Prone Position in the Non-intubated Patient
The FLARE Four
- There is widespread consensus on the benefit of prone positioning in the treatment of intubated patients with severe ARDS
- The distribution of stresses within lung tissue is more homogenous in the prone position
- If prone positioning is successful in lung recruitment, the resultant increases in aeration and oxygen tension should mitigate hypoxemic vasoconstriction
- If intubation is not feasible or is discordant with a patient’s goals and preferences, prone positioning in the non-intubated patient is likely safe and may be effective
Tonight's FLARE will address two questions:
Subscribe to the latest updates from FLARE Advances in Motion
- What is the effect of prone position in a non-intubated patient?
- Should it be considered in patients with severe COVID-19?
Introduction
There is widespread consensus on the benefit of prone positioning in the treatment of intubated patients with severe ARDS (Beitler et al., 2014; Fan et al., 2017; Guérin et al., 2013). In the setting of severe SARS-CoV-2 infection, some centers have also considered the use of prone positioning in the management of spontaneously breathing patients without invasive mechanical ventilation. In this FLARE, we discuss the physiologic rationale for prone positioning in ARDS and review the limited reports to date on “proning” non-intubated patients in the setting of COVID-19.
Before delving into the physiology, we want to emphasize that management of ARDS in COVID-19 should prioritize lung-protective ventilation. Clinical trials and subsequent meta-analyses have only established the therapeutic benefit of prone positioning in the context of low tidal volume mechanical ventilation (Beitler et al., 2014; Guérin et al., 2013). Thus, we do not suggest prone positioning in a non-intubated patient with ARDS if intubation appears otherwise indicated at that time (i.e. we do not recommend it as an alternative or rescue therapy to avoid intubation). Prone positioning could be considered if intubation is not feasible, is discordant with a patient’s goals and values, or is otherwise not indicated.
Physiologic Benefits Associated with Prone Position
Distribution of Transpulmonary Pressures, Recruitment and V/O Matching
A brief aside for non-pulmonary/critical care readers:
Transpulmonary pressure (PTP) is the pressure distending the lung, and is defined as: PTP = pressure at the airway opening - pleural pressure.
When monitoring mechanical ventilation in the ICU, we typically approximate PTP with the pressure at the airway opening (as displayed on the ventilator). However, as the equation above indicates, there are two components to the true distending pressure: (1) the pressure measured at the airway opening, and (2) the pleural pressure. To understand the important role of the pleural pressure, consider a trumpet player who generates an enormous alveolar pressure to force exhalation while playing a loud note. Her lungs nevertheless do not experience an enormous distending pressure (transpulmonary pressure) and burst. Why not? Because the high pressure inside the alveolus is balanced by an opposing pleural pressure, elevated due to the contraction of her abdominal and chest wall muscles.
Pleural pressure is not homogeneous across the lung surface. It is less negative in the dependent portion of the lung than in the non-dependent portion. This gradient results, in part, from dependent portions of the lung supporting the weight of the lung above. As a result, in the supine position, transpulmonary pressure is greater in the ventral (non-dependent) lung than in the dorsal (dependent) lung. In ARDS, this difference is intensified by the increased weight of edematous, injured tissue and consequent dorsal alveolar collapse (derecruitment). At the same time, the aerated ventral lung preferentially receives greater airflow and is at risk for overdistension (Figure 1).
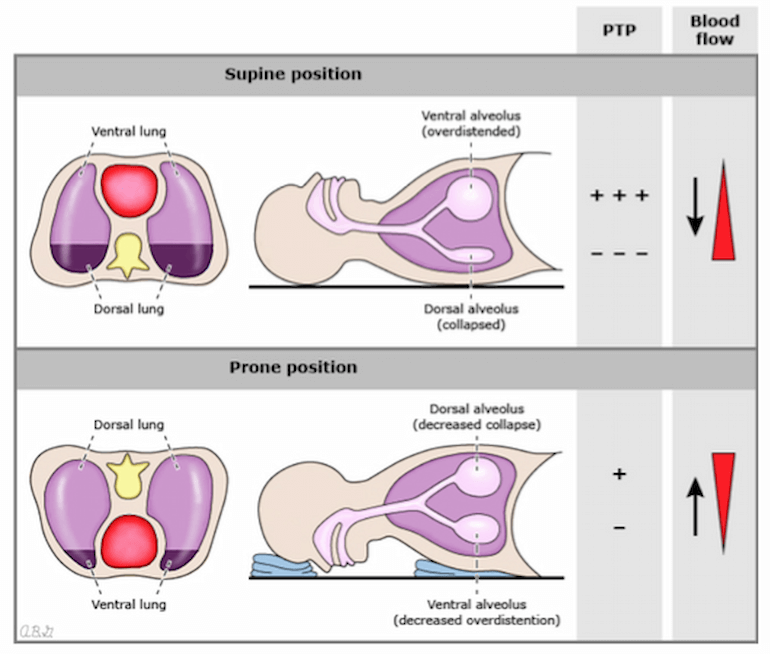
Figure 1
Regional decruitment, alveolar distension/collapse, transpulmonary pressure and blood flow in the supine and prone position. PTP= transpulmonary pressure. Image from A. Malhotra, UptoDate (Malhotra, 2019).
