Mass Eye and Ear Ophthalmology: Celebrating 200 Years of Excellence in Patient Care, Research, and Education
In This Article
- This year, Mass Eye and Ear is celebrating its 200th anniversary
- Over the past 200 years, Mass Eye and Ear researchers have been pioneers in many facets of ophthalmology, such as cornea research, retinal disease, proton beam irradiation, photodynamic therapy, optical coherence tomography, and much more
- In this article, we highlight some of the ophthalmology department’s most significant achievements in patient care, research, and education
Figure 1
A drawing of the first Mass Eye and Ear building on Charles Street, then known as the Massachusetts Charitable Eye and Ear Infirmary, in 1850.
This year, Mass Eye and Ear is celebrating its 200th anniversary. In the coming months, we will be sharing special stories and hosting a series of events, programs, and exhibits. To kick things off, we are highlighting some of the ophthalmology department’s most significant achievements below.
More than 80 Years of Excellence in Glaucoma Care, Teaching, and Research
Figure 2
Dr. Paul Chandler in the laboratory in an undated photo (left) and Dr. Morton Grant in 1970 (right).
In 1940, Paul A. Chandler, MD, who would go on to become a national leader in the diagnosis and management of glaucoma, joined the clinical staff at Mass Eye and Ear, where he developed a busy glaucoma referral practice.
In 1943, W. Morton Grant, MD, joined the Howe Laboratory at Mass Eye and Ear, and quickly became Dr. Chandler’s most frequent research collaborator. In 1955, they officially founded the Glaucoma Service (then known as the Glaucoma Consultation Service), and Dr. Grant served as its second director, succeeding Robert Trotter, MD. Together, the two friends and colleagues helped transform both the clinical and investigative disciplines of glaucoma.

Figure 3
Drs. Morton Grant (left) and Paul Chandler (right) at one of their weekly lunch meetings. Photo Credit: Marshall Cyrlin.
Drs. Chandler and Grant were also highly respected educators and mentors, dedicated to teaching the next generation of glaucoma specialists. When they met weekly for lunch to discuss interesting glaucoma cases and problems, they encouraged trainees to bring their own bagged lunch and join them for the informal discussions. In 1982, fellows who trained under the pair founded The Chandler-Grant Society to carry on their legacy. One such trainee was the late David Epstein, MD, who would go on to become one of the most influential leaders in glaucoma and glaucoma research in the modern era. Dr. Epstein, who went on to lead the Glaucoma Service after Dr. Grant, believed learning directly from the patient’s presentation, investigating first in the clinic, but if that didn’t solve the issue, taking the question to the laboratory to determine mechanism and treatment. David Epstein was a true student of Drs. Chandler and Grant.
Figure 4
Dr. Janey Wiggs working in the laboratory in 1993 (left) and in the laboratory in 2015 (right).
In 2021, working with international collaborators from more than 10 different countries, medical geneticist and glaucoma specialist Janey Wiggs, MD, PhD, identified over 120 novel genetic risk factors for various forms of glaucoma, including adult-onset primary open-angle glaucoma, pseudoexfoliation glaucoma, juvenile open angle glaucoma, and others. “This study, the largest of its kind, may help lead to the discovery of new biological pathways in glaucoma, and new treatment targets,” explained Dr. Wiggs, associate chief, Ophthalmology Clinical Research at Mass Eye and Ear and the Paul Austin Chandler professor of Ophthalmology at Harvard Medical School.
Charles L. Schepens, MD: Retina Pioneer and Innovator
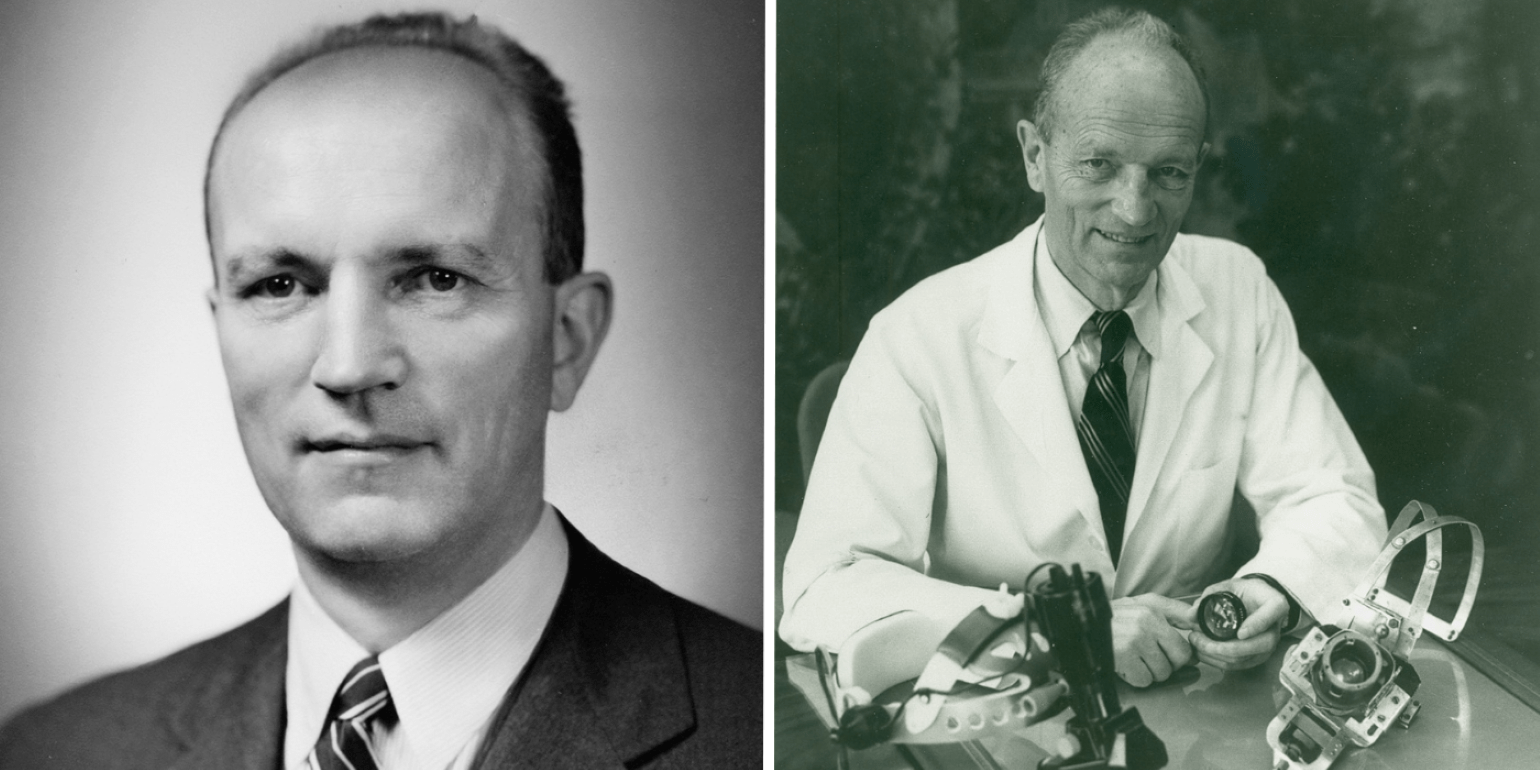
Figure 5
Dr. Charles Schepens pictured in the late 1940s (left) and with the binocular ophthalmoscope he developed in 1945 (right).
In 1947, Charles L. Schepens, MD, joined Mass Eye and Ear, and soon after established the world’s first retina service and retinal disease fellowship program. Since then, the Retina Service has grown to be one of the largest in the country. Our retinal researchers and clinician scientists have been at the forefront of the most transformative advances in retinal care, including photodynamic therapy, the first FDA-approved pharmacologic treatment for wet (neovascular) age-related macular degeneration (AMD), and anti-VEGF therapy for AMD, diabetic retinopathy, retinal vein occlusion and other retinal disorders, which are described further below. Today, our Retina Service continues to provide the most advanced medical and surgical treatments for retinal disorders and access to cutting-edge clinical trials.
Dr. Schepens is widely known as the father of modern retinal surgery. He pioneered many surgical procedures, especially scleral buckle techniques. He also developed numerous ophthalmic instruments, including the binocular indirect ophthalmoscope, the small pupil ophthalmoscope, the scanning laser ophthalmoscope, and a universal intraocular laser. His devices and surgical techniques have been credited with raising the success rate of retinal reattachment surgery from 40% to 90%.
Mass Eye and Ear retinal surgeon Hal Mackenzie Freeman, MD, continued Dr. Schepens legacy of pioneering retinal surgery procedures. In 1965, Dr. Freeman published a paper with Dr. Schepens on an inverted operating table they designed to fix giant retinal tears. This table suspended patients face down above the surgeon and allowed for gravity to unfold the giant retinal tear, thus making it operable for the surgeon. The prototype of the giant retinal tear operating table is now at the Smithsonian Institute in Washington.
