The Role of Radiology in Identifying Intimate Partner Violence
In This Article
- Intimate partner violence (IPV) affects roughly 32 million people in the U.S., where more than one in three women have been a victim of rape, physical abuse or stalking by an intimate partner
- Many cases of IPV are not reported because of fear of reprisal or social stigma
- Radiologists can help identify patients who experience IPV by learning to recognize common imaging findings associated with it
- Common imaging findings for IPV include soft-tissue swelling, laceration, hematoma and infection
Intimate partner violence (IPV) is both a widespread public health concern and a significantly underreported problem. In the U.S., more than one in three women have been victims of rape, physical abuse or stalking by an intimate partner, according to the U.S. Centers for Disease Control and Prevention. Yet, for a number of possible reasons, including fear of reprisal by the partner and social stigma, victims often do not tell anyone about the abuse.
Subscribe to the latest updates from Radiology Advances in Motion
Radiologists can play an important role in identifying cases of IPV and helping ensure patients receive the help they need, even when they are seeking care for unrelated reasons. IPV is associated with a range of imaging findings. Radiologists can learn to recognize these symptoms to aid in diagnosis and treatment of IPV and help prevent further abuse. However, while a considerable amount of research has been devoted to the possible role of radiologists in identifying cases of child and elder abuse, relatively few studies have looked at radiology and IPV. (The relative focus on child and elder abuse is in part due to clinicians’ reporting responsibilities in these areas.) In a paper published online in February 2019 in the journal Radiology, a team of investigators at Brigham and Women’s Hospital and the Harvard T.H. Chan School of Public Health provides extensive guidance in recognizing imaging findings suggestive of IPV.
The Physical, Psychological and Economic Toll of Intimate Partner Violence
IPV is a serious public health concern impacting roughly 32 million people in the U.S. While IPV most often afflicts women, victims can also include men. Both heterosexual and same-sex relationships are affected by IPV. In addition to possible blunt force-related injuries, research has shown greater rates of asthma, irritable bowel syndrome, diabetes, chronic pain, memory loss, neurologic symptoms and poor reproductive health in victims of IPV, as well as a range of mental health concerns. Also, children exposed to IPV in the home are more likely to experience somatic symptoms, anxiety, depression, aggressive behavior and attention problems. IPV is also associated with significant economic costs. A 2007 study found that it is responsible for excess health care costs of approximately $19.3 million, each year, for every 100,000 women ages 18 to 64. A striking percentage of these costs is associated with emergency department care. An estimated 35% of all emergency department visits by women—and 21% of all injuries necessitating urgent surgery—are linked to IPV.
Because of fear of reprisal and social stigma, many victims may not report intimate partner violence during clinical encounters. Radiologists may be in a position to recognize possible cases of IPV before other health care providers based on imaging findings alone. Such early detection can be especially important because many victims will suffer repeated episodes of IPV, leading to subacute or chronic fractures or escalating violence. By identifying victims sooner, the health care team can refer them to appropriate support services—in accordance with established protocols to help ensure safety and confidentiality—and, by doing so, aid in preventing further injuries.
