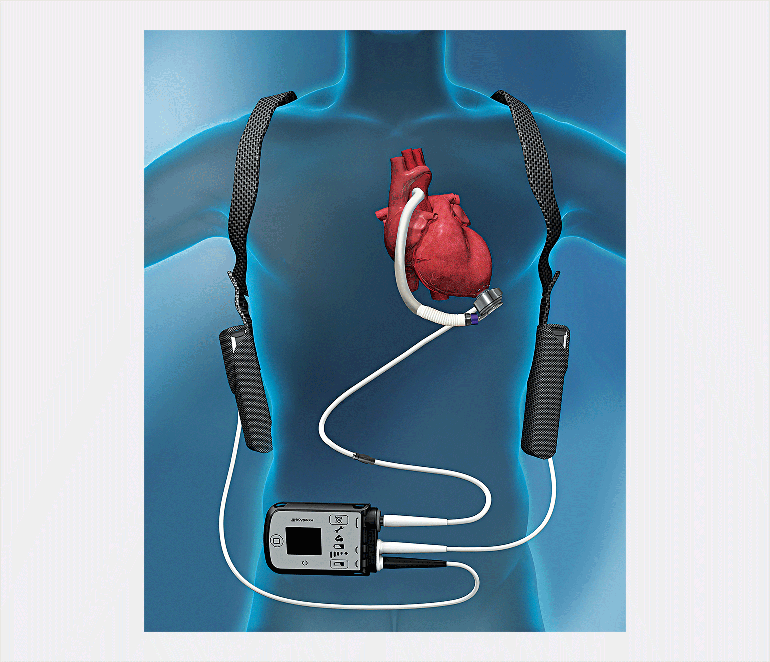
Fig. 1: The Heartmate3
is a mechanical circulatory support device in clinical trials. It restores blood flow for patients with advanced heart failure and offers improvements, such as an artificial pulse, over previous models.
24-Hour Care for VAD Recipients
The Mass General VAD team consists of physicians, nurse practitioners and nurses who provide 24-hour care for VAD recipients. Teams provide coordinated care whether VAD placement is a bridge to transplant or destination therapy for patients who do not meet transplant criteria. For VAD receipt there are no strict age exclusions, which are otherwise a consideration in organ transplantation. An appropriate VAD candidate is doing poorly on medications but has kidneys, lungs and liver that are still functioning well. “Patients need to be people that really want to be independent again, to make a commitment to something that could potentially drastically improve their quality of life,” says Dr. D’Alessandro.
According to Steph Ennis, NP, MSN, “Our patients are able to live better lives than they have been living for a long time.” Because heart failure is nearly always a condition of progressive decline, access to advanced therapies is essential to the best patient care. “It is critical to have access to every approved mechanical circulatory support device as well as the latest generation of devices within trials,” adds Dr. D’Alessandro. “This ensures that the patient has every available option and allows us to optimally tailor their care.” The Mass General Heart Failure and Cardiac Transplant Team also provides access to other electrophysiology devices and heart failure pharmacologic treatments, and participates in more than 15 active clinical trials.
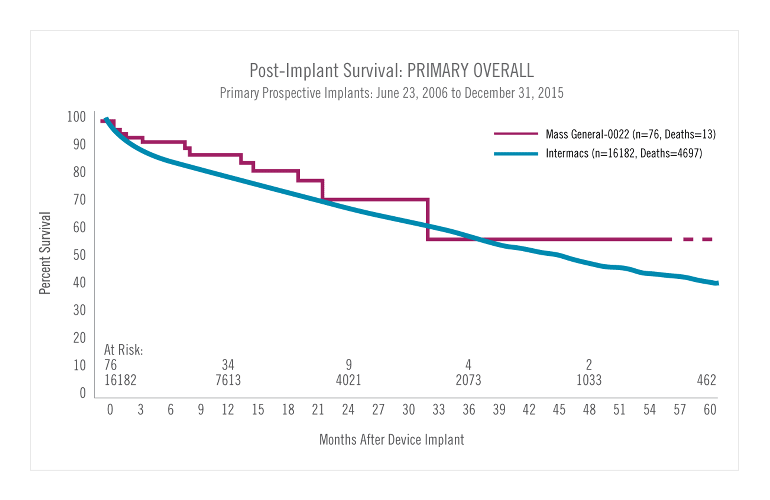
Fig. 2: Post-Vad Survival Rate:
The graph shows six-year patient survival data following VAD device implantation. Roughly half of implanted heart failure patients survive through five years.
For more information about the HeartMate 3 protocol, call 866-576-0690
Refer a patient to the Heart Center