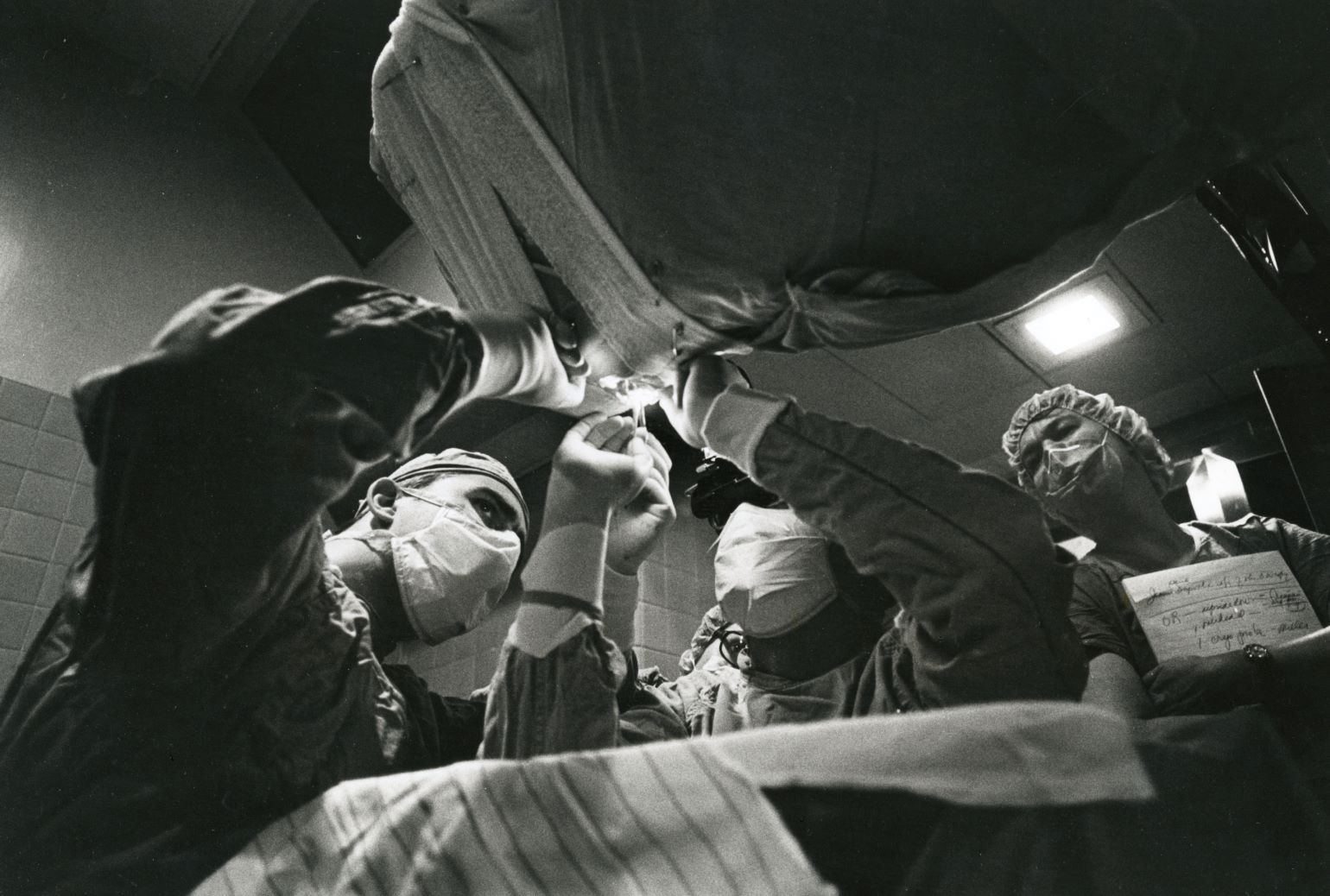
Figure 6
Retinal surgeons operate on a patient using the inverted operating table designed by Drs. Hal Freeman and Charles Schepens. Date of photo unknown.
Claes H. Dohlman, MD, PhD: Cornea Research Pioneer and Visionary
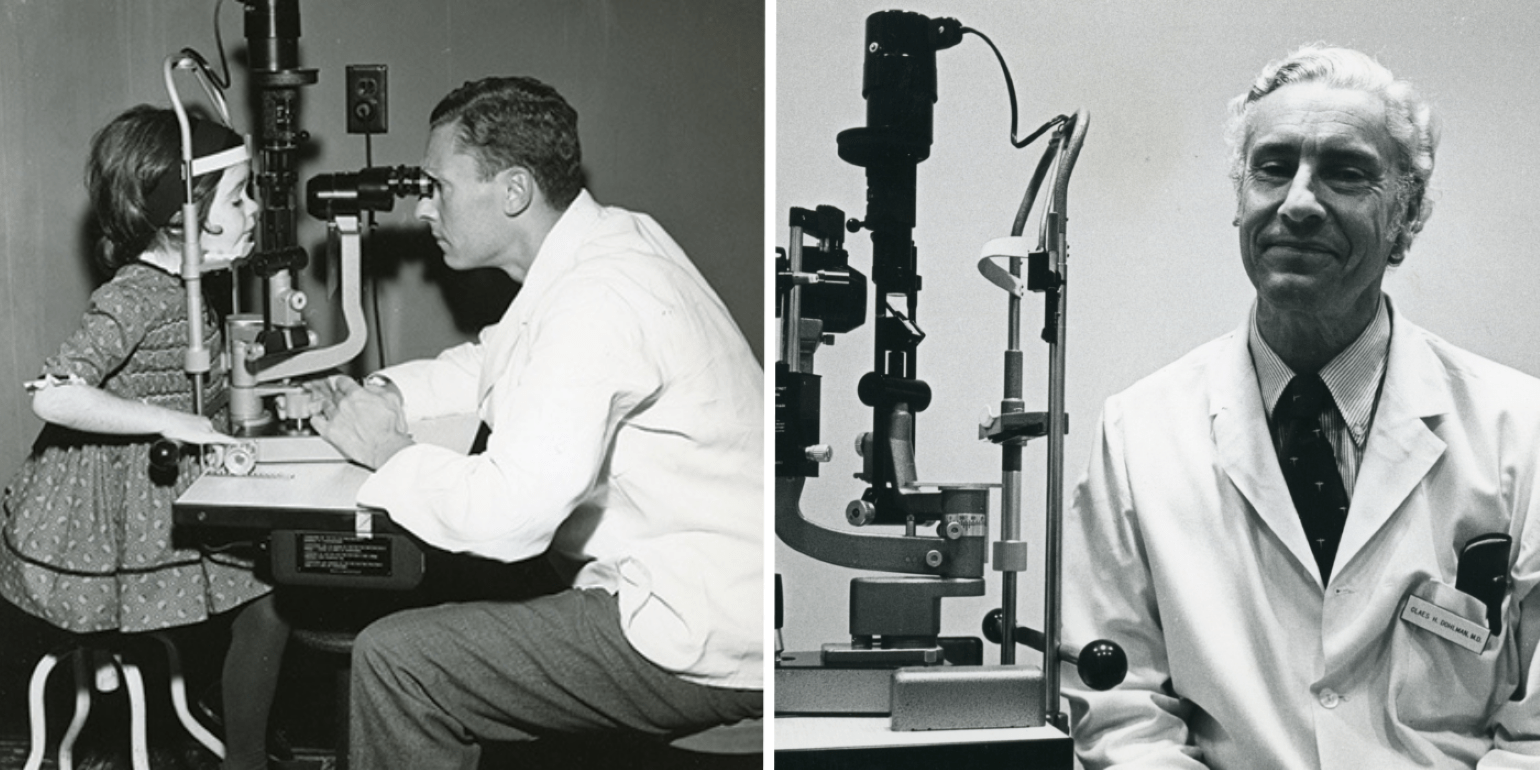
Figure 7
Dr. Claes Dohlman examining a pediatric patient in the 1950s (left) and in an undated photo in the cornea clinic (right).
In a career that now spans seven decades, Claes Dohlman, MD, PhD, is widely known as the father of modern corneal science. In 1958, Dr. Dohlman joined Mass Eye and Ear, where he later founded the Cornea Service—the first cornea subspecialty clinic in the world—and the first-ever Cornea Fellowship. Under Dr. Dohlman’s leadership, the Cornea Service has grown to be one of the largest and most renowned in the world. Our translational cornea research has led to new treatments for a range of corneal disorders, including stem cell transplantation for ocular surface reconstruction and the Boston Keratoprosthesis.
First developed by Dr. Dohlman in 1965, the Boston Keratoprosthesis (Boston KPro) was approved by the Food and Drug Administration in 1992 and is still the most widely used and successful artificial cornea to date. Today, clinician scientists at Mass Eye and Ear, led by Eleftherios Paschalis, PhD, and Thomas H. Dohlman, MD, work to further advance this technology, including the development of the ‘Lucia’ type I keratoprosthesis, which offers improved cosmetic appearance for patients.
