What We Have Learned About COVID-19: Part One
The FLARE Four
- In the months since the first cases of COVID-19 were reported, an astounding amount of research (of varying quality) has been published
- Despite early confusion, there is now substantial consensus on optimal treatment of the critically ill patient with COVID-19. This is based on established evidence for pre-COVID-19 ARDS as well as data from new randomized controlled trials
- Several early hypotheses that gained widespread attention have been refuted by subsequent investigation
- Critical questions remain, but we now have a solid foundation, including two new drug treatments, with which to establish a standard of care. Moreover, with many ongoing trials, we can look forward to additional high-quality evidence in the near future
Subscribe to the latest updates from FLARE Advances in Motion
Many people are asking...What have we learned about COVID-19?
Since the initial outbreak of COVID-19, clinicians have treated hundreds of thousands of patients. At the same time, over 55,000 COVID-related research articles have been published (albeit of heterogeneous quality). Much has been learned. It is also unfortunately true that questionable findings have been amplified by the lay press (Savel et al. 2020) and a great deal of misinformation was spread. This has resulted in variable clinical practice and even conflicting expert guidelines (Marini and Gattinoni 2020; Alhazzani et al. 2020).
COVID-19 Phenotypes: Severe COVID-19 Is ARDS
COVID-19 in its most severe form causes acute respiratory distress syndrome (ARDS). A central problem in ARDS is the inherent heterogeneity of the disease (Bellani et al. 2016). The Berlin definition (ARDS Definition Task Force et al. 2012) applies to patients that vary considerably in their degree of hypoxemia, respiratory system mechanics and prognosis. For this reason, there has been a longstanding interest in defining sub-phenotypes of ARDS (Prescott et al. 2016). Despite much high-quality work (Calfee et al. 2014; Famous et al. 2017), prior to COVID-19, no scheme for sub-phenotyping had prospectively demonstrated the ability to improve treatment response. This is key because, broad as it is, the Berlin definition and its like serve as the inclusion criteria for the large RCTs used to establish the standard of care in ARDS. In other words, heterogeneity is real but evidence-based ARDS care provided without regard to heterogeneity reduces mortality. In this setting, the standard for adoption of a particular sub-phenotyping scheme must have a prospectively demonstrated ability to improve outcomes (Bos, Sinha and Dickson 2020). The mere demonstration of heterogeneous presentations among the overall ARDS population is not new (Panwar et al. 2020) and is not sufficient to establish the validity of a classification scheme.
Nevertheless, there is continued and appropriate interest in sub-phenotyping. Given the novelty of SARS-CoV-2, it is fair to ask if the resulting disease has novel features. Some early reports argued that SARS-CoV-2 infection results in a unique clinical pathology (Gattinoni et al. 2020) and therefore evidence-based treatment protocols developed for other causes of respiratory failure may not apply to COVID-19 (Toy and Maremont 2020). We now have a number of published case series on COVID-19 that demonstrate internal uniformity and similarity to prior ARDS cohorts. Table 1 lists several observational series describing the North American experience of COVID-19. These reports document the near-universal presence of impaired gas exchange (ratio of partial pressure of arterial oxygen to fraction of inspired oxygen, P:F < 200) and bilateral pulmonary infiltrates in critically ill COVID-19 patients. These are also the key diagnostic features of ARDS (ARDS Definition Task Force et al. 2012). Low respiratory system compliance, while not part of the diagnostic criteria for ARDS, is frequently seen in the syndrome and is also in COVID-19 as indicated in the table.