The problem of derecruitment is exacerbated in the supine position by the weight of the mediastinal contents resting on the lung, whereas in the prone position the mediastinum is supported by the sternum. Finally, the lung is not symmetric along the dorsal-ventral axis — there is a greater mass of tissue in the dorsal lung than the ventral lung. Therefore there is a greater amount of dependent lung in the supine position compared to the prone position. Thus proning results in dorsal recruitment, leading to a net increase in recruited lung and a decrease in overdistended lung. The anatomic asymmetry also results in improved V/Q matching in the prone position. Given that there are more alveoli and vessels in the dorsal lung, and therefore more blood flow to dorsal lung regardless of patient position, recruiting that region will result in a net decrease in shunt (perfusion without ventilation) (Bellani et al., 2009; Nyrén et al., 1999).
Finally, the distribution of stresses within lung tissue is more homogenous in the prone position. This is expected to mitigate the propagation of lung injury that is often associated with heterogeneous inflation of the injured lung (Liu et al., 1990).
Right Ventricular Function
If prone positioning is successful in lung recruitment, the resultant increases in aeration and oxygen tension should mitigate hypoxemic vasoconstriction. When these changes occur in the dorsal regions of the lung, which receive the majority of non-gravity dependent blood flow, pulmonary vascular resistance (and thus RV afterload) decrease (Jozwiak et al., 2013). Thus, prone position may improve RV function.
Application to Non-intubated Patients in the Setting of COVID-19
The above physiologic rationale for prone positioning emphasizes the benefit of recruitment of dorsal lung regions and redistribution of transpulmonary forces. These changes may be expected to also occur in the proned non-intubated patient (especially if NIPPV is provided) though we lack direct clinical evidence to better inform this approach. Of note, low tidal volumes cannot be guaranteed in the spontaneously breathing, non-sedated patient, which may potentially lead to injurious inflation patterns due to increased transpulmonary pressures (Yoshia et al., 2017).
Two descriptive reports suggest that non-intubated prone positioning was pursued for the treatment of ARDS in the setting of COVID-19 in China. In these reports, patients were prone for ~2 hour periods, with multiple sessions each day, either receiving HFNC or NIPPV (Ding et al., 2020; Sun et al., 2020). Anecdotes from colleagues across the United States suggest the successful use of this approach as well.
Conclusion
Intubation and lung-protective ventilation remain the cornerstone of ARDS management, including the management of COVID-19-associated ARDS. If intubation is not feasible or is discordant with a patient’s goals and preferences (e.g. DNI), prone positioning in the non-intubated patient is likely safe and may be effective based on the above physiologic rationale. We recommend assessment of changes in oxygenation after prone positioning to assess the efficacy and close monitoring as would be performed in an intubated patient.
References
- Beitler, J.R., Shaefi, S., Montesi, S.B., Devlin, A., Loring, S.H., Talmor, D., and Malhotra, A. (2014). Prone positioning reduces mortality from acute respiratory distress syndrome in the low tidal volume era: a meta-analysis. Intensive Care Med. 40, 332–341.
- Bellani, G., Messa, C., Guerra, L., Spagnolli, E., Foti, G., Patroniti, N., Fumagalli, R., Musch, G., Fazio, F., and Pesenti, A. (2009). Lungs of patients with acute respiratory distress syndrome show diffuse inflammation in normally aerated regions: a [18F]-fluoro-2-deoxy-D-glucose PET/CT study. Crit. Care Med. 37, 2216–2222.
- Ding, L., Wang, L., Ma, W., and He, H. (2020). Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit. Care 24, 28.
- Fan, E., Del Sorbo, L., Goligher, E.C., Hodgson, C.L., Munshi, L., Walkey, A.J., Adhikari, N.K.J., Amato, M.B.P., Branson, R., Brower, R.G., et al. (2017). An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome. American Journal of Respiratory and Critical Care Medicine 195, 1253–1263.
- Guérin, C., Reignier, J., Richard, J.-C., Beuret, P., Gacouin, A., Boulain, T., Mercier, E., Badet, M., Mercat, A., Baudin, O., et al. (2013). Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 368, 2159–2168.
- Jozwiak, M., Teboul, J.-L., Anguel, N., Persichini, R., Silva, S., Chemla, D., Richard, C., and Monnet, X. (2013). Beneficial hemodynamic effects of prone positioning in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 188, 1428–1433.
- Liu, S., Margulies, S.S., and Wilson, T.A. (1990). Deformation of the dog lung in the chest wall. J. Appl. Physiol. 68, 1979–1987.
- Malhotra, A. (2019). Prone ventilation for adult patients with acute respiratory distress syndrome. In UpToDate, P.E. Parsons, and G. Finlay, eds. (Waltham, MA: UpToDate),.
- Nyrén, S., Mure, M., Jacobsson, H., Larsson, S.A., and Lindahl, S.G. (1999). Pulmonary perfusion is more uniform in the prone than in the supine position: scintigraphy in healthy humans. J. Appl. Physiol. 86, 1135–1141.
- Sun, Q., Qiu, H., Huang, M., and Yang, Y. (2020). Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann. Intensive Care 10, 33.
- Yoshida T, Nakahashi S, Nakamura MAM, et al. Volume-controlled Ventilation Does Not Prevent Injurious Inflation during Spontaneous Effort. Am J Respir Crit Care Med. 2017;196(5):590–601.
View all COVID-19 updates
Learn about research in the Division of Pulmonary and Critical Care Medicine