50 Years of Proton Beam Irradiation
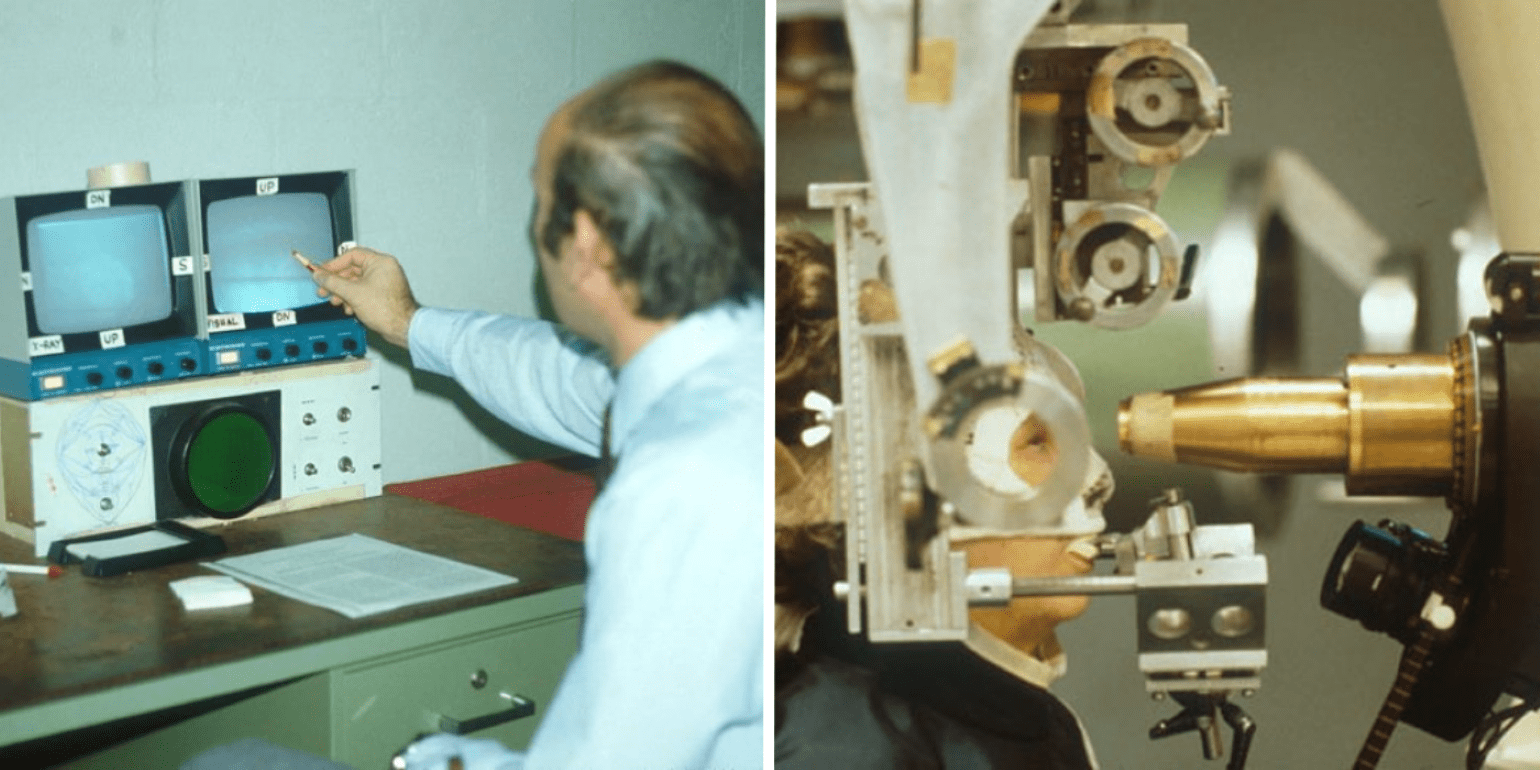
Figure 8
Dr. Evangelos Gragoudas monitoring a patient’s eye position during radiation treatment at the Harvard Cyclotron (left), and a patient seated in front of the proton beam collimator awaiting treatment (right).
Developed in 1975 by Evangelos Gragoudas, MD, proton beam irradiation (PBI) is a focused form of radiation that is particularly effective for treating tumors near critical parts of the eye. The therapy delivers a precise beam of radiation to the tumor, thereby limiting damage to the surrounding healthy tissues.
Under the mentorship of Dr. Schepens, Dr. Gragoudas began work on proton beam irradiation as an alternative to enucleation for choroidal melanoma. Nearly 50 years of follow-up studies show that PBI has the lowest local recurrence rate of any radiation therapy and is currently one of the most effective therapies for treating intraocular tumors.
25 Years of Photodynamic Therapy
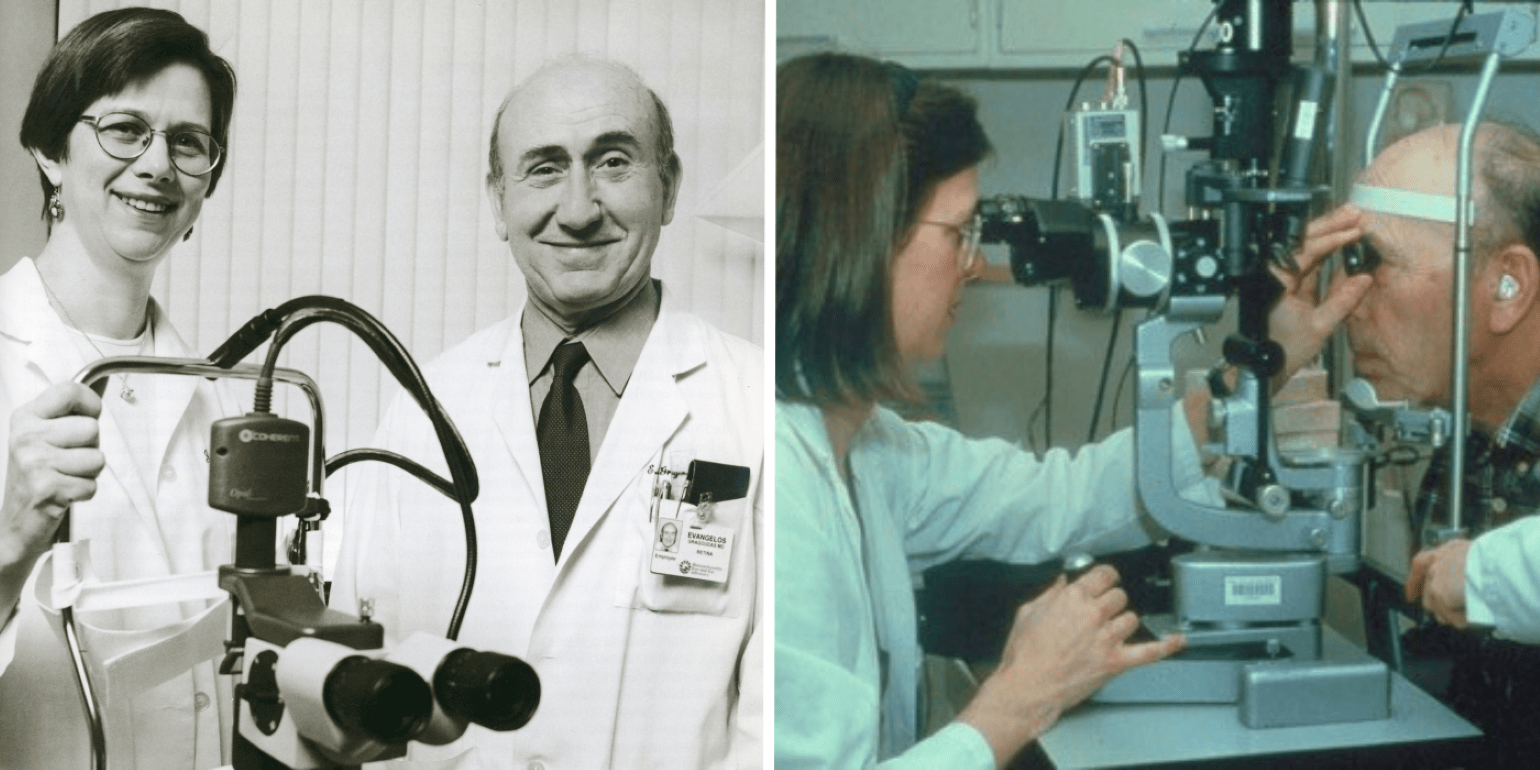
Figure 9
Drs. Joan W. Miller and Evangelos Gragoudas in 1999 with the PDT laser used in clinical trials (left), and Dr. Miller treating a patient with verteporfin PDT (right).
Evangelos Gragoudas, MD, and Joan W. Miller, MD, both internationally recognized experts on retinal disorders, pioneered preclinical and clinical studies for the use of photodynamic therapy using the laser-activated dye verteporfin for the treatment of choroidal neovascularization in patients with age-related macular degeneration (AMD). Based on these Mass Eye and Ear studies, photodynamic therapy using verteporfin (Visudyne®) became the first approved pharmacologic therapy to treat neovascular retinal disease and reduce and slow vision loss in patients with AMD.