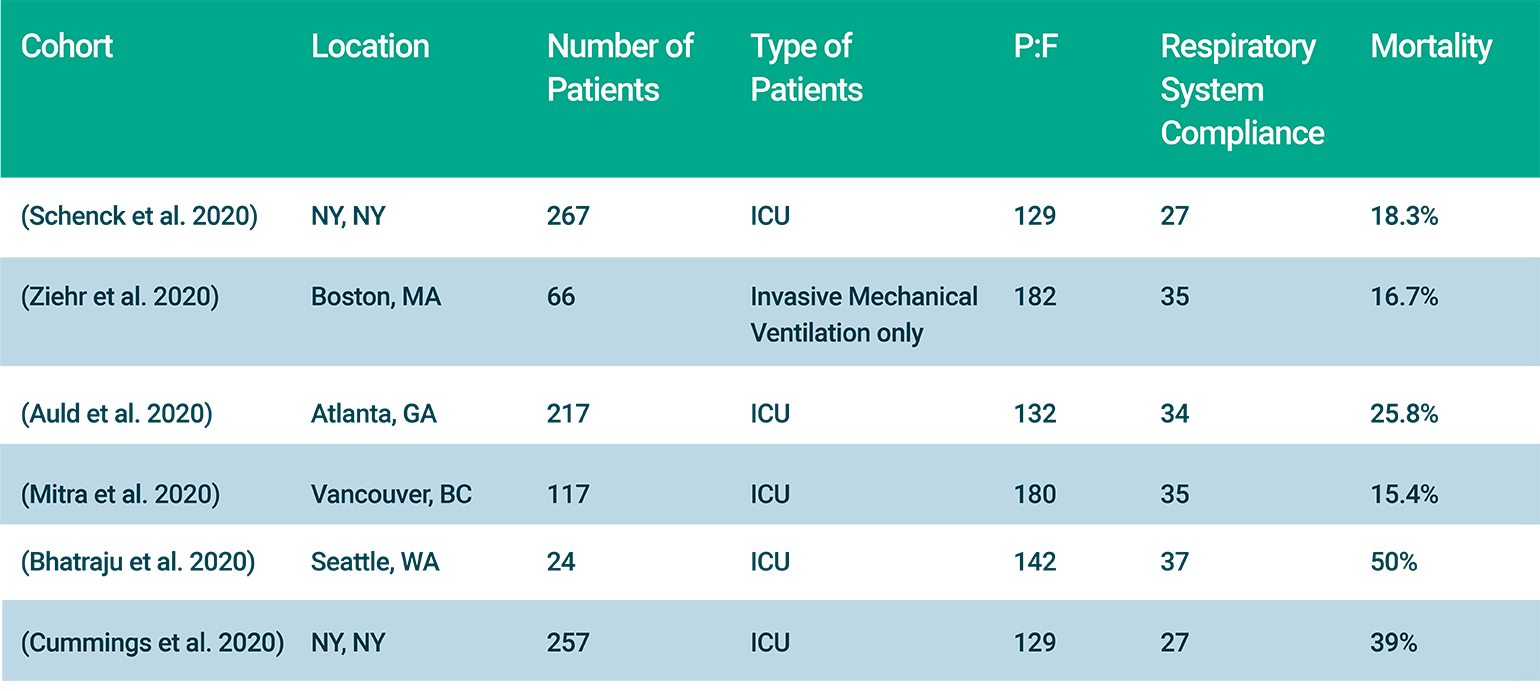
Table 1
Published observational cohorts in COVID-19 in North America.
There have also been a number of reports of post-mortem examinations in COVID-19 (Konopka et al. 2020; Barton et al. 2020; Tian et al. 2020; Carsana et al. 2020) reviewed in a prior FLARE. What these reports have in common is widespread observation of diffuse alveolar damage—the pathologic correlate of ARDS. Despite persistent arguments to the contrary, the peer-reviewed literature on COVID-19 is clear—it is characterized clinically by hypoxemia and bilateral infiltrates, pathologically by diffuse alveolar damage and is optimally treated by a strategy that minimizes distending pressure and lung stretch. On this basis, severe COVID-19 is ARDS and should be treated with the best established evidence-based protocols as applied to other causes of ARDS (low tidal volume ventilation, prone ventilation and conservative fluid management).
