Review: Telemedicine for Diagnosis and Management of Age-Related Macular Degeneration
Key findings
- A number of studies have demonstrated that ophthalmic lesions characteristic of age-related macular degeneration (AMD) can be detected remotely by various forms of retinal imaging, Amsler grid testing, and preferential hyperacuity perimetry
- Telemedical care of patients with AMD can include having in-person imaging evaluated remotely by a retina specialist, remote consultation between subspecialists and comprehensive ophthalmologists, and home-based monitoring of patients with high-risk AMD
- Each model of care shows promise for detecting exudative AMD in at-risk populations and ensuring patient access to subspecialists
- Additional advances in retinal imaging and testing, including optical coherence tomography (OCT) angiography and automated home-based OCT, are expected to improve the quality of remote evaluation of patients with AMD
Even before the COVID-19 pandemic, telemedicine was used to screen, diagnose, and manage age-related macular degeneration (AMD).
Subscribe to the latest updates from Ophthalmology Advances in Motion
John B. Miller, MD, director of Retinal Imaging at Mass Eye and Ear/Mass General Hospital, and Grayson W. Armstrong, MD, MPH, director of the Ophthalmology Emergency Service at Mass Eye and Ear, recently reviewed the latest research. In the Journal of Clinical Medicine, they discuss current telemedicine applications for the care of patients with AMD and potential future use cases.

Figure 1
A color fundus photograph of a patient's retina with age-related macular degeneration (AMD). Image courtesy of Grayson W. Armstrong, MD.
Telemedicine for Diagnosing AMD
Several studies have demonstrated that ophthalmic lesions characteristic of AMD can be detected remotely by:
- Non-stereoscopic two-dimensional fundus images when compared with stereoscopic photos
- Non-stereoscopic mydriatic color fundus photographs when compared with in-person examination and fluorescein angiography
- Optical coherence tomography (OCT) alone or with color fundus photographs, including when obtained by non-ophthalmologists
- Non-imaging-based evaluations such as Amsler grid testing and preferential hyperacuity perimetry
Further advances in retinal imaging and testing, including OCT angiography, may improve the quality of remote telemedical evaluation of AMD.
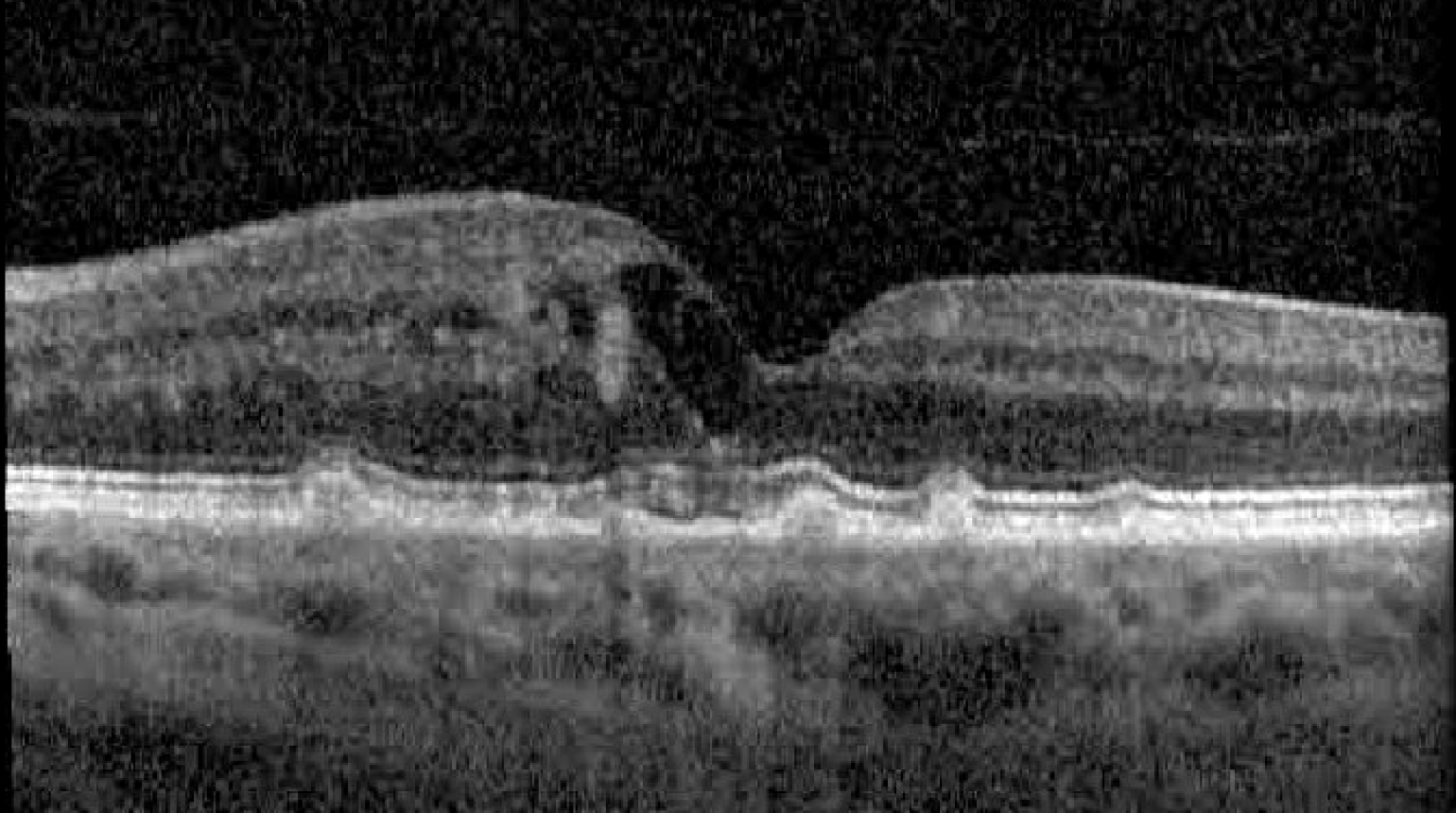
Figure 2
An image of a patient's retina with age-related macular degeneration (AMD) captured using optical coherence tomography (OCT). Image courtesy of Grayson W. Armstrong, MD.
Telemedicine for Managing AMD