25 years of Anti-VEGF Treatment for Retinal Disorders
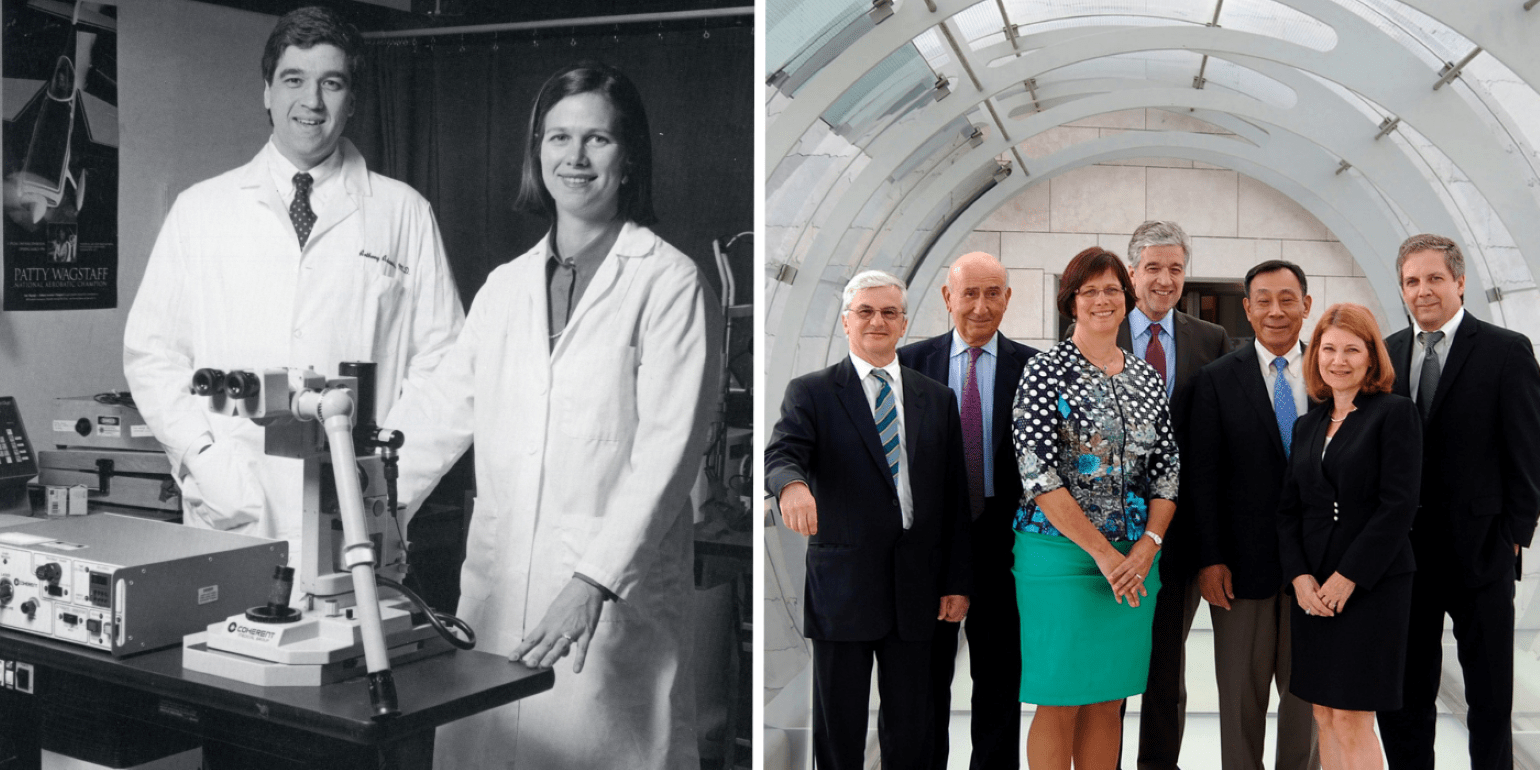
Figure 10
Drs. Joan W. Miller and Anthony Adamis in the laboratory at Mass Eye and Ear (left), and winners of the 2014 Antonio Champalimaud Award Vision Award for the development of anti-VEGF drugs (right).
In the 1990s, Mass Eye and Ear researchers Joan W. Miller, MD; Anthony Adamis, MD; Evangelos S. Gragoudas, MD; and Patricia A. D’Amore, PhD, MBA, worked in collaboration with Joslin Diabetes Center researchers Lloyd Paul Aiello, MD, PhD, and George King, PhD, also of Harvard Ophthalmology, along with Napoleone Ferrara, MD, of the University of California, San Diego (formerly Genentech), to identify vascular endothelial growth factor (VEGF) as the key driver of angiogenesis in the eye. Angiogenesis underlies the pathology of various blinding retinal disorders, including AMD and diabetic retinopathy. The researchers demonstrated that blocking VEGF could suppress ocular angiogenesis, leading to the development of anti-VEGF therapies for patients.
This biomedical breakthrough led to a new class of ophthalmic anti-VEGF drugs, which first became available in the United States in 2003 with the introduction of pegaptanib (Macugen®) for neovascular AMD. There are now numerous approved anti-VEGF drugs, and millions of people receive anti-VEGF injections annually around the world.
In recognition of their transformational clinical research, the team was awarded the 2014 António Champalimaud Vision Award, the highest distinction in ophthalmology and visual science.
25 years of Optical Coherence Tomography
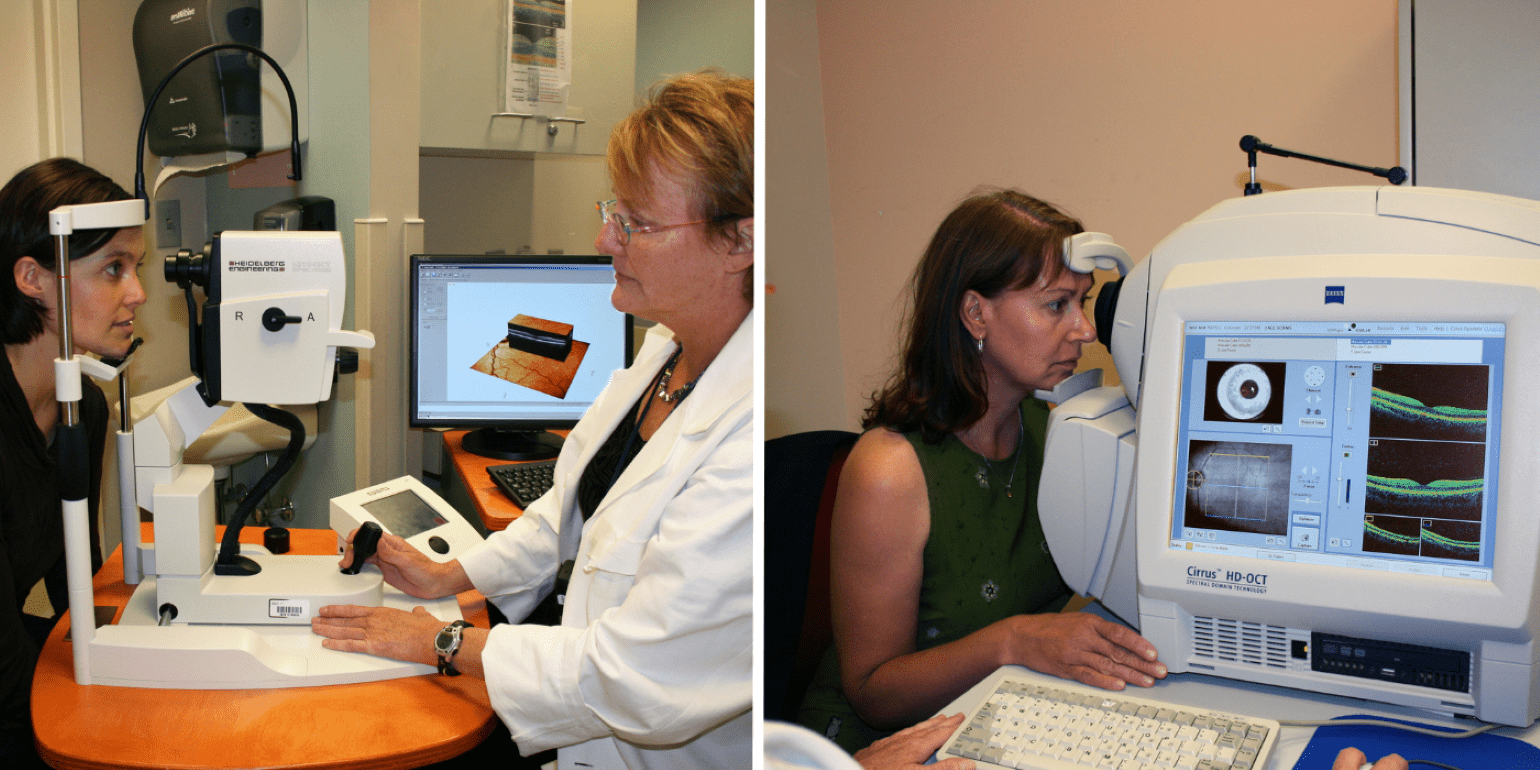
Figure 11
Two early OCT machines in use at Mass Eye and Ear in 2008, the Heidelberg Engineering SPECTRALIS (left) and the ZEISS CIRRUS OCT (right).