Mechanical Ventilation: Still Saving Lives
There exists a widespread impression in the lay press that mechanical ventilation in the setting of COVID-19 leads inevitably to death (examples here, here and here.) A major contributor to this inaccurate impression was a report from Northwell Health in New York published late April in JAMA (Richardson et al. 2020). The Northwell report received substantial media attention for its claim of mortality of 88% among ventilated patients. This claim was later corrected to indicate that mortality figures were determined by reporting only on those patients who had reached a definitive outcome (death or discharge) during the relatively short follow-up period of the study (average of ~4 days) and excluding the 53.8% of patients who remained alive and ventilated at the time of publication. Depending on the fate of the excluded patients, true mortality in the Northwell cohort could have been as low as 25% or as high as 97%—too broad to meaningfully inform clinical decisions. Fortunately, since that time, case series with more accurate 28-day mortality have become available (see Table 1) and report uncorrected mortality ranging from 15% to 50%. This is broadly similar to outcomes from pre-COVID-19 ARDS (Bellani et al. 2016) and should provide yet more reassurance that severe COVID-19 behaves largely the same as ARDS in the pre-COVID-19 era.
Happy Hypoxia: Not Hypoxia and Not New
Early in the outbreak, some reported that patients with COVID-19 respiratory failure were presenting with hypoxemia that is out of proportion to the degree of dyspnea—a phenomenon termed (incorrectly) "happy hypoxia." To the extent that this is a real phenomenon (most reports were anecdotal), the observation of hypoxemia without dyspnea should not be surprising (Tobin, Laghi and Jubran 2020) and is not unique to COVID-19. Indeed, an argument may be made that the widespread attention paid to this issue was more a function of the number of non-specialist providers seeing COVID-19 patients than it was of the virus itself. Since that time, corrective literature (Tobin, Laghi and Jubran 2020), which explains the established principles of respiratory physiology (Banzett et al. 1996; Burki and Lee 2010; Lansing, Gracely and Banzett 2009; Harold L. Manning et al. 1992) behind this phenomenon, has emerged. Dyspnea has a complex relationship to hypoxemia, and hypoxemia alone is a weak stimulus for dyspnea (H. L. Manning and Schwartzstein 1995) We cover the physiology at length in a prior two-part FLARE.
Hydroxychloroquine: Not Recommended for the Treatment of COVID-19 of Any Severity
There now exists a large amount of literature on the use of hydroxychloroquine in COVID-19—the size of which is inversely related to the amount of evidence of benefit. We have covered the early reports and scientific rationale for use of hydroxychloroquine in prior FLARE's (March 22 and April 29). Since that time large studies have been published (Mehra et al. 2020) and retracted. The definitive study on the use of hydroxychloroquine, the Outcomes Related to COVID-19 Treated with Hydroxychloroquine among In-patients with Symptomatic Disease (ORCHID) trial, conducted by the NIH sponsored Prevention and Early Treatment of Lung Injury (PETAL) network, has been completed but has not yet been published. ORCHID was a rigorous multicenter, blinded, placebo-controlled randomized trial that enrolled 479 patients with laboratory-confirmed COVID-19. Patients received 5 days of hydroxychloroquine or placebo. The trial was stopped in June after the fourth scheduled interim analysis, based on futility. While we await publication for full analysis of this trial, we should note that there is no high-quality RCT evidence in favor of hydroxychloroquine and a good amount of evidence (Tang et al. 2020; Cavalcanti et al. 2020) against it. The evidence is conclusive enough that the Food and Drug Administration (FDA) has revoked its emergency use authorization for hydroxychloroquine in COVID-19.
Steroids: Recommended for Patients with Severe or Critical COVID-19
See also: FLARES from April 4 and June 27.
The release of results from the RECOVERY trial (RECOVERY Collaborative Group et al. 2020) changed the conversation around steroids and ARDS. The data on steroids in ARDS in the pre-COVID era were mixed. In fact, the LaSRS trial suggested an increase in mortality in patients who had >13 days of ARDS prior to receiving steroids (Steinberg et al. 2006; Villar et al. 2020). There was also a particular concern around the use of steroids for viral pneumonia based on observational data and meta-analysis that found an increase in mortality associated with steroid use for influenza (Zhang et al. 2015; Brun-Buisson et al. 2011).
