Latarjet Procedure Helps Few Elite Football Players
Key findings
- Of 2,617 football players reviewed, <1% had undergone the Latarjet procedure
- In the 13 players with a history of Latarjet surgery, 46% had hardware complications
- In the 8 players with a CT image available, 62% had moderate to nearly complete bone resorption
The Latarjet procedure is advocated as the treatment of choice for recurrent anterior shoulder instability with significant glenoid bone loss. In the National Football League (NFL), nearly 5% of incoming players report undergoing a shoulder stabilization procedure, but little was known about outcomes of Latarjet surgery in elite football players.
Subscribe to the latest updates from Orthopaedics Advances in Motion
In a retrospective study published in The Orthopaedic Journal of Sports Medicine, researchers found that only a small percentage of prospective NFL players had undergone a Latarjet procedure, with high rates of postoperative complications and degenerative changes of the glenohumeral joint.
Mark D. Price, MD, PhD, an orthopedic surgeon with the Sports Medicine Center at Massachusetts General Hospital, and colleagues reviewed all participants at the NFL Scouting Combine from 2009 through 2016. At the combine, shoulder stabilization surgery is the fourth most common procedure among players. Combine participants were selected for the study if their written history suggested a previous Latarjet procedure or if dictation notes on previous radiographic imaging mentioned hardware near the glenohumeral joint. In addition, data were analyzed from standard imaging studies performed at the combine. No clinical examination findings were collected.
Of 2,617 football players reviewed, only 13 (<1%) had a history of Latarjet surgery. Of these, seven had undergone the procedure as the primary treatment of recurrent instability, five players had one prior surgery and one player had two prior surgeries. Seven players had 2-screw constructs, and the other six players had one screw for fixation of the coracoid bone block.
Hardware complications were observed in six of the 13 players (46%). These included broken screws in two players, bent screws in two, and screw pullout in three. All 13 players had radiographic evidence of degenerative changes of the humeral head and/or the glenoid, although these changes were mild in ten players (77%). The researchers speculate that the degeneration may be attributable to recurrent instability episodes before or after the Latarjet procedure.
Eight of the 13 players who had Latarjet surgery had subsequently undergone computed tomography (CT). All 8 of them had evidence of bony resorption of the bone block. Three of the 8 (38%) showed evidence of minimal resorption (<25%), but in the others the resorption was moderate to nearly complete resorption. In two of the eight players, CT showed essentially no bony bridging to the native glenoid, and only one player had 100% complete bridging.
Seven of the 13 players with a history of a Latarjet procedure were ultimately drafted into the NFL, but none participated in more than half of their eligible plays during their rookie season (Figure 1). Therefore, the researchers were unable to draw conclusions about the effect of Latarjet on these players’ performance. Still, they consider their findings useful for NFL team physicians in counseling incoming players who have undergone the Latarjet surgery.
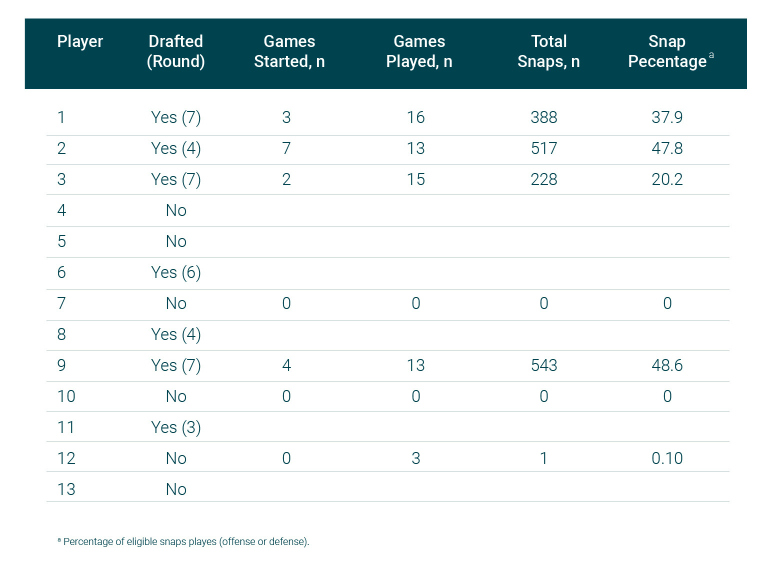
Figure 1: Volume of play measures during the players’ rookie season
view original journal article Subscription may be required
Learn more about the Sports Medicine Center at Mass General