Researchers at Mass Eye and Ear, Mass General Hospital, and MIT co-discovered optical coherence tomography (OCT), the most widely used non-invasive imaging tool in retina care. David Huang, MD, PhD, was a graduate student at Harvard Medical School/MIT Health Sciences and Technology program, working at Mass Eye and Ear when he published his first paper on OCT with co-inventors James Fujimoto, SM, PhD, and Eric Swanson, SM, and former Mass Eye and Ear researcher Joel Schuman, MD. The group received the 2012 António Champalimaud Vision Award and David Huang received the 2023 Lasker Award for their work.
The development of OCT imaging completely revolutionized ophthalmic care by allowing clinicians to rapidly detect and then treat retinal diseases. As OCT imaging technology has advanced, it has become increasingly utilized for a range of eye disorders including age-related macular degeneration, diabetic retinopathy, retinal vein occlusions, and uveitis, among others.
Excellence in Education
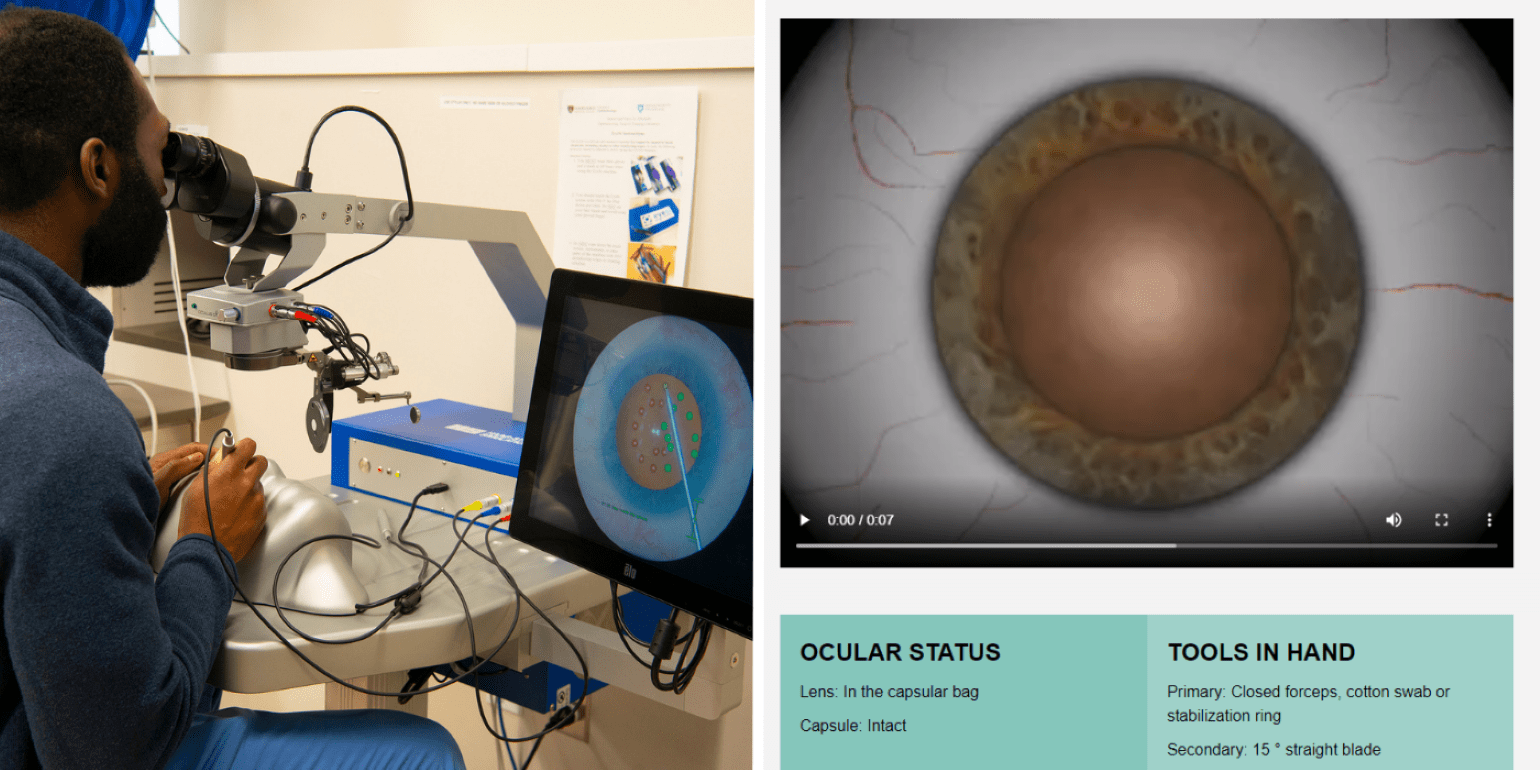
Figure 12
Ophthalmology Resident Dennis Akrobetu, MD, testing out the upgraded EYESI Surgical Simulator tool in the Samuel and Nancy Jo Altschuler Ophthalmology Surgical Training Laboratory (left), and a view of the digital Cataract Master surgical training tool (right).
Mass Eye and Ear is the primary teaching hospital of Harvard Ophthalmology, led by Chair Joan W. Miller, MD. Medical students, residents, and fellows receive world-class training in comprehensive ophthalmology and all the ophthalmic subspecialties, and students and post-doctoral fellows receive training in our internationally renowned laboratories. Harvard Ophthalmology prides itself on training the next generation of ophthalmology and vision research leaders, and about 1 in 5 current Ophthalmology Department Chairs in the U.S. and Canada are alumni.
The department leads the nation in developing an innovative and challenging cataract curriculum for ophthalmology residents. In 2005, the department launched the first national cataract surgery course, which is now held annually at Mass Eye and Ear. In 2009, the department implemented the Stepwise cataract surgery curriculum that emphasizes gradual, hands-on training. In 2012, former faculty members John I. Loewenstein, MD, and Bonnie An Henderson, MD, created the Cataract Master, a digital cataract surgical training tool that is now available nationally to American Academy of Ophthalmology members. The department also hosts an annual vitrectomy course for first-year retina fellows and a biennial orbital dissection course for ophthalmic plastic surgery fellows.
In 2017, Mass Eye and Ear established the Samuel and Nancy Jo Altschuler Ophthalmology Surgical Training Laboratory thanks to the generous gift of the Altschuler family honoring Lucy Young, MD, PhD. The facility features state-of-the-art surgical training equipment that allows Harvard Ophthalmology residents, Mass Eye and Ear fellows, and practicing surgeons to refine their surgical skills in a realistic preoperative environment. An early adopter of the EYESI Surgical Simulator tool, Mass Eye and Ear was one of the first institutions in the country to receive the upgraded EYESI tool in 2023.

Figure 13
Mass Eye and Ear faculty member Dr. Nimesh Patel teaching a retina fellow at the annual Vitrectomy Course (left) and faculty, trainees, and alumni at the Harvard Ophthalmology Alumni Reception at the 2023 Association for Research in Vision and Ophthalmology Annual Meeting in New Orleans (right).
Harvard Ophthalmology/Mass Eye and Ear boasts an engaged and diverse alumni community. In 2010, the Harvard Ophthalmology Alumni Association was founded and is currently led by Joseph Rizzo III, MD, and Joseph Ciolino, MD. Mass Eye and Ear’s Alumni Association nurtures relationships with former clinical and research trainees, whose support continues to strengthen our training programs.
In June 2010, the department expanded its Annual Meeting event to include an Alumni Reunion program. The Alumni Association now hosts several other annual events at key professional meetings, including the American Academy of Ophthalmology and Association for Research in Vision and Ophthalmology Annual Meetings.
