New Tools Assess Risk of Motor Deficit, Short-term Mortality in Patients with Spinal Epidural Abscess
Key findings
- Using 24 years of data on patients with spinal epidural abscess, Massachusetts General Hospital researchers identified eight independent predictors of pretreatment motor deficit and eight independent predictors of 90-day mortality
- Pretreatment motor deficit itself was one of the risk factors for 90-day mortality
- The researchers developed nomograms to help clinicians quantify the probability of motor deficit and mortality for individual patients
- Diagnosis and treatment of spinal epidural abscess before motor weakness develops may improve survival
Subscribe to the latest updates from Orthopaedics Advances in Motion
In patients with spinal epidural abscess, purulent expansion within the confined epidural space may cause spinal cord injury, with subsequent paralysis or death. The choice of operative versus nonoperative management largely depends on whether the patient has a motor deficit or is in imminent danger of developing one, but few studies have identified predictors of motor deficit or mortality.
Orthopedic surgeons at Massachusetts General Hospital including Department of Orthopaedics Chief Mitchel B. Harris, MD, and Orthopaedic Spine Center Chief Joseph H. Schwab, MD, conducted a study to identify independent predictors pretreatment motor deficits or mortality and developed nomograms to help clinicians quantify the probability of developing one. A nomogram is used to predict outcomes for individual patients, rather than for risk groups, by assigning points to a patient and disease characteristics. They report their work in Journal of Bone and Joint Surgery.
The research team searched the records of 1053 adults who were diagnosed with a spinal epidural abscess at Mass General between 1993 and 2016. In these records, the median age was 59 years, 61% were male, and 23% had comorbid diabetes mellitus, an established risk factor for a spinal epidural abscess. The presentation included pretreatment motor weakness in 34% of the patients, sensory changes in 28%, bladder dysfunction in 11% and bowel dysfunction in 4%. The inpatient mortality rate was 7%, and an additional 6% of patients died within 90 days after discharge.
Multivariable analysis yielded the following results:
- Positive predictors of pretreatment motor weakness: diabetes mellitus, sensory changes, urinary incontinence/retention, fecal incontinence/retention, abscess located proximal to the conus medullaris, abscess located in multiple locations relative to the thecal sac and white blood cell count >12 x 109 cells/L
- Protective against pretreatment motor weakness: location of the abscess exclusively dorsal to the thecal sac
- Positive predictors of 90-day mortality: age >65 years, diabetes mellitus, active malignancy, receiving regular hemodialysis, pre-treatment motor deficit, concurrent endocarditis and white blood cell count >15 x 109 cells/L
- Protective against 90-day mortality: Duration of symptoms >2 weeks
- The predictors suggest risk factors for the whole population, but they are not prognostic for any given individual. Therefore, the researchers constructed nomograms by assigning points to each predictor.
By totaling the points for each patient (Figure 1), then consulting the following equation and Figure 2, clinicians can calculate each patient's probability of pre-treatment motor weakness or 90-day mortality:
Probability = econstant + (total points x points coefficient)/1 + econstant + (total points x points coefficient)
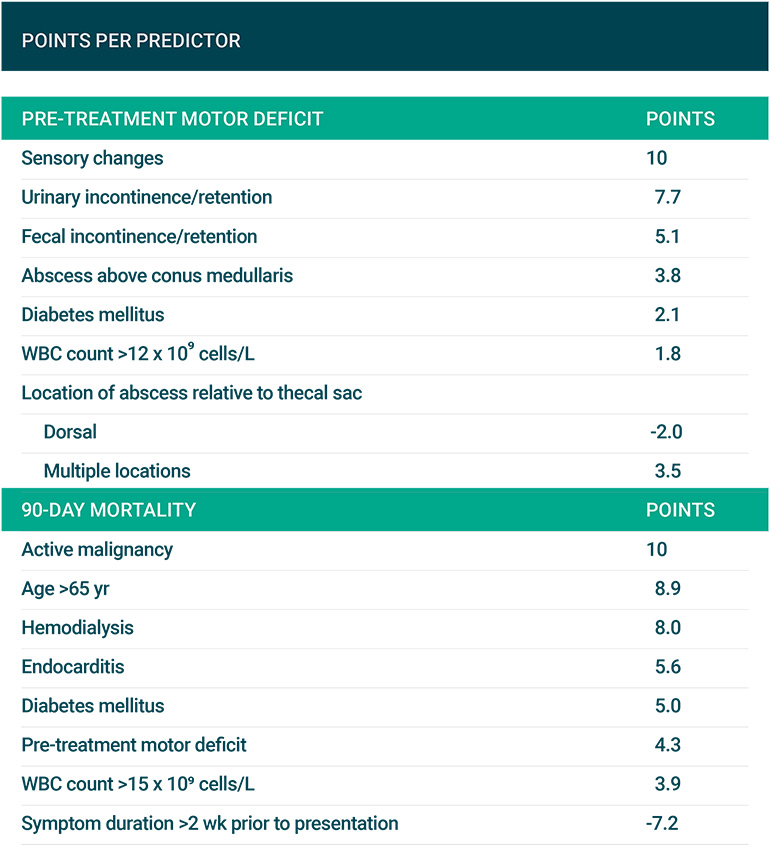
Figure 1
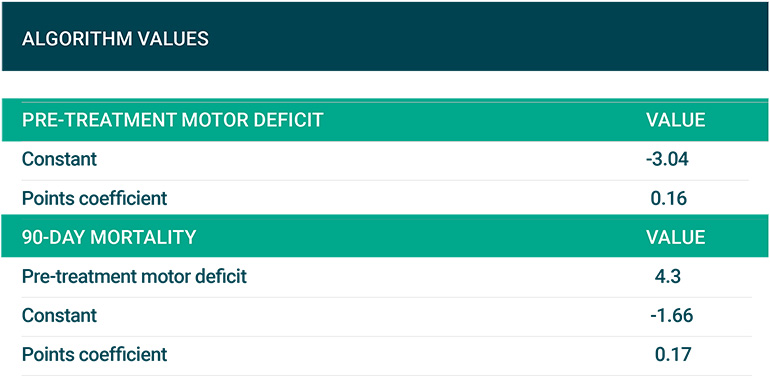
Figure 2
The researchers call particular attention to their finding that pretreatment motor deficit is a risk factor for 90-day mortality. This implies that early diagnosis of a spinal epidural abscess is important since a motor deficit is generally a late manifestation. For patients who are neurologically intact, but at high risk of motor deterioration, Dr. Schwab's team recommends treatment without delay, to avoid residual motor weakness and improve survival.
view original journal article Subscription may be required
About Mass General's Orthopaedic Spine Center
Refer a patient to the Orthopaedic Spine Center