HPV-Associated Head and Neck Cancer Blood Test Shows Promise as Test to Replace Tissue Biopsy
Key findings
- Human papillomavirus (HPV)-head and neck cancer has been rapidly increasing in incidence, surpassing cervical cancer as the most common HPV-associated malignancy in the United States
- A liquid biopsy test developed at Mass Eye and Ear was more accurate, potentially faster and less costly than standard clinical workup for diagnosing HPV-associated head and neck cancer
- 140 individuals were enrolled in a prospective study that reported these results: 70 individuals presenting with a new, assumed diagnosis of HPV-associated head and neck cancer and 70 control subjects from Mass Eye and Ear and Massachusetts General Hospital
- The study is the first time a non-invasive approach has been tested as a reliable diagnostic tool at the time of presentation for HPV-associated head and neck cancer
Researchers at Mass Eye and Ear and Massachusetts General Hospital have developed a blood test for head and neck cancer associated with the human papilloma virus (HPV) that was shown to be more accurate, possibly faster and less expensive than conventional testing methods.
Subscribe to the latest updates from Otolaryngology Advances in Motion
In a study published in Clinical Cancer Research, lead author Daniel Faden, MD, FACS, a head and neck surgical oncologist at Mass Eye and Ear, reported that the new blood test, or liquid biopsy, was more than 98% accurate and cost 38% less than standard methods.
The study used diagnostic modeling to determine whether the biopsy could generate a diagnosis faster than conventional, invasive biopsies. From these models, the researchers determined that the biopsy could potentially obtain a diagnosis 26 days faster on average than a conventional tissue biopsy.
When researchers combined the liquid biopsy with findings from routine imaging and physical exam to create a fully non-invasive diagnostic approach, diagnostic accuracy remained significantly superior to standard approaches.
HPV-associated Head and Neck Cancer Epidemic
Head and neck cancer is a common cancer in the United States and worldwide, especially in adults aged 50 years and older. Rates of one type of head and neck cancer affecting the area of the throat behind the mouth, the oropharynx, have dramatically risen in recent years, driven by HPV, which now accounts for roughly 75% of all cases of oropharyngeal cancers in the United States.
Diagnosing a patient with HPV-associated head and neck cancer through conventional methods has limitations. Tests, such as surgical biopsy, are invasive, and others, such as fine needle aspiration, may require repeat biopsies. Further, surgical biopsies, CT and PET imaging and physical exams can only detect cancers once they have grown to millions of cells and are "visible."
When caught early, these cancers can be removed by surgery or treated with radiation. However, once the cancer grows, and spreads through the lymph nodes, treatment becomes more of a challenge and patients often suffer life-long from the side effects of treatment.
Detecting DNA Fragments of HPV in Blood
Liquid biopsy provides a less-invasive method for detecting cancers. Recent studies have shown that liquid biopsies can be used to monitor for recurrence in HPV-associated head and neck cancers. Dr. Faden's new study takes the next step and asks if a highly accurate blood test, combined with routine imaging and physical exam findings, could eliminate the need for an invasive tissue biopsy all together.
The custom liquid biopsy developed and applied in this study detects microscopic levels of HPV DNA floating in the blood. The test builds on the expanding field of cell-free DNA in cancer screening and diagnostics research. Cell-free DNA are fragments of DNA that break off cancer cells and are released into the bloodstream. While cell-free DNA can be difficult to detect for some cancers, HPV-associated cancers offer a major advantage because they release HPV DNA, which is only found in the bloodstream with the presence of an HPV-associated cancer.
Diagnosing HPV-associated Head and Cancer Accurately and Quickly
In the study, researchers prospectively enrolled 70 individuals presenting with a new, assumed diagnosis of HPV-associated head and neck cancer and 70 control subjects from Mass Eye and Ear and Massachusetts General Hospital. All underwent routine physical exam and imaging.