In RECOVERY (RECOVERY Collaborative Group et al. 2020), 6,425 patients with COVID-19 were randomized to receive dexamethasone or usual care. Of note, this was not strictly an ARDS study as it included patients across the spectrum of COVID-19 requiring hospitalization. Patients receiving respiratory support (invasive mechanical ventilation or oxygen therapy) had a lower incidence of death with dexamethasone compared to the usual care group, whereas there was no clear effect in patients who received no respiratory support. While a subgroup analysis has some inherent problems and the control group for mechanical ventilation appears to have higher mortality (41.4%) than would be expected based on other COVID-19 cohorts (see Table 1 above), this data suggests there is a benefit to steroid use in COVID-19 patients receiving supplemental oxygen and/or mechanical ventilation. Based on the results from LaSRS (Steinberg et al. 2006), caution should be exercised while using this therapy > 13 days from the onset of ARDS.
Following these results, the WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group published a prospective meta-analysis to evaluate the efficacy of corticosteroids in critically ill patients with COVID-19 across 7 randomized clinical trials, including RECOVERY (WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group et al. 2020). Corticosteroids used in these studies included dexamethasone (3 trials, 1,282 patients), hydrocortisone (3 trials, 374 patients), and methylprednisolone (1 trial, 47 patients). Overall, the administration of corticosteroids was associated with lower all-cause mortality at 28 days after randomization, with an absolute mortality risk of 32% with corticosteroids, compared with 40% in usual care or placebo.
Based on these results, the WHO and CDC now both strongly recommend systemic steroids for up to 10 days in patients with severe and critical COVID-19 (requiring supplemental oxygen or mechanical ventilation) (Organization and Others 2020). In all, there is now widespread consensus that steroid therapy is these patients should be considered to be standard of care.
Remdesivir: Recommended for Patients Requiring Oxygen but Not Ventilatory Support
Remdesivir is a nucleoside analog that inhibits the RNA-dependent RNA polymerase of SARS-CoV-2. We reviewed the arm of the Adaptive COVID-19 Treatment Trial-1 (ACTT-1) dealing with remdesivir (Beigel et al. 2020) on May 26, which showed a significant benefit in terms of earlier recovery in patients requiring oxygen, but not in patients receiving HFNC or NIPPV, mechanical ventilation or ECMO. The results from this trial resulted in an emergency use authorization by the FDA for remdesivir (Beigel et al. 2020). Another randomized clinical trial of 584 patients with moderate COVID-19 (radiographic evidence of infiltrates and oxygen saturation >94% on room air) that was run concurrently with the ACTT-1 study also found statistically significant better clinical status in patients who received 5 or 10 days of remdesivir compared to standard care, up to 28 days after beginning treatment (Spinner et al. 2020).
Based on these results, NIH treatment guidelines currently recommend the use of remdesivir for patients receiving oxygen but not HFNC, NIPPV, mechanical ventilation or ECMO. The guidelines do not recommend against remdesivir in patients requiring higher levels of support but note that supplies may be limited and since benefit has not been conclusively demonstrated in other groups it may make sense to prioritize. Institutions with adequate supplies have expanded inclusion criteria.
Conclusion
Nine months into the global pandemic due to SARS-CoV-2, much has been learned. In the early days of dealing with this novel pathogen, it was difficult to place the flood of new observations and publications in context. However, it is now possible to reflect on lessons learned and to develop a consensus, evidence-based approach to the care of COVID-19. The cornerstones of such an approach are the cornerstones of ARDS management—lung-protective ventilation, prone ventilation and conservative fluid management. In addition it is now possible to say unequivocally that patients with severe COVID-19 benefit from steroids and remdesivir.