The use of telemedicine for managing patients with known AMD has already been evaluated in randomized, controlled trials. In one trial reported in JAMA Ophthalmology, patients with stable AMD or suspected neovascular AMD were randomized to an in-person visit with a retina specialist or a comprehensive ophthalmologist.
In patients randomized to be cared for by a comprehensive ophthalmologist, visual acuity and intraocular pressure were measured, and color fundus photographs and macular OCT images were obtained. They stored the information in an online database for remote review by a retina specialist, who determined whether an in-person visit for an intravitreal injection was needed.
The results showed that the telemedicine group had longer referral-to-diagnosis times for new-onset exudative AMD and longer detection-to-treatment times for recurrent exudative AMD. However, visual acuity was similar in the two groups at the end of the study, and patient satisfaction was similarly high.
Implementing Telemedicine for AMD
There are multiple examples of successful system-wide implementation of telemedical care for AMD, including:
- American Journal of Ophthalmology: At the Mayo Clinic Rochester, patients with exudative AMD were initially treated by a retinal specialist, then by a local ophthalmologist who could consult the specialist electronically. In a two-year retrospective study, 200 consultations were placed for 59 patients. Only 14 consultations (7%) did not comply with the specialist's recommendations, mainly due to scheduling errors or missed appointments
- Journal of Telemedicine and Telecare: In Italy, 94 comprehensive ophthalmologists were connected electronically to 20 retina specialists. Compared with 318 patients who received usual care over the previous three months, 360 patients enrolled in the network for three months had significantly reduced time to therapy and significantly greater improvement in visual acuity
Home-based Monitoring of AMD
Multiple devices are being studied for home-based detection and monitoring of high-risk AMD, including:
- Fundus photography
- Automated macular visual field and preferential hyperacuity perimetry testing (e.g., the ForeseeHome device, Notal Vision Ltd., Tel Aviv, Israel)
- Prototypes of compact automated OCT devices
Thus, there's considerable promise for better provision of care to patients with AMD who have limited access to health care. This is especially important during the continuing COVID-19 pandemic, where an in-person evaluation of patients at high risk of vision loss is not always safe or feasible.
view original journal article Subscription may be required
Learn more about the Department of Ophthalmology at Mass Eye and Ear/Mass General
Refer a patient to Mass Eye and Ear/Mass General