Lucien Howe Library of Ophthalmology and Frederick A. Jakobiec, MD, DSc, Education and Information Center
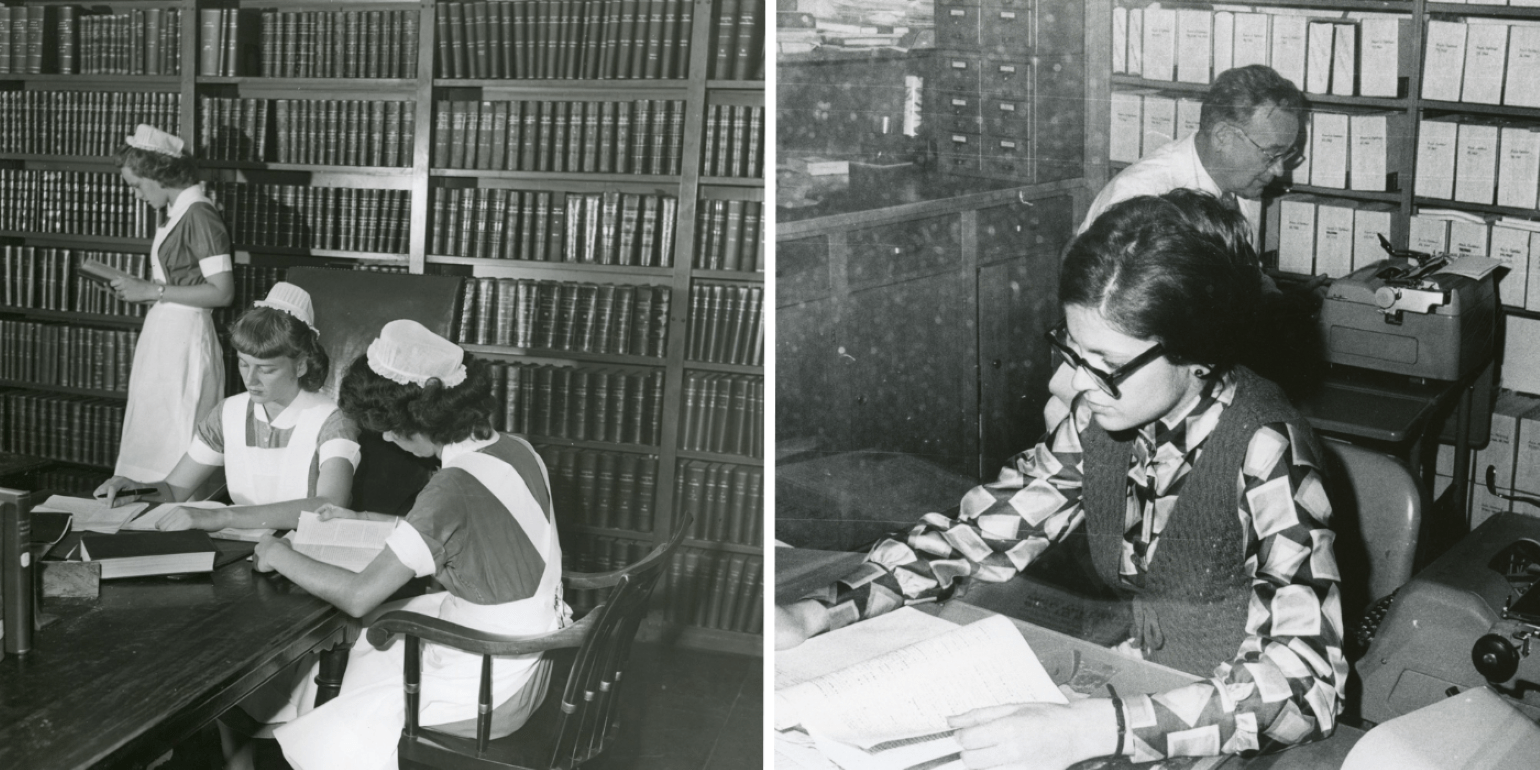
Figure 14
Nurses conducting research in the Howe Library in the 1950s (left) and long-time Mass Eye and Ear librarian Charles Snyder working in the Howe Library with colleague Susan Flanders in 1970 (right).
For nearly 150 years, the Libraries of Mass Eye and Ear have provided the highest quality of information resources and services available for evidence-based decision making for patient care and research. The original Mass Eye and Ear library was established in 1876, and in 1926, when the Lucien Howe Library of Ophthalmology at Mass Eye and Ear was founded, the two libraries merged.
In 1986, the library moved into its new space on the third floor of 243 Charles Street, where it remains today. At that time, the library was equipped with public-access computers and the hospital's first fax machine. To reflect the funding that built the new library, the name was changed to The Libraries of the Massachusetts Eye and Ear Infirmary: The Lucien Howe Library of Ophthalmology, The Leroy A. Schall Library of Otolaryngology, and the Abraham Pollen Archives and Rare Book Library.
In 2019, the late Frederick A. Jakobiec, MD, DSc, made a bequest of $1 million to support renovations and improvements to the library, now known as the Frederick A. Jakobiec, MD, DSc, Education and Information Center. A lifelong learner and devoted educator, Dr. Jakobiec was former chair of Harvard Ophthalmology and former chief of Ophthalmology at Mass Eye and Ear.
Ophthalmology Research Laboratories
Mass Eye and Ear is the flagship research and teaching hospital of Harvard Ophthalmology, and the department unites researchers from three historical laboratories: the Howe Laboratory, Schepens Eye Research Institute of Mass Eye and Ear, and the Berman-Gund Laboratory for the Study of Retinal Degenerations. Each laboratory will be highlighted individually later this year as part of the 200th Anniversary celebration, but below is a brief overview.
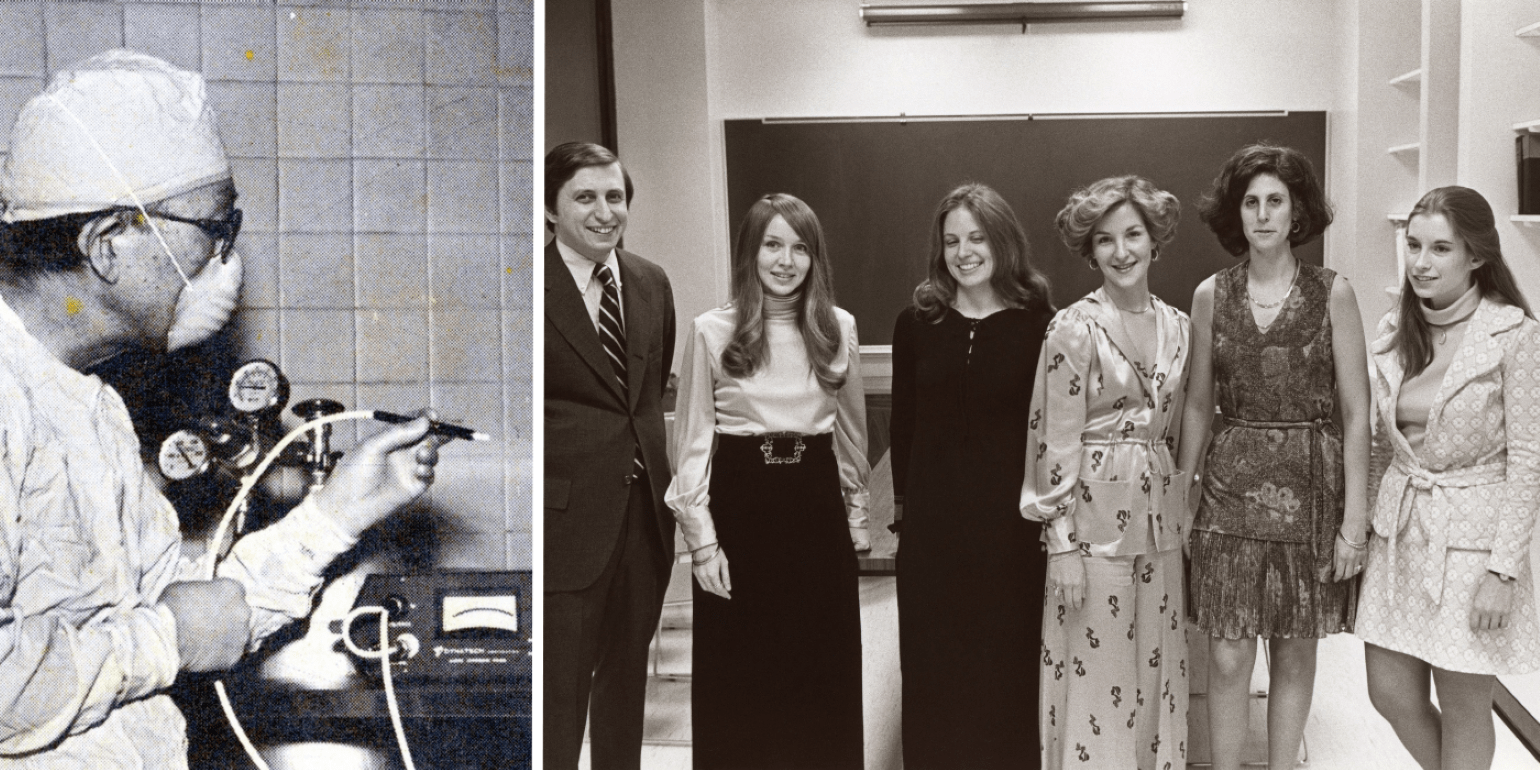
Figure 15
Ichiro Okamura, MD, using a cold probe at Schepens Eye Research Institute in the 1960s (left), Eliot L. Berson, MD, with laboratory members at the Berman-Gund Laboratory dedication in 1974 (right).