There will be many challenges as we head into another potential surge—including the increasing burden of ICU survivorship (see May 20 FLARE)—but we also look forward to the results of RCTs and vaccine trials that promise to provide a rigorous evidence base for future alterations of treatment protocols. In our next FLARE, we will address the controversies that live on. These include some early hypotheses that initially gained widespread attention and continue to find their way into conversations on ICU ward rounds and on social media ("cytokine storm") as well as other areas of active investigation including convalescent plasma therapy and anticoagulation.
References
- Alhazzani, Waleed, Morten Hylander Møller, Yaseen M. Arabi, Mark Loeb, Michelle Ng Gong, Eddy Fan, Simon Oczkowski, et al. 2020. "Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19)." Intensive Care Medicine. 46 (5): 854–87.
- ARDS Definition Task Force, V. Marco Ranieri, Gordon D. Rubenfeld, B. Taylor Thompson, Niall D. Ferguson, Ellen Caldwell, Eddy Fan, Luigi Camporota, and Arthur S. Slutsky. 2012. "Acute Respiratory Distress Syndrome: The Berlin Definition." JAMA: The Journal of the American Medical Association. 307 (23): 2526–33.
- Auld, Sara C., Mark Caridi-Scheible, James M. Blum, Chad Robichaux, Colleen Kraft, Jesse T. Jacob, Craig S. Jabaley, et al. 2020. "ICU and Ventilator Mortality Among Critically Ill Adults With Coronavirus Disease 2019." Critical Care Medicine. May. https://doi.org/10.1097/CCM.0000000000004457.
- Barton, Lisa M., Eric J. Duval, Edana Stroberg, Subha Ghosh, and Sanjay Mukhopadhyay. 2020. "COVID-19 Autopsies, Oklahoma, USA." American Journal of Clinical Pathology. 153 (6): 725–33.
- Beigel, John H., Kay M. Tomashek, Lori E. Dodd, Aneesh K. Mehta, Barry S. Zingman, Andre C. Kalil, Elizabeth Hohmann, et al. 2020. "Remdesivir for the Treatment of Covid-19 - Preliminary Report." The New England Journal of Medicine. May. https://doi.org/10.1056/NEJMoa2007764.
- Bellani, Giacomo, John G. Laffey, Tài Pham, Eddy Fan, Laurent Brochard, Andres Esteban, Luciano Gattinoni, et al. 2016. "Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries." JAMA: The Journal of the American Medical Association. 315 (8): 788–800.
- Bhatraju, Pavan K., Bijan J. Ghassemieh, Michelle Nichols, Richard Kim, Keith R. Jerome, Arun K. Nalla, Alexander L. Greninger, et al. 2020. "Covid-19 in Critically Ill Patients in the Seattle Region - Case Series." The New England Journal of Medicine. 382 (21): 2012–22.
- Bos, Lieuwe D. J., Pratik Sinha, and Robert P. Dickson. 2020. "The Perils of Premature Phenotyping in COVID: A Call for Caution." The European Respiratory Journal: Official Journal of the European Society for Clinical Respiratory Physiology. June. https://doi.org/10.1183/13993003.01768-2020.
- Brun-Buisson, Christian, Jean-Christophe M. Richard, Alain Mercat, Anne C. M. Thiébaut, Laurent Brochard, and REVA-SRLF A/H1N1v 2009 Registry Group. 2011. "Early Corticosteroids in Severe Influenza A/H1N1 Pneumonia and Acute Respiratory Distress Syndrome." American Journal of Respiratory and Critical Care Medicine. 183 (9): 1200–1206.
- Calfee, Carolyn S., Kevin Delucchi, Polly E. Parsons, B. Taylor Thompson, Lorraine B. Ware, Michael A. Matthay, and NHLBI ARDS Network. 2014. "Subphenotypes in Acute Respiratory Distress Syndrome: Latent Class Analysis of Data from Two Randomised Controlled Trials." The Lancet. Respiratory Medicine. 2 (8): 611–20.Carsana, Luca, Aurelio Sonzogni, Ahmed Nasr, Roberta Simona Rossi, Alessandro Pellegrinelli, Pietro Zerbi, Roberto Rech, et al. 2020. "Pulmonary Post-Mortem Findings in a Series of COVID-19 Cases from Northern Italy: A Two-Centre Descriptive Study." The Lancet Infectious Diseases. June. https://doi.org/10.1016/S1473-3099(20)30434-5.