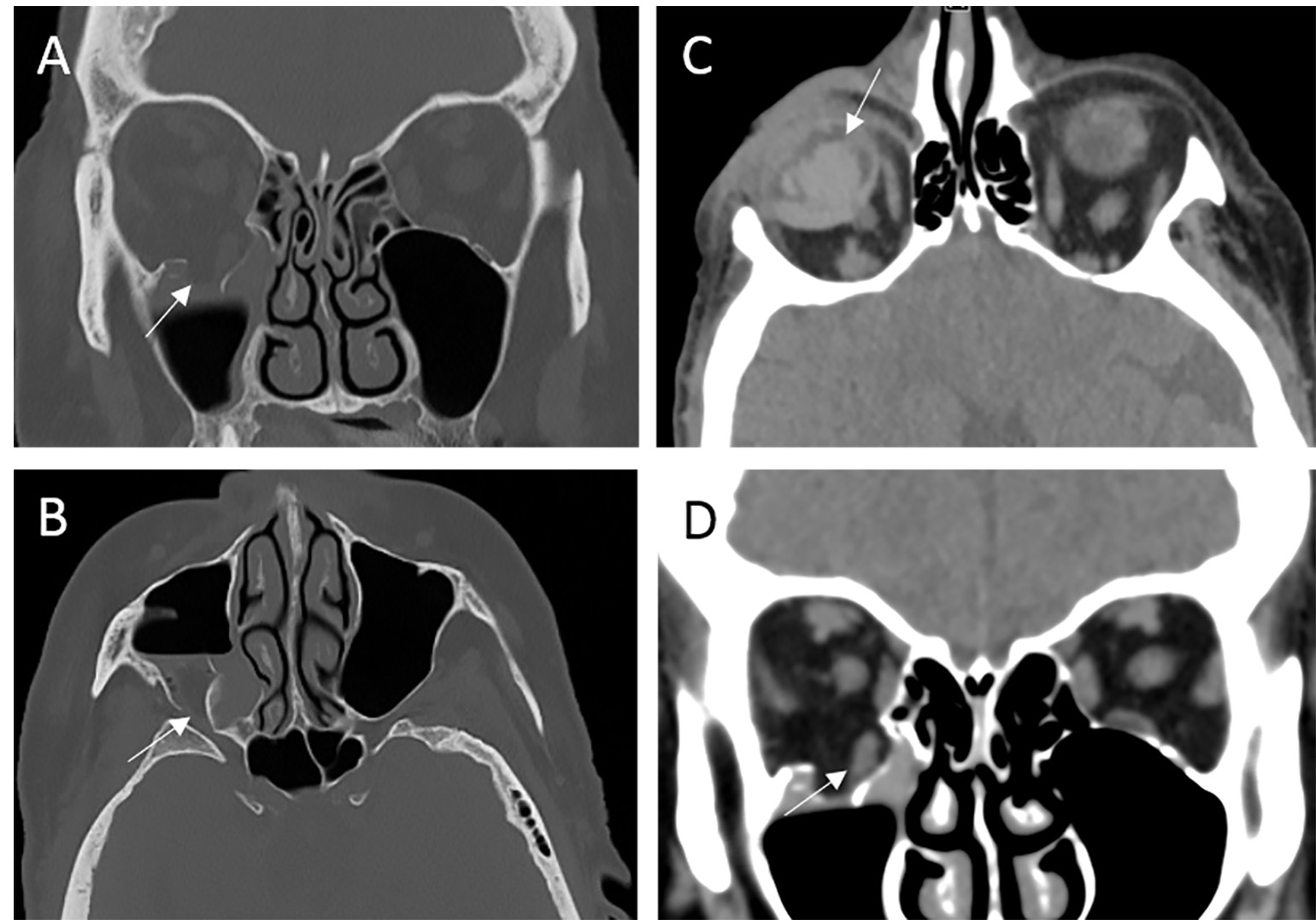
Figure 1
73-year-old female presenting after being punched by her husband found to have inferior blowout fracture of the right orbit (A), fracture of the lateral wall of the right maxillary sinus (B), and right vitreous hemorrhage (C). There is associated herniation of the right inferior rectus (D). Image courtesy of Elizabeth George, MD, Department of Radiology, Brigham and Women’s Hospital.
Common Imaging Findings in Intimate Partner Violence
In a 2019 published Radiology paper, the investigators sought to establish the imaging findings associated with IPV to help radiologists identify cases and work with other members of the clinical team to provide appropriate care. To this end, they retrospectively reviewed the medical records of 185 patients who had been referred to an IPV support program from the emergency department (ED) between January 2015 and October 2016 and compared them with records from a control group of 555 age- and sex-matched subjects. They also reviewed all imaging studies performed in the five years previous to the index ED visit. The study is important not only because it addresses an under-reported topic in the literature but also because it is among the first to include sociodemographic factors as well as imaging findings in its analysis.
The authors found that the mean age of the IPV victims was 34.1 years and that the majority of victims were female (96.2%) and African American, Hispanic or other nonwhite ethnicity (65.4%). The study confirmed an association between IPV and housing instability and psychiatric history. Finally, compared with the control group, a greater and statistically significant percentage of the IPV victims were pregnant at the time of the index ED visit (11.2%, as compared to 4.3%). Research has shown that violence during pregnancy can lead to obstetric complications, postpartum depression and maternal homicide. The authors of the Radiology paper also highlighted common imaging findings in IPV that radiologists can learn to recognize as possible markers of IPV. The most common findings for the IPV group for the five years prior to the index ED visit were soft-tissue swelling, laceration, hematoma and infection. (Other studies have used terms such as contusion of soft tissue or superficial bruising to describe similar findings.) Such injuries are often the result of direct trauma to the body.