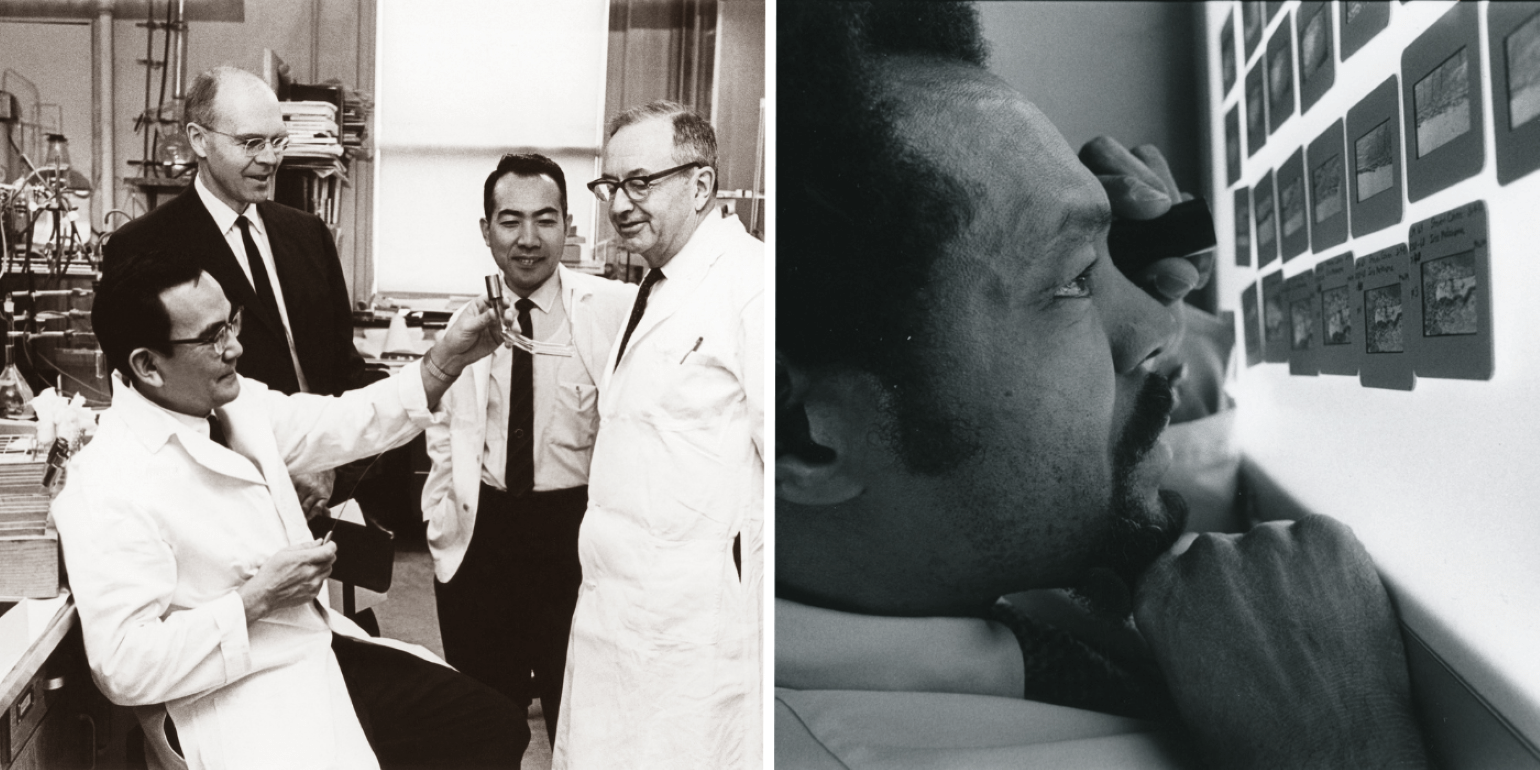
Figure 16
Howe Laboratory researchers Jin Kinoshita, PhD; W. Morton Grant, MD; Toichiro Kuwabara, MD, PhD; and David G. Cogan, MD, in 1969 (left), and Thomas Richardson, MD, a glaucoma specialist and Howe Laboratory researcher, viewing slides in 1980 (right).
Howe Laboratory
The Howe Laboratory, established in 1926, was the first endowed ophthalmology research laboratory in the United States and was initially led by pathologist and researcher Frederick H. Verhoeff, MD. David G. Cogan, MD, directed the laboratory from 1940 to 1974, and it became a hub for translational research.
As the need for pathology grew, Mass Eye and Ear formed a separate pathology laboratory dedicated to the histopathologic diagnosis of ocular conditions. In 1989, the late Frederick A. Jakobiec, MD, DSc, an international leader in eye pathology, joined Mass Eye and Ear as chief of Ophthalmology. After stepping down from leading the department, Dr. Jakobiec transitioned to directing the pathology laboratory, now known as the David G. Cogan Laboratory of Ophthalmic Pathology, and resumed his prolific research efforts and teaching of residents, fellows, and faculty. Dr. Jakobiec bequeathed a $4.5 million gift to Mass Eye and Ear to support four named endowments, including the Frederick A. Jakobiec Directorship of the David G. Cogan Laboratory of Ophthalmic Pathology. Today, in addition to serving as a regional and national diagnostic center, the laboratory continues to be an integral part of training physicians and researchers in eye pathology.
Berman-Gund Laboratory for the Study of Retinal Degenerations
Founded in 1974 under the leadership of the late Eliot L. Berson, MD, and established by philanthropists Gordon Gund and Bernard Berman and supported by the Foundation Fighting Blindness, the Berman-Gund Laboratory for the Study of Retinal Degenerations conducts multidisciplinary research on these disorders. Dr. Berson’s research within the laboratory laid the foundation for our current understanding of retinitis pigmentosa. Dr. Berson and colleague Thaddeus (Ted) Dryja, MD, identified 16 different genes responsible for retinitis pigmentosa and other forms of retinal degeneration and retinal dysfunction. To date, its researchers have helped discover more than 20 of the genes which harbor mutations that cause these disorders and are currently exploring new methods of treatment including gene augmentation therapy.
Schepens Eye Research Institute of Mass Eye and Ear
Originally called the Retina Foundation, Schepens Eye Research Institute of Mass Eye and Ear was founded in 1950 by pioneering retinal surgeon Charles Schepens, MD. In 2011, Mass Eye and Ear joined forces with Schepens Eye Research Institute to create the world’s largest and most robust basic and clinical ophthalmology research enterprise. This collaboration is working to translate bench-to-bedside research into better treatments and new cures for blinding diseases.
Today, Schepens Eye Research Institute and the Howe Laboratory are led by Patricia D’Amore, PhD, MBA, who plays a vital role in shaping research goals, overseeing faculty development, and building collaborative relationships. These storied laboratories are an important part of Mass Eye and Ear’s research history and future, although our current ophthalmology research efforts are organized around multidisciplinary Centers of Excellence and Institutes, rather than the historic laboratories, to allow clinicians, educators, investigators, trainees, and laboratories to come together to focus on a specific ophthalmic disorder or scientific discipline.
Women in Ophthalmology: A History of Firsts
Since the late 1800s, women have been at the heart of Mass Eye Ear, but like many medical institutions of the time, women initially held nursing and administrative roles. Maud Carvill, MD, was the first woman on the surgical staff at Mass Eye and Ear when she was appointed in 1921, followed by Edith Ives Cogan, MD. But social changes in the 1960s created more opportunities for women.
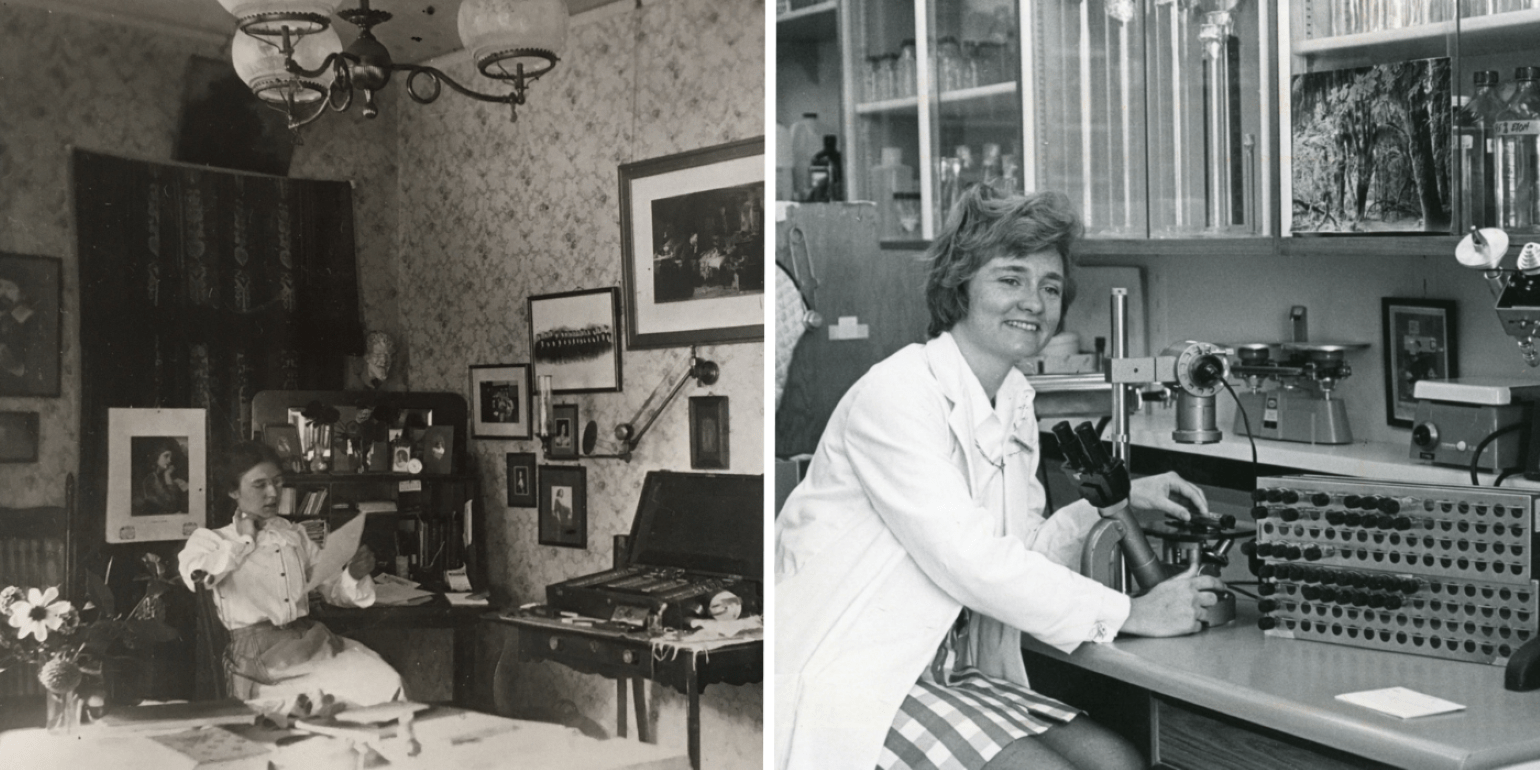
Figure 17
Edith Ives Cogan, MD, working at home (left), and Deborah Pavan-Langston, MD, in the laboratory in 1971 (right).