- Cummings, Matthew J., Matthew R. Baldwin, Darryl Abrams, Samuel D. Jacobson, Benjamin J. Meyer, Elizabeth M. Balough, Justin G. Aaron, et al. 2020. "Epidemiology, Clinical Course, and Outcomes of Critically Ill Adults with COVID-19 in New York City: A Prospective Cohort Study." The Lancet. May. https://doi.org/10.1016/S0140-6736(20)31189-2.
- Famous, Katie R., Kevin Delucchi, Lorraine B. Ware, Kirsten N. Kangelaris, Kathleen D. Liu, B. Taylor Thompson, Carolyn S. Calfee, and ARDS Network. 2017. "Acute Respiratory Distress Syndrome Subphenotypes Respond Differently to Randomized Fluid Management Strategy." American Journal of Respiratory and Critical Care Medicine. 195 (3): 331–38.
- Gattinoni, Luciano, Silvia Coppola, Massimo Cressoni, Mattia Busana, Sandra Rossi, and Davide Chiumello. 2020. "COVID-19 Does Not Lead to a 'Typical' Acute Respiratory Distress Syndrome." American Journal of Respiratory and Critical Care Medicine. 201 (10): 1299–1300.
- Konopka, Kristine E., Teresa Nguyen, Jeffrey M. Jentzen, Omar Rayes, Carl J. Schmidt, Allecia M. Wilson, Carol F. Farver, and Jeffrey L. Myers. 2020. "Diffuse Alveolar Damage (DAD) from Coronavirus Disease 2019 Infection Is Morphologically Indistinguishable from Other Causes of DAD." Histopathology. https://doi.org/10.1111/his.14180.
- Marini, John J., and Luciano Gattinoni. 2020. "Management of COVID-19 Respiratory Distress." JAMA: The Journal of the American Medical Association. April. https://doi.org/10.1001/jama.2020.6825.
- Mitra, Anish R., Nicholas A. Fergusson, Elisa Lloyd-Smith, Andrew Wormsbecker, Denise Foster, Andrei Karpov, Sarah Crowe, et al. 2020. "Baseline Characteristics and Outcomes of Patients with COVID-19 Admitted to Intensive Care Units in Vancouver, Canada: A Case Series." CMAJ: Canadian Medical Association Journal = Journal de l'Association Medicale Canadienne. May. https://doi.org/10.1503/cmaj.200794.
- Organization, World Health, and Others. 2020. "Corticosteroids for COVID-19: Living Guidance, 2 September 2020." World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/334125/WHO-2019-nCoV-Corticosteroids-2020.1-eng.pdf.
- Panwar, Rakshit, Fabiana Madotto, John G. Laffey, Frank M. P. Van Haren, and LUNG SAFE Investigators and the ESICM Trials Group. 2020. "Compliance Phenotypes in Early ARDS Before the COVID-19 Pandemic." American Journal of Respiratory and Critical Care Medicine. August. https://doi.org/10.1164/rccm.202005-2046OC.
- Prescott, Hallie C., Carolyn S. Calfee, B. Taylor Thompson, Derek C. Angus, and Vincent X. Liu. 2016. "Toward Smarter Lumping and Smarter Splitting: Rethinking Strategies for Sepsis and Acute Respiratory Distress Syndrome Clinical Trial Design." American Journal of Respiratory and Critical Care Medicine. 194 (2): 147–55.
- RECOVERY Collaborative Group, Peter Horby, Wei Shen Lim, Jonathan R. Emberson, Marion Mafham, Jennifer L. Bell, Louise Linsell, et al. 2020. "Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report." The New England Journal of Medicine. July. https://doi.org/10.1056/NEJMoa2021436.