The next most common finding was musculoskeletal injuries. Notably, while the majority of acute fractures in the control group were extremity fractures, which were likely the result of accidental trauma, a higher proportion of the patients in the IPV group experienced craniofacial fractures, suggesting non-accidental trauma. This finding corresponds to anecdotal evidence and other studies that indicate the areas of the head, neck and face are common targets in IPV.
Potential violence-related obstetric-gynecologic findings, including intrauterine growth restriction, sub-chorionic hematoma, failed pregnancy and retained products of conception, were associated with the highest odds of IPV. These findings tie in with existing literature suggesting a higher prevalence of IPV during pregnancy.
Another of the study’s findings warrants mention. More than one quarter of the patients in the IPV group (27%) reported a history of strangulation. While the imaging findings did not offer definitive evidence of strangulation-related injuries, which include soft-tissue, airway and vascular injuries in the neck, radiologists should be aware of the frequency of strangulation in IPV victims. Importantly, a history of strangulation has been shown to correlate with a seven-fold higher risk of future homicide, underscoring the critical role radiologists can play in evaluating these injuries using evidence-based imaging protocols.
Screening for Women at Risk for IPV in Breast Imaging Centers
In a paper published in the Journal of the American College of Radiology, in a special issue addressing health equity, Mass General researchers describe an additional avenue through which radiologists can help identify victims of IPV. With roughly 83 million women aged 40 to 74 in the U.S. receiving mammograms within the past two years, they write, breast imaging centers can play an instrumental role in screening for IPV. In the JACR study, they sought to determine the efficacy of an IPV screening assessment and referral program for women who come to the breast imaging center at Mass General for screening and diagnostic mammography.
Introduced in June 2016, this program seeks to identify women who may experience IPV by including the questions, "Do you feel safe at home?" and a follow-up "Do you feel safe in your relationship?" on the intake questionnaire. If they answer yes, they are provided with information about the HAVEN (Helping Abuse and Violence End Now) program at Mass General. HAVEN offers a range of advocacy and counseling services for victims of IPV, in English or Spanish or in other languages through interpreter services. The free and confidential program, which sees between 600 and 700 patients annually, ranging in age from 15 to 87 years, does not bill insurance or document visits in patients’ electronic health records, thus helping ensure the patients’ safety.
The study retrospectively reviewed data from the intake questionnaires from women presenting to outpatient breast imaging sites at Mass General between June 2016 and December 2017. Over the course of those 18 months, the researchers note, 71 women responded that they felt unsafe in their homes. While this number represented a relatively small percentage of the total number of respondents included in the study at less than 1%, the finding is consistent with reported estimates from other health care institutions that screen for IPV. Also, meta-analyses have shown that such screening efforts, even with relatively low estimates, nonetheless lead to improved identification of IPV victims.
The authors of the study note that including additional questions on intake questionnaires is one of a variety of possible tools available to radiologists to help screen for patients who either experience or are at risk for IPV. Others may be available soon. Another potential solution is to develop prediction systems to help identify women at risk for IPV either before or during their mammography appointments, enabling more targeted screening interventions for these women. Tools to increase patient awareness of IPV and its relationship to health and well-being could also be standard practice in radiology settings, especially in imaging specifically related to female patients.
Scheduling
The HAVEN program at Massachusetts General Hospital offers direct services to patients, employees and community members who have experienced IPV to help improve their health and safety. These services include safety planning, counseling, education, referral, legal consultation and court accompaniment. Advocates are available at the main campus of Mass General and at the Health Centers of Revere and Chelsea. HAVEN also provides consultation and training for health care providers regarding screening and best practices to support their patients and their housing, employment and financial circumstances. For more information or to schedule an appointment, please call the HAVEN main line at 617-724-0054 or the HAVEN director at 617-726-7674.
Reference
Bhole S, Bhole A and Harmath C (2014). The black and white truth about domestic violence. Emerg Radiol 21: 407– 412.
Learn more about HAVEN at Mass General
Visit the Department of Radiology at Mass General