In 1959, Alice McPherson, MD, was the first woman in the U.S. to complete a retina fellowship and did so under the mentorship of Charles L. Schepens, MD— the “Father of Modern Retinal Surgery”—at Mass Eye and Ear. She went on to become the first full-time woman vitreoretinal surgeon in the world and a towering figure in the field of retina.
In 1966, Deborah Pavan-Langston, MD, became the first woman to be accepted into the Mass Eye and Ear (now Harvard) Ophthalmology Residency Training Program and the first woman to complete a Cornea Fellowship at Mass Eye and Ear. And in 1973, she became the first woman to direct the Cornea Service at Mass Eye and Ear.
Under the leadership of the late Frederick Jakobiec, MD, DSc, chief of Ophthalmology from 1989-2002, the number of women ophthalmologists continued to grow, setting the stage for a history of firsts for women in ophthalmology at Mass Eye and Ear.
In 1990, the late Mariana Dieste Mead, MD, was the first woman selected to serve as chief resident in Ophthalmology at Mass Eye and Ear.
In 1997, Ilene Gipson, PhD, a senior scientist at Mass Eye and Ear, became the first woman to be promoted to professor of Ophthalmology at Harvard Medical School.
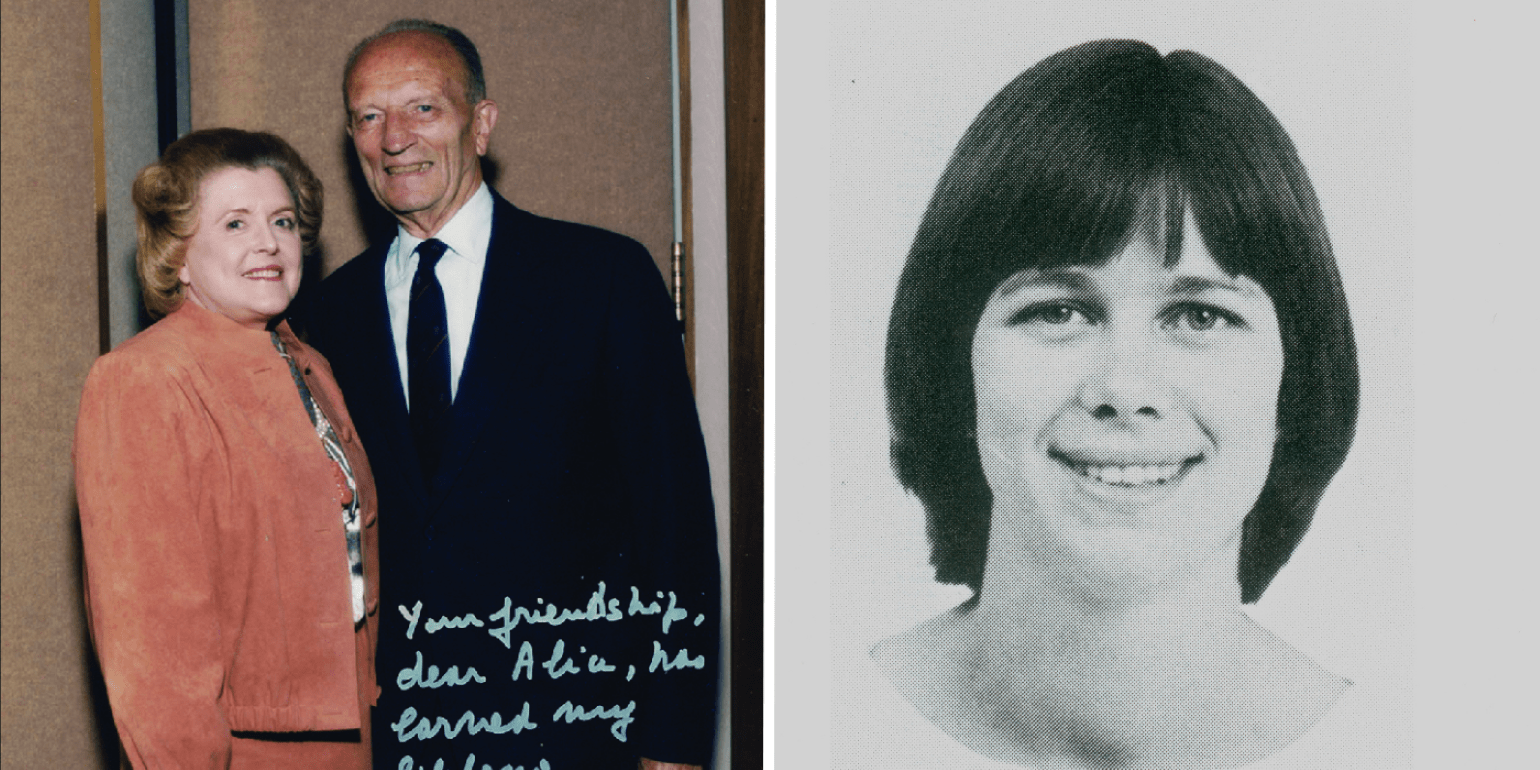
Figure 18
Alice McPherson, MD, with her mentor, Charles Schepens, MD (left), and future Department Chair Joan W. Miller, MD, during her residency training at Mass Eye and Ear (right).
In 2002, Joan W. Miller, MD, became the first woman physician to achieve the rank of professor of Ophthalmology at Harvard Medical School, and in 2003 she became the first woman appointed chief of Ophthalmology at Mass Eye and Ear and chair of Ophthalmology at Harvard Medical School. Among her many awards and accolades, Dr. Miller was the first person to receive all three highly esteemed awards—the Charles L. Schepens, MD/American Academy of Ophthalmology Award, the Gertrude D. Pyron Award of the Retina Research Foundation, and the Lucien Howe Medal from the American Ophthalmological Society. And in 2015, she became the first woman to receive the Mildred Weisenfeld Award for Excellence in Ophthalmology from the Association for Research in Vision and Ophthalmology. Learn more about women in ophthalmology at Mass Eye and Ear.
Looking to the Future
As we celebrate 200 years of exceptional patient care, transformational research, world-class education, and community service, our legacy continues to propel us forward. From a humble one-room clinic in Boston to a leading institution of Harvard Ophthalmology, we are constantly evolving, yet remain steadfast in our mission to eradicate blindness and provide premier patient care, while training the next generation of leaders in the field. This bicentennial celebration marks not an end, but a promise—a promise of more cures for our patients, more lives touched, and more hope kindled, as we embark on the next chapter of our enduring mission.
We are focused on providing clinical innovations and care to areas where the greatest unmet needs still exist, including retinal degenerations, macular degenerations, diabetic eye disease, and optic neuropathies, particularly glaucoma. Our other important clinical program areas include the cornea and ocular surface, oncology, immunology, infectious disease, and vision rehabilitation. As technology continues to advance, we are also pursuing a range of promising new research areas, including artificial intelligence, big data, genetics and gene-based therapy, imaging, and other diagnostic technologies.
Our 200th anniversary celebrations will continue with more exciting stories, events, and exhibits. The special Mass Eye and Ear exhibit at the Russell Museum of Medical History and Innovation will open this spring, and on June 13-14, 2024, Harvard Ophthalmology will hosts an expanded Annual Meeting and Alumni Reunion to celebrate Mass Eye and Ear and its illustrious alumni with awardees Deborah Jacobs, MD, MS; Reza Dana, MD, MSc, MPH; Julia Haller, MD; and David Guyer, MD, and honor Evangelos S. Gragoudas, MD, for 50 years with Mass Eye and Ear.
Learn more about research in Ophthalmology at Mass Eye and Ear/Mass General
Refer a patient to Mass Eye and Ear/Mass General