- Richardson, Safiya, Jamie S. Hirsch, Mangala Narasimhan, James M. Crawford, Thomas McGinn, Karina W. Davidson, Douglas P. Barnaby, et al. 2020. "Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area." JAMA: The Journal of the American Medical Association. April. https://doi.org/10.1001/jama.2020.6775.
- Savel, Richard H., Ariel L. Shiloh, Paul C. Saunders, and Yizhak Kupfer. 2020. "Mechanical Ventilation During the Coronavirus Disease 2019 Pandemic: Combating the Tsunami of Misinformation From Mainstream and Social Media." Critical Care Medicine. June. https://doi.org/10.1097/CCM.0000000000004462.
- Schenck, Edward J., Katherine Hoffman, Parag Goyal, Justin Choi, Lisa Torres, Kapil Rajwani, Christopher W. Tam, Natalia Ivascu, Fernando J. Martinez, and David A. Berlin. 2020. "Respiratory Mechanics and Gas Exchange in COVID-19 Associated Respiratory Failure." Annals of the American Thoracic Society. May. https://doi.org/10.1513/AnnalsATS.202005-427RL.
- Steinberg, Kenneth P., Leonard D. Hudson, Richard B. Goodman, Catherine Lee Hough, Paul N. Lanken, Robert Hyzy, B. Taylor Thompson, Marek Ancukiewicz, and National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. 2006. "Efficacy and Safety of Corticosteroids for Persistent Acute Respiratory Distress Syndrome." The New England Journal of Medicine. 354 (16): 1671–84.
- Tian, Sufang, Yong Xiong, Huan Liu, Li Niu, Jianchun Guo, Meiyan Liao, and Shu-Yuan Xiao. 2020. "Pathological Study of the 2019 Novel Coronavirus Disease (COVID-19) through Postmortem Core Biopsies." Modern Pathology. https://doi.org/10.1038/s41379-020-0536-x.
- Toy, Sarah, and Mark Maremont. 2020. "Months Into Coronavirus Pandemic, ICU Doctors Are Split on Best Treatment." NEWSPLUS,PRO,WSJ-PRO-WSJ.com, July 1, 2020. https://www.wsj.com/articles/months-into-coronavirus-pandemic-icu-doctors-are-split-on-best-treatment-11593602756.
- Villar, J., C. Ferrando, D. Martinez, A. Ambros, T. Munoz, J. A. Soler, G. Aguilar, et al. 2020. "Dexamethasone Treatment for the Acute Respiratory Distress Syndrome: A Multicentre, Randomised Controlled Trial." Lancet Respir Med. 8 (3): 267–76.
- WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Jonathan A. C. Sterne, Srinivas Murthy, Janet V. Diaz, Arthur S. Slutsky, Jesús Villar, Derek C. Angus, et al. 2020. "Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-Analysis." JAMA: The Journal of the American Medical Association. September. https://doi.org/10.1001/jama.2020.17023.
- Zhang, Yi, Wenjie Sun, Erik R. Svendsen, Song Tang, Raina C. MacIntyre, Peng Yang, Daitao Zhang, and Quanyi Wang. 2015. "Do Corticosteroids Reduce the Mortality of Influenza A (H1N1) Infection? A Meta-Analysis." Critical Care / the Society of Critical Care Medicine. 19 (February): 46.
- Ziehr, David R., Jehan Alladina, Camille R. Petri, Jason H. Maley, Ari Moskowitz, Benjamin D. Medoff, Kathryn A. Hibbert, B. Taylor Thompson, and C. Corey Hardin. 2020. "Respiratory Pathophysiology of Mechanically Ventilated Patients with COVID-19: A Cohort Study." American Journal of Respiratory and Critical Care Medicine. April. https://doi.org/10.1164/rccm.202004-1163LE.
View all COVID-19 updates
Learn more about research in the Division of Pulmonary and Critical Care Medicine