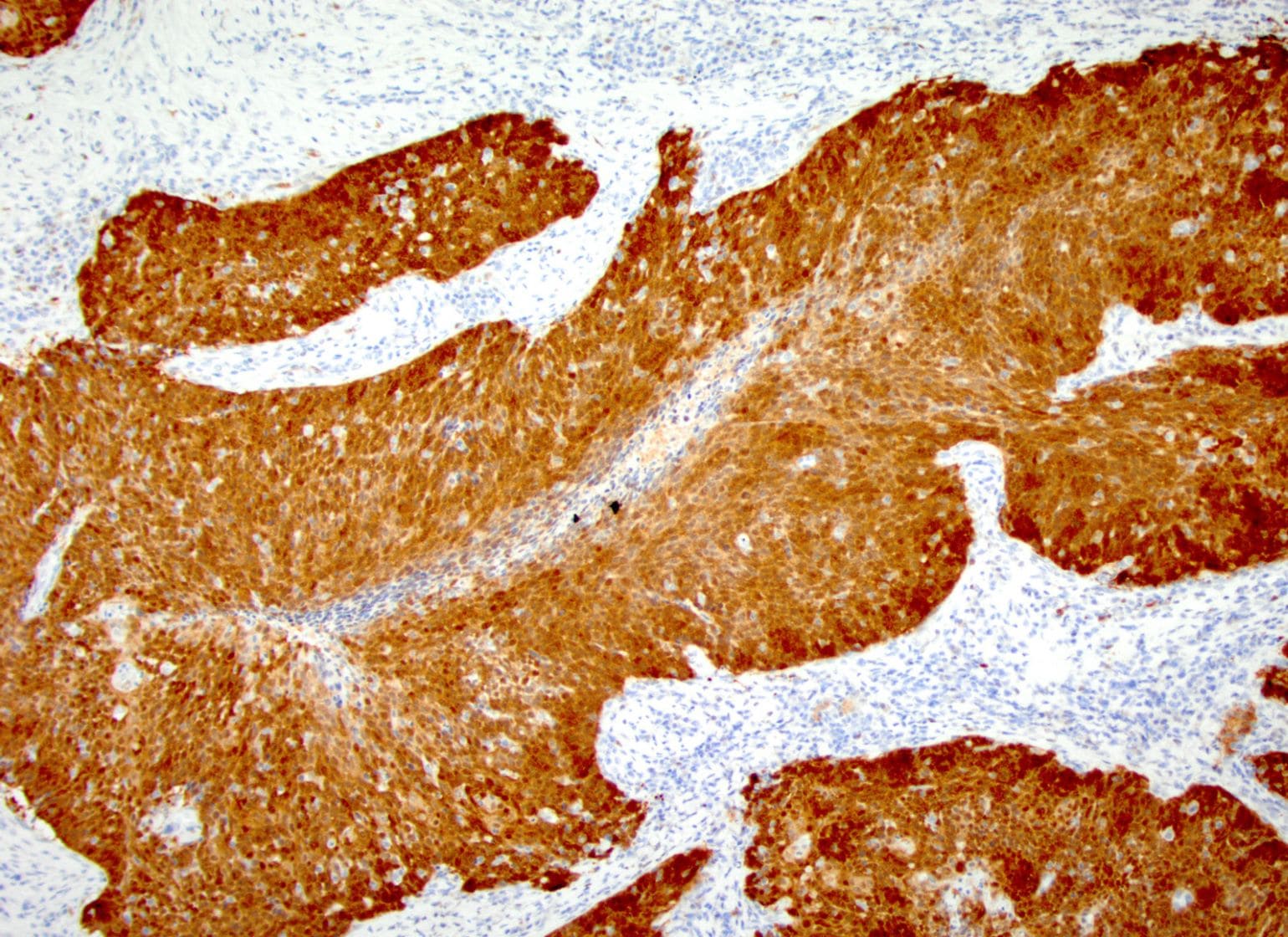
Figure 1
P16 Immunohistochemical staining of an HPV-associated tonsil cancer from a patient enrolled in a prospective study of circulating tumor HPV DNA published in Clinical Cancer Research. Image courtesy of Dr. Faden.
They found liquid biopsy was significantly more accurate than the standard of care, with 98.4% sensitivity for identifying a positive result and 98.6% specificity for detecting a negative result. When liquid biopsy was combined with routine imaging and physical exam findings, diagnostic sensitivity was 95.1% and diagnostic specificity was 98.6%. The study also found that the average time from the first presentation to a health care provider to diagnosis would be 63% less than typical methods. Costs of the liquid biopsy were also found to likely be significantly lower than conventional methods with an average estimated savings of over $6,000 per patient.
As a result of these findings, a Mass Eye and Ear team, led by Dr. Faden and Jeremy D. Richmon, MD, director of Head and Neck Robotic Surgery, has designed a clinical trial which will attempt to validate findings from this study, as well as use the liquid biopsy to make real-time decisions for patients during treatment in an attempt to personalize care.
view original journal article Subscription may be required
Learn more about the Department of Otolaryngology–Head and Neck Surgery at Mass Eye and Ear
Refer a patient to Mass Eye and Ear/Mass General Brigham